Borderline personality disorder was added to American psychiatry’s official lexicon with the publication of DSM-III in 1980, classified on axis II in the diagnostic manual’s new multiaxial system. The decision to classify personality disorders on a separate axis derived from the widely shared belief, persisting into the 1980s, that these disorders were psychogenic, caused during early development by parental neglect, abuse, or inconstancy. Patients with borderline personality disorder were described as showing “social contrariness” and as “consistently using others for one’s own ends” (DSM-III, p. 322). A prototypic image of a borderline personality disorder patient emerged within clinical settings as an angry, volatile patient prone to reject help, blame others, and behave self-destructively. Too often, this behavior was seen as willfully oppositional, and borderline personality disorder patients were spoken of as dreaded pariahs. Recommended treatment was generally psychodynamic psychotherapy or psychoanalysis, often referred to as “heroic” and of uncertain or poor prognosis.
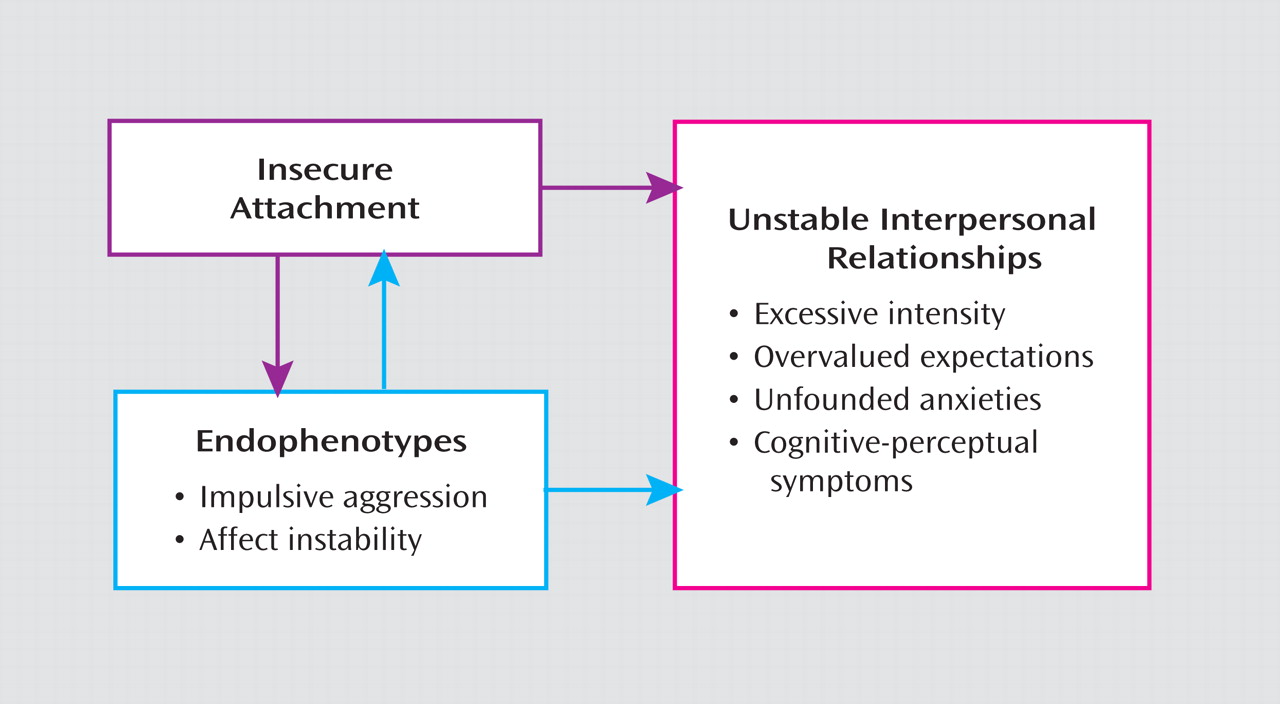
How things have changed! We now have a vastly enriched understanding of borderline pathology, thanks to the invaluable contributions of clinical and basic science research. We now recognize that the “stress-vulnerability” model of disease is a useful guide to a biopsychosocial concept of borderline personality disorder patients. Core heritable endophenotypes of affective dysregulation and impulsive aggression have been identified
(1) . Borderline pathology is at least partially “hard-wired,” involving brain abnormalities that can be identified by brain imaging techniques. Intriguing new findings suggest inherent hyperactivity of the amygdala and overreaction to negative or even neutral facial expressions
(2), possibly correlated with interpersonal hypersensitivity. Patients with borderline personality disorder may be primed to overanticipate and overreact to real criticism or rejection, but they may also negatively personalize disinterest or inattention from others. Resulting states of “emotional overdrive” are, furthermore, difficult to extinguish due to impairment in the usual cortical capacity to downregulate or inhibit this limbic-driven emotionality or impulsivity
(3) . These heritable risk factors, in turn, interfere with the normal attachment process during development, and this disruption can be magnified when there is inadequate parental support. For patients with borderline personality disorder, these combined etiological factors produce arrested, distorted, or incomplete integration of aspects of self and others, resulting in early onset and persistence of profound interpersonal difficulties (
Figure 1 ). Normal early development becomes derailed, and the crucial developmental milestone of basic trust is not achieved.
In this issue of the
Journal, three articles are presented on borderline personality disorder by some of the leading experts who have helped shape the giant steps we have taken in our understanding of this prevalent and disabling condition. It is logical to mention first Gunderson’s elegant review
(4) of the ontogeny of borderline personality disorder as a diagnostic construct, from descriptions of its origins as a clinically described syndrome of uncertain etiology to current notions of borderline personality disorder as a brain disorder characterized by underlying heritable risk factors activated by environmental stress. Of particular importance is Gunderson’s closing admonition that however clear we may be about the contribution of biological vulnerability to characteristic symptomatic behavior such as self-injury, this behavior has meaning as well, often found in the trauma-laced early lives of patients with borderline personality disorder.
In this issue’s Clinical Case Conference, Goodman and colleagues
(5) summarize their work with a patient with borderline personality disorder, who was enrolled in a protocol involving dialectical behavior therapy, as well as concomitant research measurements of the patient’s reactions to emotional stimuli. The patient showed expected physiologic hyperresponsiveness to emotional stimuli but did not react subjectively with comparable intensity, which the authors speculate might suggest that the patient had the ability to mentalize, hence respond well to treatment, as indeed she did. The use of functional magnetic resonance imaging data at the outset and in the course of treatment, although perhaps not ready for prime time, is a promising new pathway to guide treatment planning and to understand treatment progress.
Also in this issue, in the Treatment in Psychiatry feature, Gabbard and Horowitz
(6) present an intriguing discussion of the role of insight and of working with the transference in the context of our current expanded scope of evidence-based effective treatments for borderline personality disorder. They make the important point that all patients with borderline personality disorder are not alike, so the decision to utilize specific treatment elements such as transference interpretation should be matched to the individual characteristics of each patient. In considering the phases of treatment outlined by Gabbard and Horowitz, an additional goal is to explore how to measure progress in standardized ways. For example, the authors recommend “using rational ‘cognitions’ to counteract habitual, almost ‘knee-jerk’ assumptions and fantasies” that reflect dysfunctional beliefs and patterns. Work of this sort is reminiscent of what LeDoux
(7), some time ago, described as the goal of psychotherapy—to teach the cortex to control the amygdala, focusing on two critical brain regions now known to be dysregulated in patients with borderline personality disorder.
It is interesting that, although we now recognize the importance of heritable risk factors predisposing a patient to develop borderline personality disorder, the evidence-based core treatment recommended for this disorder is psychotherapy, an intervention long thought to change the
mind but not necessarily the
brain . Ironically, we also now understand that intensive psychotherapy is a form of long-term learning and memory, which indeed changes the brain. Psychotherapy is thus, at least in part, a biological treatment. But one important emphasis here is the reference to “long-term.” How many of us remember the mountains of material we memorized the day before that critical exam—the one, in fact, that we aced? Short-term retention is a different animal from long-term memory, as Kandel has taught us
(8), and the neurobiological mechanisms for the two are totally different. It is not, therefore, surprising that a few sessions of psychotherapy do not “stick.” Effective psychotherapy for patients with borderline personality disorder takes time, commitment, and persistence. Often the biggest hurdle is to engage the patient in treatment—to establish a partnership that can endure so that any one of the many types of effective treatments can take hold and lead to lasting change. In all three articles in this issue, the importance of the patient’s ability to mentalize is emphasized. Mentalizing is the basis for one evidence-based treatment for borderline personality disorder, mentalization-based therapy, developed by Bateman and Fonagy
(9) . But as they and others have pointed out, mentalizing is a fundamental framework that serves as a common denominator for therapies of many colors. It is a way to see ourselves from the outside and see others from the inside, a skill that, when learned by patients with borderline personality disorder, greatly facilitates psychotherapeutic work. The good news to underscore, during this Congressionally established Borderline Personality Disorder Awareness Month, is that many treatments have now been demonstrated to be effective for patients with borderline personality disorder. This optimistic state of affairs situates us very far along from the discouraging early days of borderline personality disorder’s diagnostic arrival.