Ideally, interventions to improve the quality of mental health care should be broadly effective across populations, including those of lower socioeconomic status. Quality improvement programs tailored for lower-income populations have been shown to be effective. For example, cognitive-behavioral therapy (CBT), antidepressants, and extensive outreach and support were shown to be effective for low-income Latina and African American women with depression (
1), group support and antidepressants were shown to be effective for impoverished Chilean patients (
2), and medication and problem-solving therapy were effective for low-income depressed patients with cancer (
3). However, more universal quality improvement interventions designed for broader segments of the population may or may not have equivalent effects across vulnerable subpopulations. Some universal quality improvement interventions have been shown to benefit all study participants uniformly (
4), and others have been shown not only to be broadly clinically effective but to have a differentially positive effect on vulnerable populations, namely, ethnic minorities (
5,
6). For example, the Partners in Care project, a primary care effectiveness quality improvement study, found greater outcome improvement for minorities than whites and lower outcome disparities among minorities relative to whites in quality improvement programs compared with enhanced usual care over 9 years of follow-up (
1,
7,
8). Such interventions serve a dual purpose in that they improve quality broadly while at the same time reducing disparities in outcomes.
Attention has been focused on racial and ethnic disparities, but other factors that increase risk for substandard treatment, such as lower socioeconomic status, warrant further exploration. Researchers have cited the contributions of poverty to the development of poor mental health, particularly environmental toxins, food insecurity, geographic barriers to health care, violence, limited economic opportunities, crime, and increased stress. However, less is known about how lower socioeconomic status affects mental health treatment outcomes. Anxiety is more prevalent in disadvantaged populations (
9,
10), and poorer persons have been shown to have poorer outcomes (
11,
12). Chronic economic deprivation increases levels of both anxiety and depression (
13). Having fewer resources, such as funds for transportation, child care, or health insurance, may also indirectly affect clinical outcomes and continued engagement in care or adherence to treatment (
14–
16).
We previously found evidence that a flexible treatment delivery model for anxiety disorders in the primary care setting was superior to usual care (
17). The Coordinated Anxiety Learning and Management (CALM) intervention, a collaborative care intervention for anxiety disorders in primary care, resulted in greater improvement in anxiety symptoms, reduced functional disability, and improved quality of care over 18 months compared with treatment as usual. In the present study, we examined the clinical effectiveness of the CALM intervention relative to income. Although more work has been done for depression, evidence for the effect of quality improvement programs for anxiety disorders on lower-income populations is lacking. Our previous study of persons with panic disorder revealed a comparable clinical response between lower- and higher-income individuals in a collaborative care intervention (medication and CBT) over 12 months of follow-up (
4). Other than our previous work, we are aware of no other study of quality improvement or collaborative care intervention specifically for anxiety disorders that has focused on the potentially moderating effect of income on clinical outcomes. Since our study population was relatively wealthy and about 50% of the lower-income participants were white, the study offers an opportunity to examine the association between income and clinical outcomes without substantial confounding by race. In addition, since most poorer persons receive mental health treatment in primary care rather than specialty care settings (
18), data from the CALM study are broadly relevant to the examination of lower income and clinical outcomes.
We hypothesized that lower-income participants in the CALM intervention would show less improvement or would improve at a lower rate than higher-income individuals. We reasoned that participants with lower incomes would not only be more ill at baseline, but they would also be likely to have more continual economic stress over the course of the 12-month treatment program, placing them at risk for less robust clinical response. On the other hand, we also hypothesized that it is possible that lower-income individuals assigned to CALM would improve at a higher rate because CALM facilitates access to evidence-based treatment, which may be less available to persons with lower incomes in usual care. This study contributes to the ongoing discussion as to whether or not, and to what extent, quality improvement interventions should be universal for specific vulnerable populations, as opposed to targeted or tailored (
19).
Method
Sample
We enrolled 1,004 primary care patients with panic disorder, social anxiety disorder, generalized anxiety disorder, or posttraumatic stress disorder (PTSD) between June 2006 and April 2008 in the CALM study. CALM is the largest randomized trial of collaborative care for anxiety disorders to date (
17,
20).
Four sites coordinated patient recruitment: the University of Washington, Seattle, the University of California at San Diego and Los Angeles, and the University of Arkansas for Medical Sciences at Little Rock. Each of the four sites selected clinics in their geographic area to participate. Candidate clinics were evaluated, and 17 clinics were selected based on a number of considerations, including provider interest, space availability, size and diversity of the patient population, and insurance mix (public and private), with the goal of recruiting a diverse population of patients and clinics.
A facilitated-referral approach was used to recruit participants. Primary care providers and clinic nursing staff directly referred potential participants. In addition, the coordinating sites actively publicized the study within each clinic, allowing for self-referral. Referred participants met with a study anxiety clinical specialist to determine eligibility for CALM. Eligible individuals were required to have patient status at one of the participating clinics; be at least 18 years old; meet DSM-IV criteria for generalized anxiety disorder, panic disorder, social anxiety disorder, or PTSD (based on the Mini-International Neuropsychiatric Interview [
21]); have a score ≥8 (indicating moderate but clinically significant anxiety symptoms on a scale ranging from 0 to 20) on the Overall Anxiety Severity and Impairment Scale (
22); be willing to participate in the study; and be able to provide written, informed consent. Exclusion criteria were serious alcohol or drug use (specifically, alcohol or marijuana dependence or any other drug abuse or dependence, including methadone; 4% were excluded for this reason), unstable medical condition, marked cognitive impairment, active suicidal intent or plan, psychosis, or bipolar I disorder. Individuals already receiving ongoing CBT, those without routine access to a telephone, and those who could not speak English or Spanish were excluded.
Of 1,620 patients referred and interviewed for eligibility, 1,062 were determined to be eligible, and after the study procedures were explained, 1,036 provided written informed consent. After a baseline interview, 1,004 participants were randomly assigned to CALM or to usual care using an automated computer program at RAND. The RAND Survey Research Group conducted all baseline and follow-up assessments (at 6, 12, and 18 months) by telephone. Randomization was stratified by clinic and presence of comorbid major depression using a permuted block design. Block size was masked to all clinical site study members.
Intervention Design
CALM is a flexible, collaborative care delivery model for primary care anxiety treatment that addresses any of four common anxiety disorders (generalized anxiety disorder, panic disorder, social anxiety disorder, and PTSD) in primary care. It provides strategies to enhance patient engagement in treatment, including allowing choice of CBT, medication, or both, and also provides the option for additional treatment over the course of a year. It uses a web-based outcomes system to optimize treatment decisions and a computer-assisted program to allow CBT-inexperienced care managers to optimize both delivery of CBT and fidelity to the CBT model. Medication is prescribed by primary care physicians with care manager assistance in promoting adherence, dose optimization, and medication switches or augmentation. Although the CALM intervention was not specifically tailored for special groups of participants, an ethnicity advisory group reviewed all materials and content of the intervention to ensure that it was appropriate for African Americans, Asians, Latinos, and whites.
CALM patients initially received their preferred course of treatment over 10–12 weeks. The CBT program included five generic modules (education, self-monitoring, hierarchy development, breathing training, and relapse prevention) and three modules (cognitive restructuring, exposure to internal stimuli, and exposure to external stimuli) tailored to the four specific anxiety disorders. Patients who had multiple anxiety disorders (about two-thirds of participants) were asked to choose the most disabling or distressing disorder to focus on within CBT, with the expectation that their comorbid disorders would also improve. CBT was administered by the care manager, referred to as the anxiety clinical specialist. A local study psychiatrist provided single-session medication management training to providers, as-needed consultation by telephone or e-mail, and, occasionally, face-to-face assessment for complex patients. The algorithm emphasized first-line use of selective serotonin reuptake inhibitors or serotonin-norepinephrine reuptake inhibitors, as well as dose optimization and side-effect monitoring. If needed, these were followed by second- and third-step combinations of two antidepressants or an antidepressant and a benzodiazepine. The anxiety clinical specialist monitored adherence and related medication suggestions from the supervising psychiatrist to the primary care provider.
Patient outcomes were tracked by the anxiety clinical specialist on a web-based system. The goal was either clinical remission, defined as an anxiety scale score <5, or sufficient improvement such that the individual did not want further treatment (
23). Symptomatic patients could receive additional treatment with CBT or medication for up to 12 months. After treatment was completed, participants received monthly relapse prevention follow-up telephone calls to reinforce CBT skills or medication adherence. Most participants assigned to the CALM intervention completed the treatment course in 6 months, but occasionally the course of treatment was interrupted, usually by life events or the emergence of substance abuse or dependence. Participants assigned to usual care were treated by their physicians in the usual manner, which could include referral to a mental health specialist.
Measures
Mental Health Outcomes
An assessment battery was administered by telephone at baseline and at 6, 12, and 18 months. The primary outcome for the secondary analyses reported here included psychic (psychological symptoms) and somatic (physical symptoms) aspects of anxiety, two key components of all anxiety disorders, as measured by the Brief Symptom Inventory-12 (
24) subscales for anxiety and somatization. Lower scores on the Brief Symptom Inventory indicate fewer symptoms. Other measures were the global mental and physical health subscales of the 12-Item Medical Outcomes Study Short-Form Health Survey (
25) and the Centers for Disease Control and Prevention (CDC) Healthy Days Measures, a single-item estimate of restricted activity days or days (in the past 30) in which poor physical or mental health prevented a participant from performing usual activities (
26). For the global mental health and physical health subscales, higher scores indicate better functioning, while for the CDC measure, lower scores reflect better functioning.
Income
Income was assessed at baseline. We derived a dichotomous measure of high and low income by first calculating weighted average income thresholds based on the Federal Poverty Guidelines (
27), adjusted for family size, age of respondent, and number of children <18 years old. Family income divided by this threshold value created a poverty ratio. We then divided the sample into those with incomes at or below 200% of the poverty level and those with incomes above that threshold. Among CALM participants, 287 were designated as having lower income, including 133 in the intervention group and 154 in the comparison group, and the remaining 717 were designated as having higher income, including 370 in the intervention group and 347 in the comparison group.
Statistical Analysis
We compared baseline demographic and clinical characteristics of individuals with lower and higher incomes using t tests and chi-square tests for continuous and categorical variables, respectively. For the longitudinal analysis of intervention effects by income group, we jointly modeled the outcomes at the four assessment times (baseline and 6, 12, and 18 months) by study site, income, time, and intervention; by the two-way interactions of time and intervention, income and time, and income and intervention; and by the three-way interaction of time, intervention, and income. We fitted the models using a restricted maximum likelihood approach, which produces valid estimates under the missing-at-random assumption. This approach uses all available data to obtain unbiased estimates of model parameters. We used SAS, version 9.3 (SAS Institute, Cary, N.C.), to perform the statistical analysis. All p values were two-tailed.
Results
Persons in the lower-income group (N=287) were younger, less educated, and less likely to have health insurance compared with those in the higher-income group (N=717) (
Table 1).
Lower-income individuals tended to be sicker at baseline, as reflected by more medical and anxiety comorbidities, and had higher disability scores on both anxiety-specific (Sheehan Disability Scale) and generic (mental and physical health subscales of the short-form health survey) functioning measures, indicating poorer physical and mental functioning. While lower-income participants were no more likely to meet criteria for panic disorder, generalized anxiety disorder, or social anxiety disorder than higher-income participants, they demonstrated a higher prevalence of both PTSD and comorbid depression at baseline.
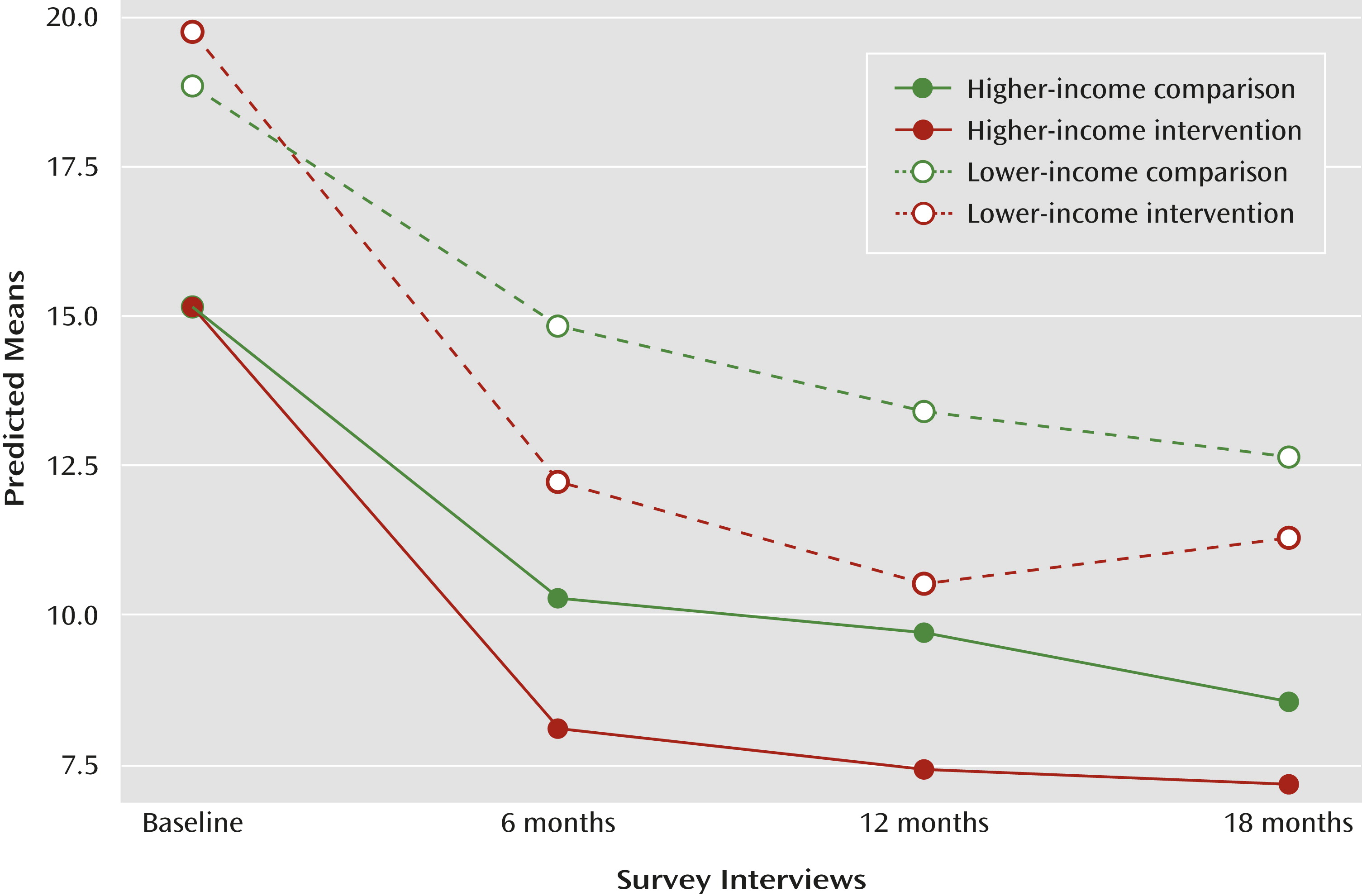
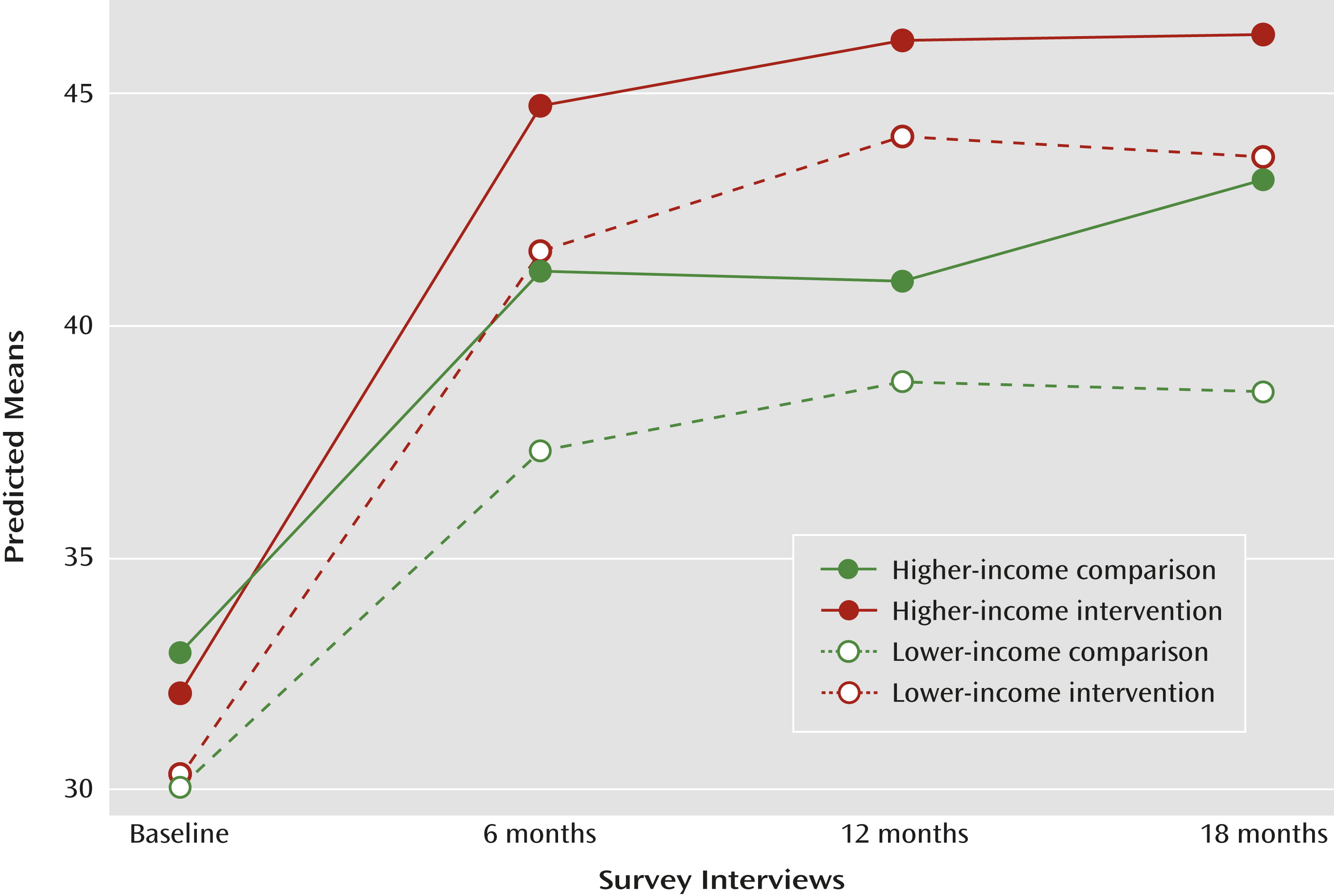
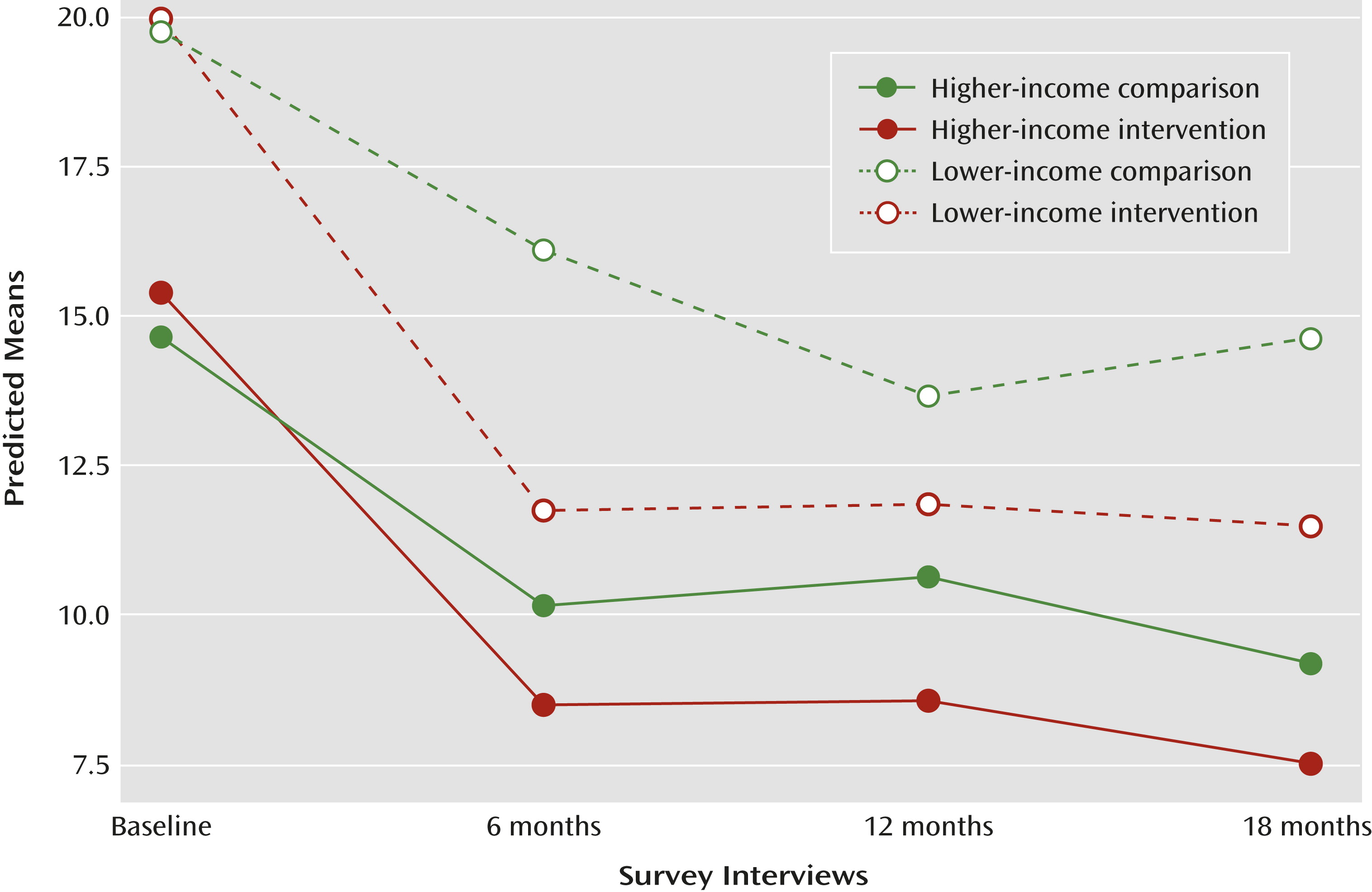
Baseline and follow-up symptom ratings predicted mean scores for lower- and higher-income participants in the CALM and usual care conditions from general linear mixed models using repeated measures for the three outcomes (as defined by scores for the Brief Symptom Inventory, short-form health survey mental health functioning, and restricted activity days), as presented in
Figure 1,
Figure 2, and
Figure 3. In all three models, the three-way interaction of time, intervention, and income did not reach statistical significance, nor did the two-way interactions between income and time and between income and intervention. However, the two-way interaction between time and intervention was significant in all three models (Brief Symptom Inventory score, p<0.0001; short-form health survey mental health functioning score, p<0.0001; and restricted activity days score, p<0.003).
Lower-income participants reported more symptoms at baseline on the Brief Symptom Inventory than higher-income participants, regardless of whether or not they were assigned to CALM or usual care, but lower-income participants assigned to CALM had higher scores on this functioning measure at baseline. The CALM intervention lowered symptoms significantly more than usual care for both lower- and higher-income individuals over 6 and 12 months, but by 18 months, there was no significant difference in scores between lower-income participants assigned to CALM and lower-income participants assigned to usual care, although the difference in these scores between higher-income participants in both treatment groups persisted (
Figure 1). This may be because fewer lower-income individuals were assessed at 18 months, especially for the CALM intervention. A similar pattern was seen for global mental health subscale scores (
Figure 2), although the intervention effect was comparable and significant for both lower- and higher-income individuals over all 18 months. At 6 months, the CALM intervention brought the global mental health subscale scores for lower-income participants to the level of that for higher-income comparison subjects. The pattern for restricted activity days scores, presented in
Figure 3, was similar to that for Brief Symptom Inventory scores (
Figure 1). Higher-income participants had fewer restricted activity days than lower-income participants at all times in both CALM and usual care. There was no difference in the restricted activity days between the CALM and usual care groups at baseline. However, at the follow-up assessments, the CALM group had significantly fewer restricted activity days than the usual care group for both lower- and higher-income participants, except at the 12-month interview for lower-income individuals, in which the difference became nonsignificant. Again, this may be because fewer individuals were assessed at that time in the lower-income group, especially for the CALM intervention.
To examine whether or not lower-income participants in the CALM intervention differed in terms of treatment patterns, we assessed whether they experienced interrupted treatment and whether they participated in the relapse prevention component of the program. (This information was available only for participants in the intervention group [N=503].) We also compared the number of completed CBT sessions across income groups. Lower-income participants (N=126) were significantly more likely to have interrupted treatment compared with higher-income participants (N=356) (12.7% compared with 7.0%, χ2=3.85; p<0.05) but were significantly less likely to have participated in relapse prevention (61.9% compared with 72.2%, χ2=4.65; p=0.03), and they completed fewer CBT sessions (mean=6.00 compared with mean=7.39; χ2=10.42, p=0.001 from Kruskal-Wallis test).
Discussion
As expected, lower-income participants in the CALM study were more ill and disabled at baseline than higher-income participants. At baseline, lower-income individuals were not only more burdened with symptoms but also more functionally impaired.
At the same time, the lower- and higher-income groups were similar in terms of clinical response to the CALM intervention, as depicted by the comparable slopes of the lines in
Figures 1,
2, and
3. The lower-income participants began the study sicker and ended the study sicker than the higher-income participants. Thus, although lower-income individuals experienced a comparable degree of clinical improvement relative to higher-income individuals, the disparities related to income were not eliminated. These findings are similar to those in our previous study of collaborative care for panic disorder (
4) as well as to those of Areán et al. (
12) in the IMPACT (Improving Mood–Promoting Access to Collaborative Treatment) collaborative care intervention for older adults. It is possible that the persistent differential in clinical outcomes across income groups results from having fewer resources available (e.g., funds for child care or transportation) to assure continued access to treatment. However, it could also relate to differential beliefs or attitudes about the relevance of CBT given the realistic life stressors among lower-income individuals. Regardless of the explanation, it is conceivable that had lower-income participants received comparable numbers of CBT sessions, relapse prevention, and continuous care, they may have had a more robust clinical response relative to those with higher incomes.
Most participants in the CALM study completed treatment within the initial 6-month period but could be actively followed by the study clinicians for 12 months, after which they received only one follow-up assessment by telephone from the survey group but no clinical interventions. Therefore, one might expect that clinical response would be greatest at 6 months and might deteriorate after that point, a pattern reflected in our data. However, given that the lower-income participants continued to be subject to more economic stress, it may be especially remarkable that they did not experience significantly greater deterioration of clinical improvements after 6 months relative to the higher-income participants. This suggests that the effect of the CALM intervention was sustained equally well across participants regardless of income level and in spite of presumed differences in treatment intensity and continuity, at least over the first 12 months. This is in contrast to a recently reported depression intervention for lower-income women with comorbid cancer in which marked recurrence of depression occurred postintervention (
3).
This study suggests that if the goal is to obtain an equivalent clinical response across lower- and higher-income patients, clinic-based collaborative care for anxiety disorders as delivered in the CALM study is adequate and effective. However, it is possible that the lower-income participants could have benefited to a greater extent from tailored supplements to treatment, such as assistance with transportation or child care or even novel delivery approaches, such as treatment delivered in the home. Providing such features for lower-income individuals might be more likely to result in an intervention that not only improves quality of care but also even further reduces disparities in clinical outcomes. Studies are needed to address significant barriers to building collaborative care teams in safety-net care populations, including approaches to facilitate communication across mental health and medical providers through newer health technologies.
Limitations
Because CALM participants were recruited from primary care settings, most had health insurance and the resources needed to get to the primary care clinics. Before entering the CALM study, 57% of participants were already receiving medication, much of it clinically appropriate. Hence, the participants represent a select group that did not improve with first-line medication treatment administered by a primary care provider. These participants as a whole were better off economically than many segments of the population who may not have ready access to primary care or who may live in even more stressful situations in which meeting daily needs for survival are paramount. Our findings therefore should not be interpreted as applying to all groups of lower-income persons. In addition, while the study used common and widely accepted outcome measures, these measures capture symptoms at only one point in time and may not reflect the often episodic nature of anxiety disorders.
Our analysis illustrates that a collaborative care intervention for anxiety in primary care worked equally well for those with lower and higher incomes but did not eliminate baseline disparities in mental health status associated with economic disadvantage. Our findings should reduce the tendency to be nihilistic about how mental health treatments affect lower-income individuals. Even when treatments were delivered with less intensity and frequency than desirable, clear and meaningful benefits were obtained.