Complex Challenges in Treating Depression During Pregnancy
Abstract
Epidemiology
Risk Factors
Etiology and Phenomenology of Symptoms
In Utero Environment
Impact of Depression During Pregnancy
Antidepressant Use
Impact of Antidepressant Use During Pregnancy
Impact of Nonpharmacologic Treatments on Pregnancy
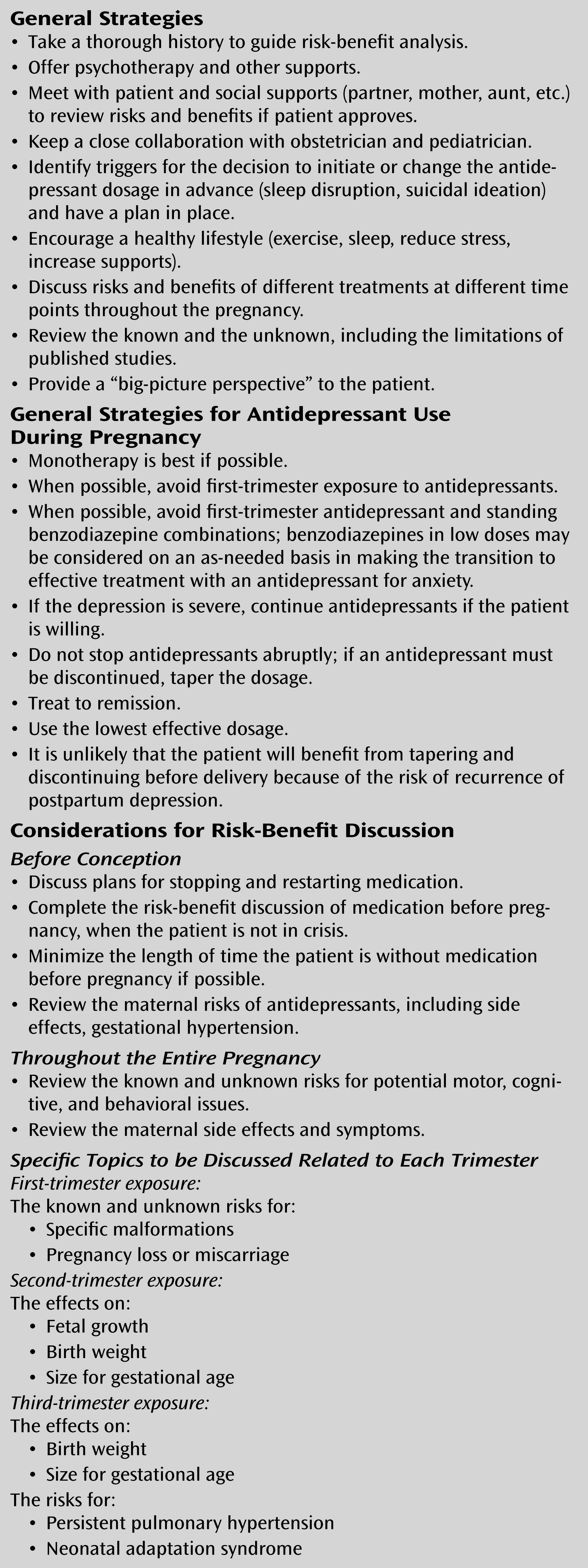
Clinical Approach to Treating Women During Pregnancy
| Outcome | Antidepressants | Depression |
|---|---|---|
| Birth outcomes | ||
| Miscarriage | Increased risk with use in early pregnancy: 12.4% (exposed) versus 8.7% (unexposed); relative risk=1.45 (within expected range of 15%–20% of pregnancies) (38). Limitations: other contributing factors not consistently controlled for (39) | Inconclusive: limitations of sample sizes and methodologies (31) |
| Effects on growth | Increased risk for slower rates of head growth (25). Limitations of studies: difficulty untangling duration of exposure, timing of exposure, severity of illness, other confounding factors | Increased risk for slower fetal body and head growth (25) |
| Low birth weight | Increased risk with SSRI or TCA use (41); in some studies, accounted for by shorter gestational duration (40) | Inconclusive: increased risk in some (21) but not all (24) studies |
| Small for gestational age | Increased risk with SSRI use (small compared with depressed unexposed) (41– 43) | Inconclusive: increased risk in some (41) but not all (31) studies |
| Preterm delivery (<37 weeks’ gestation) | Inconclusive: increased risk in some but not all studies (SSRIs, TCAs, SNRI/NRIs) (43). If increased risk found, modest difference in mean gestational duration of 1 week or less (31). Controlling for confounders had no effect. Dependent on duration of in utero exposure: more exposure, more likely decrease in gestational age (44) | Inconclusive: increased risk in some (21) but not all (31) studies |
| Structural malformations | Studies from linked databases and case cohort studies. No association between SNRI/NRI use and malformations; conflicting associations for TCA use and malformations (41); conflicting associations for SSRI use and malformations (specifically paroxetine) (39, 41– 45) | No studies |
| Cardiac malformations | Conflicting results: No increased rate of major or specific cardiac malformation with SSRI exposure (four studies) (31, 47). First-trimester exposure to paroxetine increased risk of cardiac malformations (three studies); increase not found in other studies (three studies) (31). Combination of SSRI and benzodiazepine may increase congenital heart defects (45) | No studies |
| Other | Specific defects found; small risks and not replicated (48, 49) | No studies |
| Neonatal outcomes | ||
| Behavioral | Increased risk for irritability, jitteriness, seizures with TCAs (44). Increased risk for irritability, tachypnea, hypoglycemia, temperature instability, weak/absent cry, seizures (15%–30% of women who took SSRIs in late pregnancy); transient symptoms (41, 51) | Increased risk for irritability, decreased activity and attentiveness, fewer facial expressions (23) |
| Persistent pulmonary hypertension | Conflicting results; some show increased risk (44, 55, 57) with later gestational exposure to SSRIs and others do not (54, 56). Study of 1.6 million births found an absolute risk increase from 1.2/1000 base rate to 3/1000 in SSRI exposure; only 33 infants exposed to SSRIs in late pregnancy with persistent pulmonary hypertension identified (57). | No studies |
| Long term growth, IQ, behavioral | Limited information; most studies show no association with use of SSRIs or TCAs. Subtle effects on motor and developmental control (52). Slower in reaching developmental milestones compared with unexposed (but within range of normal development catches up by 19 months) (53). Possible increased risk of autism spectrum disorder (odds ratio=2.2) but very small percentage (2.1%) attributed to SSRI exposure; limitations include inability to control for severity, actually taking medication, other risk factors (58). No difference in IQ, language, development, behavioral development (comparison of fluoxetine, TCAs, controls) (59). IQ negatively associated with depression duration; language negatively associated with number of depressive episodes after delivery; comparison of fluoxetine, TCAs, controls (60) | Greater developmental delay in infants exposed to depressive symptoms at 18–32 weeks’ gestation compared with nondepressed mothers (odds ratio=1.34) (26). No effect in one study (28). Possible indirect effects (27). Limitations due to bias (31) |
| Maternal outcomes | ||
| Pregnancy-induced hypertension, pre-eclampsia, and eclampsia | Increased risk (50%–53%) (61, 62). Limitations of linked databases, limited control for depression and other confounding risk factors, maternal report of medication use | Conflicting data. In one study, no increased risk (30). In another study, increased risk for pre-eclampsia (odds ratio=52.5) and eclampsia; limitations: did not account for antidepressant use (29) |
Summary and Recommendations
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

