Lithium Treatment Moderate-Dose Use Study (LiTMUS) for Bipolar Disorder: A Randomized Comparative Effectiveness Trial of Optimized Personalized Treatment With and Without Lithium
Abstract
Objective
Method
Results
Conclusions
Method
Study Design
Study Participants
| Lithium Plus OPT (N=141) | OPT Alone (N=142) | All Randomized Participants (N=283) | ||||
|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | N | % |
| Female | 77 | 54.6 | 83 | 58.5 | 160 | 56.5 |
| Race | ||||||
| White | 107 | 75.9 | 106 | 74.6 | 213 | 75.3 |
| African American | 25 | 17.7 | 23 | 16.2 | 48 | 17.0 |
| Asian | 5 | 3.5 | 7 | 4.9 | 12 | 4.2 |
| Other | 4 | 2.8 | 6 | 4.2 | 3 | 1.1 |
| Ethnicity | ||||||
| Hispanic or Latino | 16 | 11.3 | 23 | 16.3 | 39 | 13.8 |
| Not Hispanic or Latino | 125 | 88.7 | 118 | 83.7 | 243 | 86.2 |
| Education | ||||||
| < High school | 5 | 3.5 | 14 | 9.9 | 19 | 6.7 |
| High school diploma/GED | 34 | 24.1 | 24 | 16.9 | 58 | 20.5 |
| Some college | 41 | 29.1 | 37 | 26.1 | 78 | 27.6 |
| Technical or associates degree | 13 | 9.2 | 14 | 9.9 | 27 | 9.5 |
| College diploma (Bachelors Degree) | 37 | 26.2 | 28 | 19.7 | 65 | 23.0 |
| Graduate or professional degree | 11 | 7.8 | 25 | 17.6 | 36 | 12.7 |
| Employment Status | ||||||
| Employed | 52 | 36.9 | 63 | 44.4 | 115 | 40.6 |
| Unemployed | 49 | 34.8 | 44 | 31.0 | 93 | 32.9 |
| Disability recipient | 22 | 15.6 | 25 | 17.6 | 47 | 16.6 |
| Other | 18 | 12.7 | 10 | 7.0 | 20 | 9.9 |
| Bipolar I disorder | 108 | 76.6 | 108 | 76.1 | 216 | 76.3 |
| History of psychiatric hospitalizations | 59 | 43.7 | 60 | 42.9 | 119 | 43.3 |
| History of suicide attempts | 57 | 40.7 | 58 | 41.4 | 115 | 41.1 |
| Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 38.7 | 11.7 | 39.4 | 13.0 | 39.1 | 12.3 |
| MADRS score | 22.4 | 9.62 | 22.5 | 10.60 | 22.46 | 10.11 |
| CGI severity score | 4.3 | 0.90 | 4.3 | 0.88 | 4.27 | 0.89 |
| YMRS score | 13.0 | 8.49 | 12.0 | 7.96 | 12.49 | 8.23 |
| Estimated depressive episodes in the previous yearb | 3.5 | 4.1 | 3.3 | 3.1 | 3.4 | 3.6 |
| Estimated manic or hypomanic episodes in the previous yearc | 5.2 | 9.1 | 3.2 | 3.4 | 4.2 | 6.9 |
Randomization and Treatment
Outcomes
Statistical Analysis
Sample size determination.
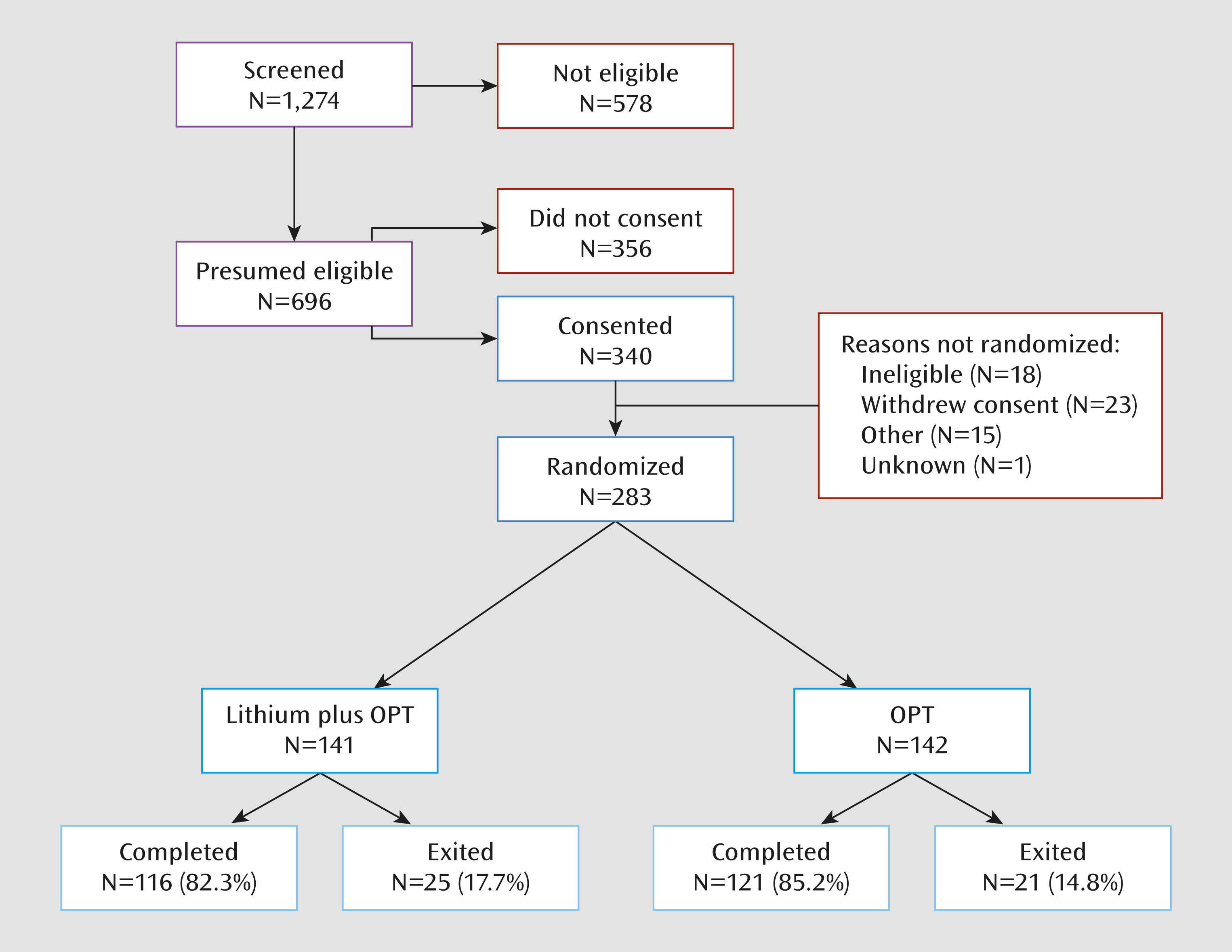
Attrition.
Results
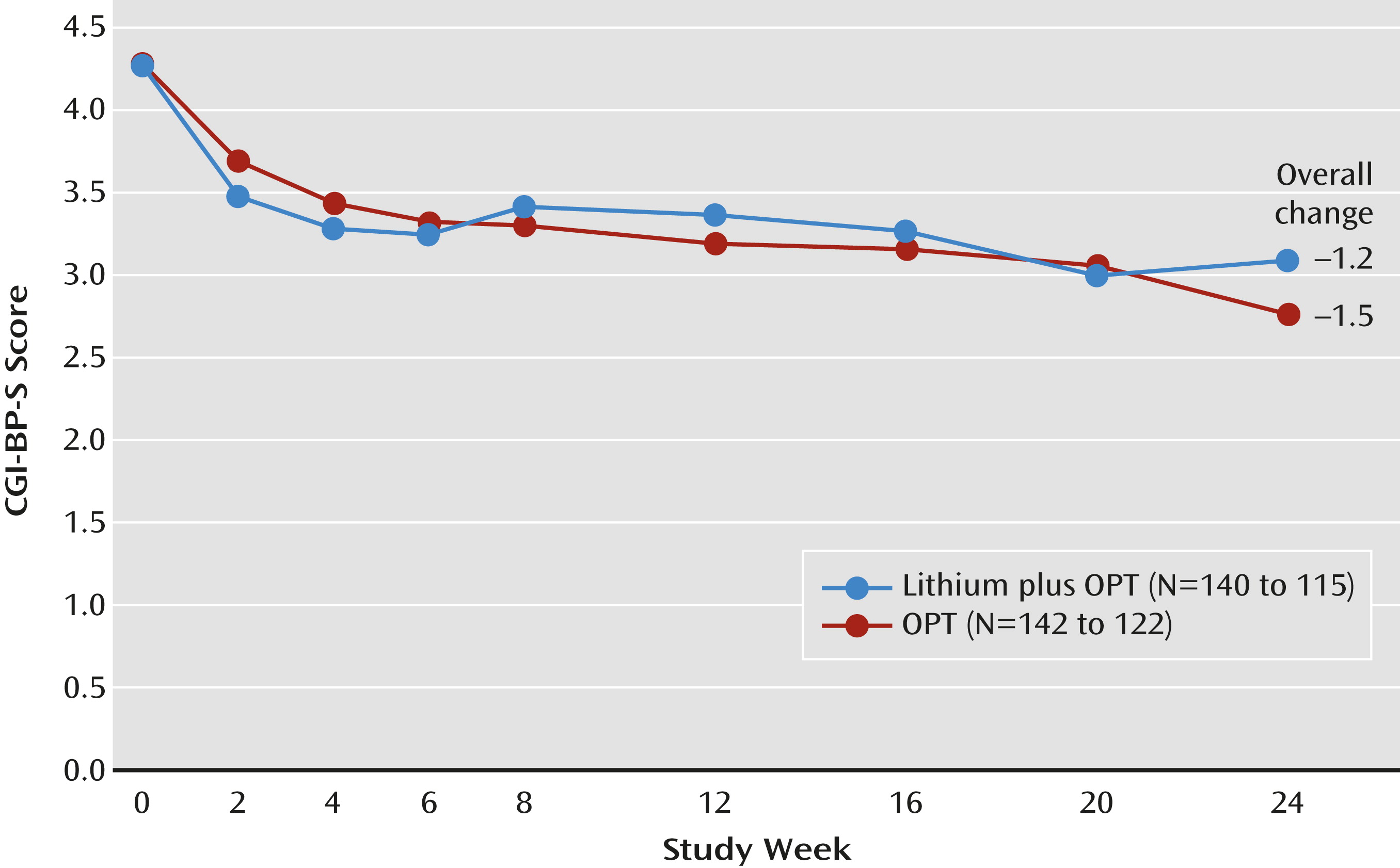
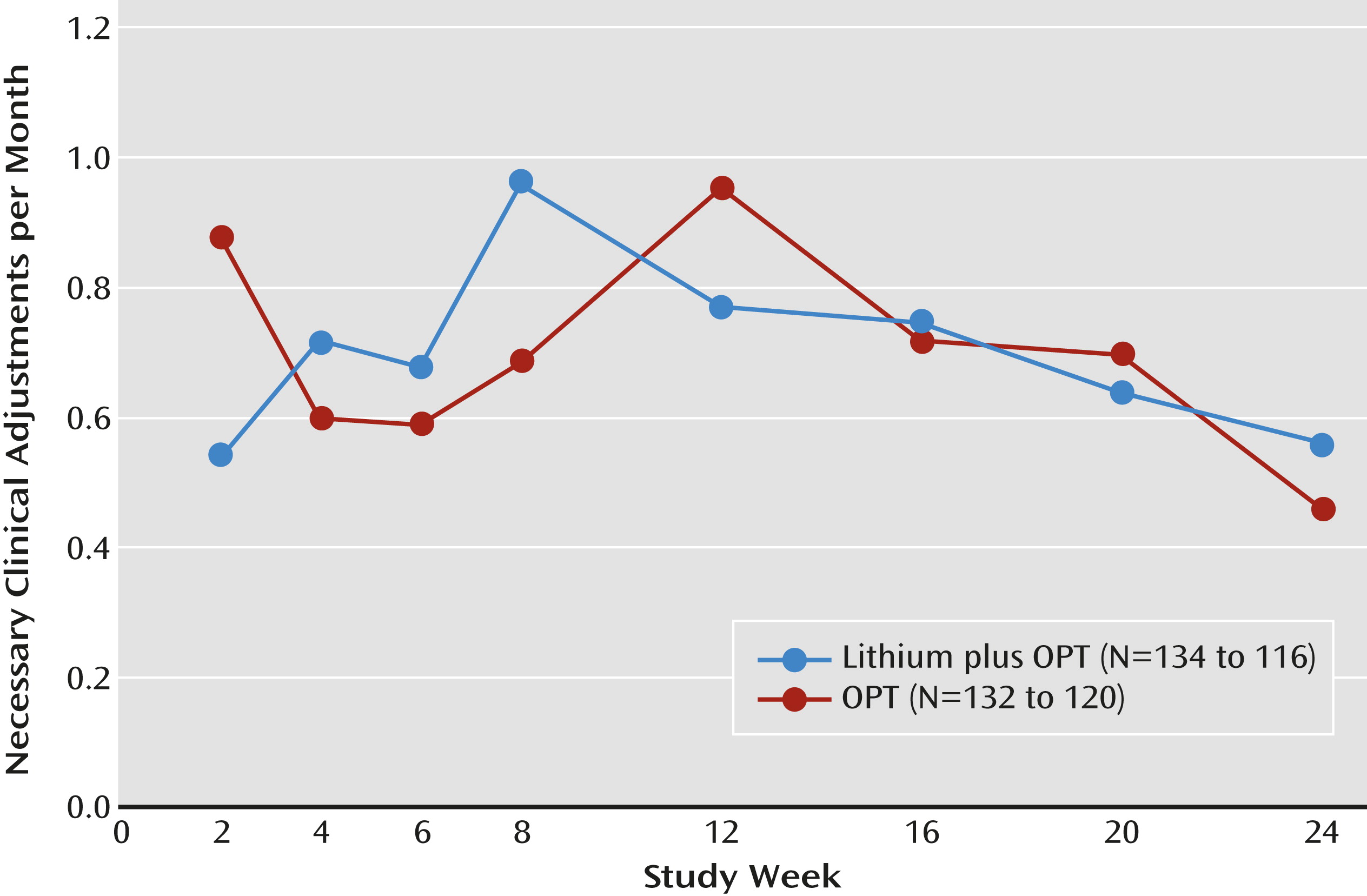
Discussion
Footnotes
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

