Results of a Multicenter Randomized Controlled Trial of the Clinical Effectiveness of Schema Therapy for Personality Disorders
Abstract
Objective
Method
Results
Conclusions
Method
Treatment, Therapists, and Treatment Integrity Check
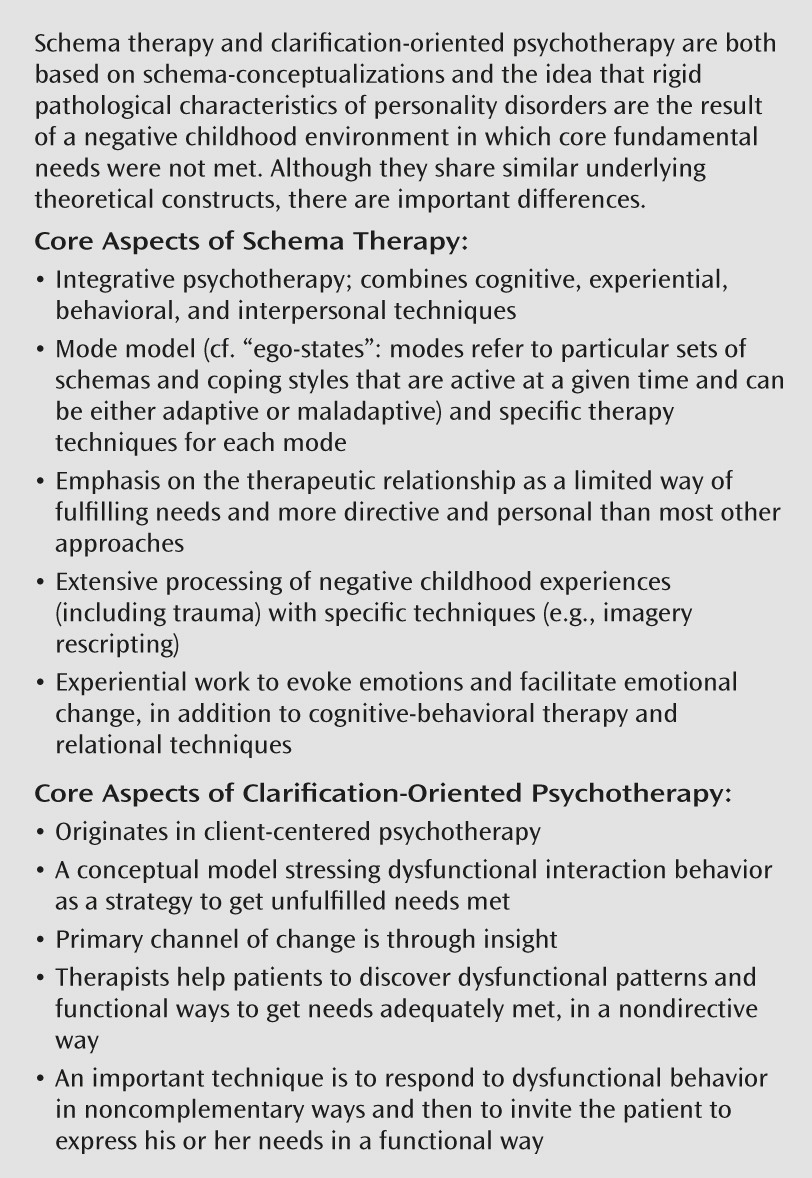
| Schema Therapy | Clarification-Oriented Psychotherapy |
|---|---|
| Therapeutic relationship | |
| Directive (with regard to both content and process). | Nondirective as to content, directive with regard to process (the therapist proposes processes that foster clarification, confrontation with interfering processes). |
| Limited re-parenting: The therapist partly meets unmet childhood needs within healthy therapy boundaries (e.g., offers safe attachment, praises the patient, stimulates playfulness, and sets limits). | No focus on meeting the patient’s unmet childhood needs in the therapeutic relationship but on helping the patient to become aware of dysfunctional ways in which basic needs and motives are expressed. When the patient displays dysfunctional, unauthentic behavior, the therapist responds in ways not expected by patient (“noncomplementary response”). |
| The therapist is open about personal responses evoked by the patient, with frequent self-disclosure if deemed helpful. | Rogerian therapy conditions (unconditional acceptance, empathy, and genuineness) are necessary but not sufficient for change. |
| Psychoeducation: The therapist teaches the patient about core needs, as well as functional and dysfunctional behaviors, and links present problems to childhood experiences. | No psychoeducation. |
| Conceptual model of the personality disorder | |
| The patient’s problems are framed through schema modes: different “sides” of themselves that become activated by triggers related to childhood experiences. These modes govern the patient’s emotions, cognitions, and behaviors. | The patient’s problems are framed as dysfunctional interpersonal strategies to get basic motives/needs met. These nonauthentic and manipulative interpersonal strategies are shaped by cognitive-affective schemas about self, personal problems, and relationships with others evolved during development. |
| Importance of determining childhood origins of schemas/schema modes | |
| Central to model and treatment. Dysfunctional parenting and traumas in childhood are viewed as origins of dysfunctional schemas/modes. The therapist frequently links the present and the past. Extensive processing of childhood experiences (including traumas) and correcting internalized messages are achieved. | Childhood origins are important to understand development of cognitive-affective schemas but are not targets of specific change techniques. |
| Main mechanisms of change | |
| Corrective emotional experiences, cognitive change, and change in behaviors. The therapist is internalized as the “healthy adult.” | Insight: Patients should become aware of their authentic motives/needs and the dysfunctional cognitive-affective schemas interfering with functional interpersonal behaviors. |
| Targets of interventions | |
| Therapeutic relationship (limited re-parenting). | Process: Promote clarification (e.g., by proposing to attend to a basic need/motive) and challenge attempts to avoid clarification. |
| Memories of childhood are linked to present problems. | Schema change: Acquiring insight that dysfunctional schemas are incorrect. |
| Present problems outside therapy. | |
| Main techniques | |
| Experiential, cognitive, and behavioral techniques are geared to specific modes. | The therapist responds to problem behavior during the session in unexpected (noncomplementary) ways to create awareness. |
| The therapist initially takes the lead (e.g., challenges punitive parent mode on empty chair, intervenes in imagery re-scripting, empathically confronts the patient with dysfunctional behaviors, and proposes and stimulates functional behaviors). | The therapist responds to functional behavior in accepting (“complementary”) ways to strengthen the behavior. |
| Gradually, patients apply techniques themselves. | The therapist proposes constructive clarification processes and challenges avoidance. |
| The therapist facilitates patients to acquire insight into the incorrectness of cognitive-affective schemas (e.g., by one-person role-play). | |
| Treatment phase | |
| Year 1 | |
| Session 1–6: introduction into schema therapy, bonding and case conceptualization in terms of mode model. | Phase 1: Bonding, understanding the patient, and being complementary to authentic expression of basic needs and not complementary to unauthentic expression. |
| Session 7–24: focus on reducing coping modes and on historical and experiential work (e.g., imagery re-scripting, empty chair technique). | Phase 2: Bonding, confronting dysfunctional interpersonal strategies, and defining treatment goals. |
| Session 25–40: focus mostly on present (e.g. behavioral pattern breaking). | Phase 3: Bonding, clarification of schemas, and confronting avoidance tendencies. |
| Year 2 | Phase 4: Facilitating patients in acquiring insight into incorrectness of cognitive-affective schemas (e.g., with one-person role-play). |
| Session 41–50: monthly booster sessions to maintain and deepen changes. | Phase 5: Transfer to behavior: facilitating patients to change their behaviors. |
| Characteristic | Treatment | Analysis | |||||
|---|---|---|---|---|---|---|---|
| Schema Therapy (N=145) | Clarification-Oriented Psychotherapy (N=41) | Treatment As Usual (N=134) | |||||
| Mean | SD | Mean | SD | Mean | SD | pa | |
| Age (years) | 37.57 | 9.69 | 39.20 | 9.37 | 38.06 | 9.63 | 0.63 |
| N | % | N | % | N | % | pb | |
| Male | 66 | 45.5 | 18 | 43.9 | 55 | 41 | 0.75 |
| Education | |||||||
| Primary school | 6 | 4.1 | 3 | 7.3 | 3 | 2.2 | 0.85c |
| Lower vocational | 6 | 4.1 | 4 | 9.8 | 15 | 11.2 | |
| Lower secondary | 22 | 15.2 | 3 | 7.3 | 8 | 6 | |
| Higher secondary | 11 | 7.6 | 2 | 4.9 | 15 | 11.2 | |
| Intermediate vocational | 46 | 31.7 | 15 | 36.6 | 45 | 33.6 | |
| Preuniversity | 11 | 7.6 | 2 | 4.9 | 10 | 7.5 | |
| Higher vocational | 29 | 20 | 12 | 29.3 | 25 | 18.7 | |
| Academic | 14 | 9.7 | 0 | 0 | 13 | 9.7 | |
| Employment status | |||||||
| Housewife | 7 | 4.8 | 1 | 2.4 | 5 | 3.7 | 0.96 |
| Student | 7 | 4.8 | 3 | 7.3 | 6 | 4.5 | |
| Employed | 66 | 45.5 | 16 | 39 | 63 | 47 | |
| Disability | 47 | 32.4 | 17 | 41.5 | 46 | 34.3 | |
| Welfare | 17 | 11.7 | 4 | 9.8 | 14 | 10.4 | |
| Retired | 1 | 0.7 | 0 | 0 | 0 | 0 | |
| Primary personality disorder diagnosis | |||||||
| Avoidant | 74 | 51 | 19 | 46.3 | 70 | 52.2 | 0.86 |
| Dependent | 16 | 11 | 6 | 14.6 | 14 | 10.4 | |
| Obsessive-compulsive | 41 | 28.3 | 11 | 26.8 | 37 | 27.6 | |
| Paranoid | 8 | 5.5 | 1 | 2.4 | 5 | 3.7 | |
| Histrionic | 0 | 0 | 1 | 2.4 | 1 | 0.7 | |
| Narcissistic | 6 | 4.1 | 3 | 7.3 | 7 | 5.2 | |
| Secondary personality disorder diagnosis | |||||||
| None | 80 | 55.2 | 19 | 46.3 | 69 | 51.5 | 0.58 |
| Avoidant | 13 | 9 | 8 | 19.5 | 22 | 16.4 | 0.09 |
| Dependent | 9 | 6.2 | 3 | 7.3 | 2 | 1.5 | 1.00 |
| Obsessive-compulsive | 11 | 7.6 | 7 | 17.1 | 15 | 11.2 | 0.19 |
| Paranoid | 3 | 2.1 | 3 | 7.3 | 4 | 3 | 0.23 |
| Histrionic | 0 | 0 | 0 | 0 | 0 | 0 | |
| Narcissistic | 0 | 0 | 0 | 0 | 1 | 0.7 | 0.50 |
| Passive-aggressive | 6 | 4.1 | 1 | 2.4 | 3 | 2.2 | 0.64 |
| Depressive | 41 | 28.3 | 13 | 31.7 | 39 | 29.1 | 0.91 |
| Axis I comorbidity (current) | |||||||
| Anxiety disorders | 82 | 56.6 | 25 | 61 | 80 | 59.7 | 0.82 |
| Depressive disorder | 61 | 42.1 | 23 | 56.1 | 59 | 44.0 | 0.28 |
| Somatoform disorders | 17 | 11.7 | 4 | 9.8 | 11 | 8.2 | 0.62 |
| Substance abuse | 7 | 4.8 | 5 | 12.2 | 1 | 0.7 | <0.01 |
| Eating disorders | 3 | 2.1 | 1 | 2.4 | 6 | 4.5 | 0.50 |
| Other axis I disorders | 11 | 7.6 | 7 | 17.1 | 19 | 14.2 | 0.11 |
| Psychotropic medication at baseline | 71 | 49 | 18 | 43.9 | 74 | 55.2 | 0.36 |
| Mean | SD | Mean | SD | Mean | SD | p | |
| Number of treatments before baseline | 2.44 | 2.35 | 2.12 | 3.3 | 2.28 | 2.22 | 0.72a |
| Number of treatment modalities before baseline | 1.51 | 1.23 | 1.27 | 1.30 | 1.36 | 1.18 | 0.41a |
| Total duration of previous treatments (months) | 29.73 | 42.70 | 31.98 | 78.51 | 35.75 | 63.73 | 0.68a |
| Number of principal treatments over 3 years | 1.33 | 0.69 | 1.51 | 0.93 | 1.39 | 0.73 | 0.40c |
| Number of secondary treatments over 3 yearsd | 0.68 | 1.04 | 0.85 | 1.04 | 0.92 | 1.32 | 0.14c |
| Median | 25th–75th Percentile | Median | 25th–75th Percentile | Median | 25th–75th Percentile | pc | |
| Total number of sessions of indicated principal treatments over 3 years | 50 | 31–50 | 51 | 28–74 | 22 | 11–47 | <0.01 |
| Total number of sessions of additional treatments over 3 years | 0 | 0–11 | 5 | 0–18 | 3 | 0–18 | 0.04 |
| Total number of days in principal treatments over 3 years | 694 | 481–766 | 895 | 393–1038 | 522 | 243–863 | <0.01 |
| N | % | N | % | N | % | p | |
| Distribution of indicated principal treatments | |||||||
| Did not receive indicated treatment | 2 | 1.4 | 0 | 0 | 7 | 5.2 | |
| Schema therapy | 143 | 98.6 | 0 | 0 | 0 | 0 | |
| Clarification-oriented psychotherapy | 0 | 0 | 41 | 100.0 | 0 | 0 | |
| Cognitive-behavioral therapy | 0 | 0 | 0 | 0 | 26 | 19.4 | |
| Eye movement desensitization and reprocessing | 0 | 0 | 0 | 0 | 2 | 1.5 | |
| Insight-oriented psychotherapy | 0 | 0 | 0 | 0 | 56 | 41.8 | |
| Supportive therapy | 0 | 0 | 0 | 0 | 43 | 32.1 | |
| % | 95% CI | % | 95% CI | % | 95% CI | pf | |
| Medication use during 3 years | 40.4e | 34–47.1 | 50.0 | 40.1–59.8 | 58.2 | 51.2–64.9 | <0.001 |
| N | % | N | % | N | % | pb | |
| Number of patients still in treatment at follow-up | 19 | 13.1 | 15 | 36.6 | 35 | 26.1 | <0.01 |
| Results of treatment integrity tests | Mean | SD | Mean | SD | Mean | SD | pa |
| Schema therapy techniques | 1.65g | 0.40 | 1.19 | 0.15 | 1.21 | 0.16 | <0.001 |
| Clarification-oriented psychotherapy techniques | 1.60 | 0.41 | 1.79h | 0.46 | 1.51i | 0.38 | <0.001 |
| Facilitative conditions | 3.80g | 0.63 | 3.52 | 0.67 | 3.45 | 0.69 | <0.001 |
| Explicit directiveness | 3.47g | 0.50 | 3.15 | 0.48 | 3.24 | 0.60 | <0.001 |
Statistical Analyses
Results
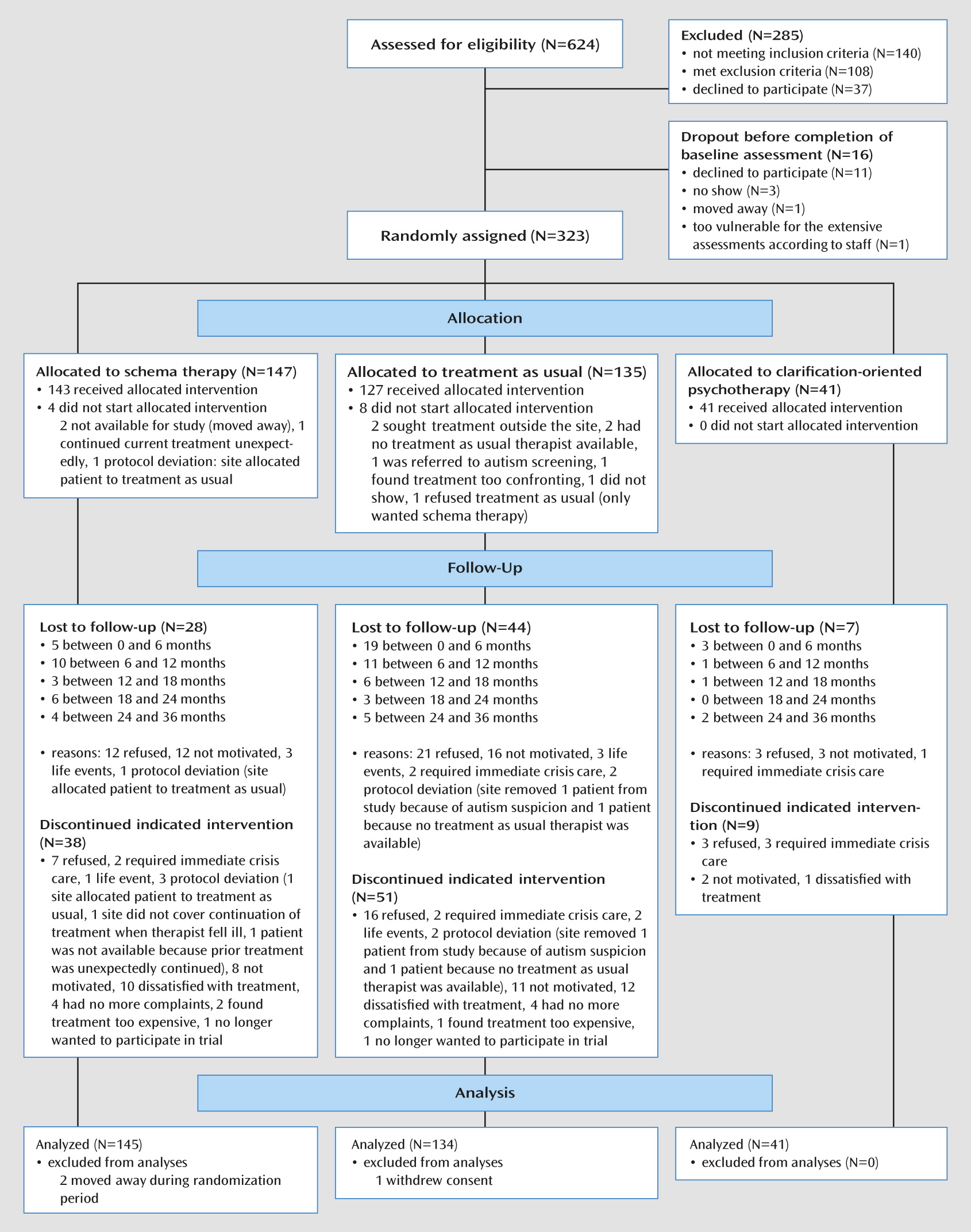
Patient Accrual
| Analysis and Contrast | Analysis | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|
| B | t | df | p | Exp(B)b | 95% CI | Estimated Proportion | 95% CI | |
| Primary analysis | ||||||||
| Recovery controlled for baseline severityc, d | ||||||||
| ST versus TAU | 1.404 | 3.326 | 314 | 0.001 | 4.073 | 1.774–9.350 | ||
| COP versus TAU | 0.334 | 0.725 | 314 | 0.47 | 1.397 | 0.564–3.459 | ||
| ST versus COP | 1.070 | 2.047 | 314 | 0.041 | 2.916 | 1.043–8.157 | ||
| Cohort-by-schema therapy | 2.120 | 2.520 | 314 | 0.012 | 8.334 | 1.592–43.631 | ||
| Severity | –1.178 | –5.252 | 314 | <0.001 | 0.308 | 0.198–0.479 | ||
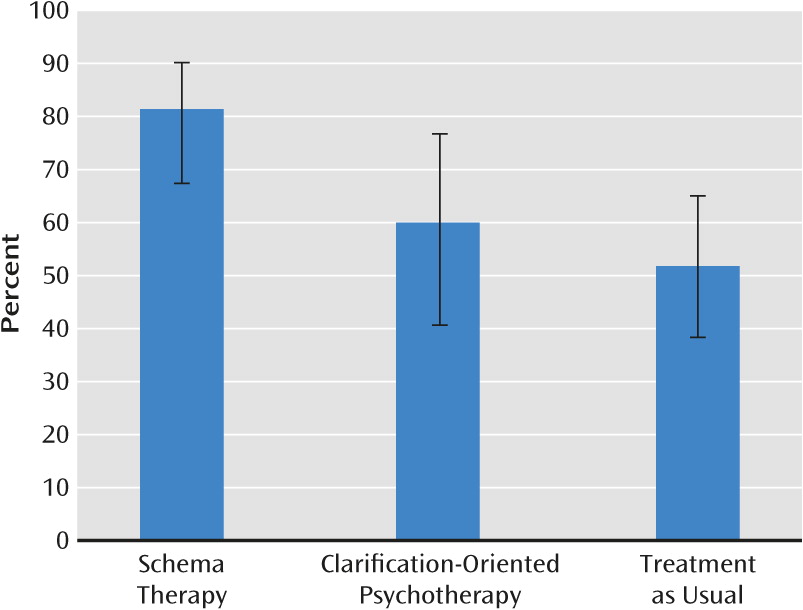
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.814 | 0.674–0.902 | ||||||
| Clarification-oriented psychotherapy | 0.600 | 0.406–0.767 | ||||||
| Treatment as usual | 0.518 | 0.383–0.650 | ||||||
| Sensitivity analysis | ||||||||
| Recovery not controlled for baseline severity | ||||||||
| ST versus TAU | 1.224 | 3.134 | 315 | 0.002 | 3.402 | 1.577–7.338 | ||
| COP versus TAU | 0.026 | 0.062 | 315 | 0.95 | 1.027 | 0.45–2.372 | ||
| ST versus COP | 1.198 | 2.471 | 315 | 0.014 | 3.313 | 1.276–8.601 | ||
| Cohort-by-schema therapy | 1.869 | 2.391 | 315 | 0.017 | 6.479 | 1.393–30.138 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.796 | 0.663–0.885 | ||||||
| Clarification-oriented psychotherapy | 0.541 | 0.364–0.708 | ||||||
| Treatment as usual | 0.534 | 0.409–0.654 | ||||||
| Recovery controlled for assessment timee | ||||||||
| ST versus TAU | 1.073 | 2.399 | 313 | 0.017 | 2.925 | 1.213–7.052 | ||
| COP versus TAU | –0.003 | –0.006 | 313 | >0.99 | 0.997 | 0.386–2.574 | ||
| ST versus COP | 1.076 | 1.999 | 313 | 0.046 | 2.933 | 1.017–8.458 | ||
| Cohort-by-schema therapy | 2.112 | 2.367 | 313 | 0.019 | 8.261 | 1.428–47.810 | ||
| Severity | –1.335 | –5.330 | 313 | <0.001 | 0.263 | 0.161–0.431 | ||
| Assessment time | 0.489 | 6.743 | 313 | <0.001 | 1.631 | 1.414–1.881 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.869 | 0.755–0.935 | ||||||
| Clarification-oriented psychotherapy | 0.694 | 0.503–0.835 | ||||||
| Treatment as usual | 0.694 | 0.558–0.804 | ||||||
| Recovery controlled for assessment typef | ||||||||
| ST versus TAU | 1.049 | 2.405 | 313 | 0.017 | 2.856 | 1.210–6.738 | ||
| COP versus TAU | 0.016 | 0.034 | 313 | 0.97 | 1.016 | 0.400–2.584 | ||
| ST versus COP | 1.033 | 1.952 | 313 | 0.05 | 2.810 | 0.992–7.958 | ||
| Cohort-by-schema therapy | 1.835 | 2.119 | 313 | 0.035 | 6.264 | 1.140–34.427 | ||
| Severity | –1.185 | –5.048 | 313 | <0.001 | 0.306 | 0.193–0.485 | ||
| Assessment type | 1.740 | 6.121 | 313 | <0.001 | 5.696 | 3.256–9.963 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.746 | 0.582–0.861 | ||||||
| Clarification-oriented psychotherapy | 0.511 | 0.320–0.699 | ||||||
| Treatment as usual | 0.507 | 0.373–0.639 | ||||||
| Recovery in subsample that started indicated treatment | ||||||||
| ST versus TAU | 1.298 | 3.071 | 304 | 0.002 | 3.664 | 1.594–8.418 | ||
| COP versus TAU | 0.226 | 0.496 | 304 | 0.62 | 1.254 | 0.511–3.075 | ||
| ST versus COP | 1.072 | 2.071 | 304 | 0.039 | 2.922 | 1.055–8.094 | ||
| Cohort-by-schema therapy | 2.289 | 2.712 | 304 | 0.007 | 9.864 | 1.873–51.932 | ||
| Severity | –1.185 | –5.201 | 304 | <0.001 | 0.306 | 0.195–0.479 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.819 | 0.684–0.904 | ||||||
| Clarification-oriented psychotherapy | 0.607 | 0.417–0.770 | ||||||
| Treatment as usual | 0.552 | 0.419–0.679 | ||||||
| Recovery defined by absence of subthreshold personality disorder (stringent criterion)g | ||||||||
| ST versus TAU | 1.410 | 3.436 | 314 | 0.001 | 4.096 | 1.827–9.185 | ||
| COP versus TAU | 0.454 | 1.012 | 314 | 0.31 | 1.574 | 0.652–3.800 | ||
| ST versus COP | 0.957 | 1.886 | 314 | 0.06 | 2.603 | 0.959–7.061 | ||
| Cohort-by-schema therapy | 2.219 | 2.713 | 314 | 0.007 | 9.202 | 1.840–46.018 | ||
| Severity | –0.979 | –4.612 | 314 | <0.001 | 0.376 | 0.248–0.571 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.789 | 0.645–0.885 | ||||||
| Clarification-oriented psychotherapy | 0.589 | 0.402–0.754 | ||||||
| Treatment as usual | 0.477 | 0.350–0.607 | ||||||
| Recovery controlled for personality disorder categoryh | ||||||||
| ST versus TAU | 1.428 | 3.374 | 311 | 0.001 | 4.172 | 1.814–9.597 | ||
| COP versus TAU | 0.342 | 0.741 | 311 | 0.46 | 1.408 | 0.568–3.490 | ||
| ST versus COP | 1.087 | 2.075 | 311 | 0.039 | 2.964 | 1.058–8.304 | ||
| Cohort-by-schema therapy | 2.164 | 2.567 | 311 | 0.011 | 8.709 | 1.658–45.753 | ||
| Severity | –1.215 | –5.335 | 311 | <0.001 | 0.297 | 0.190–0.465 | ||
| Dependent personality disorder | –0.075 | –0.174 | 311 | 0.86 | 0.928 | 0.399–2.160 | ||
| Obsessive-compulsive personality disorder | –0.410 | –1.354 | 311 | 0.18 | 0.664 | 0.366–1.204 | ||
| Paranoid, narcissistic, or histrionic personality disorder | –0.102 | –0.236 | 311 | 0.81 | 0.903 | 0.386–2.112 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.813 | 0.666–0.904 | ||||||
| Clarification-oriented psychotherapy | 0.594 | 0.395–0.766 | ||||||
| Treatment as usual | 0.510 | 0.367–0.651 | ||||||
| Recovery controlled for medication use at treatment start | ||||||||
| ST versus TAU | 1.420 | 3.352 | 313 | 0.001 | 4.136 | 0.180–0.458 | ||
| COP versus TAU | 0.355 | 0.771 | 313 | 0.44 | 1.427 | 0.576–3.533 | ||
| ST versus COP | 1.064 | 2.036 | 313 | 0.043 | 2.899 | 1.036–8.110 | ||
| Cohort-by-schema therapy | 2.072 | 2.456 | 313 | 0.015 | 7.937 | 1.511–41.667 | ||
| Severity | –1.248 | –5.256 | 313 | <0.001 | 0.287 | 0.180–0.458 | ||
| Medication use at treatment start | 0.264 | 0.969 | 313 | 0.33 | 1.302 | 0.762–2.223 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.817 | 0.678–0.904 | ||||||
| Clarification-oriented psychotherapy | 0.606 | 0.412–0.772 | ||||||
| Treatment as usual | 0.519 | 0.384–0.651 | ||||||
| Recovery controlled for medication use during 3 yearsi | ||||||||
| ST versus TAU | 1.416 | 3.343 | 313 | 0.001 | 4.120 | 1.791–9.478 | ||
| COP versus TAU | 0.342 | 0.741 | 313 | 0.459 | 1.408 | 0.568–3.492 | ||
| ST versus COP | 1.074 | 2.052 | 313 | 0.041 | 2.926 | 1.045–8.192 | ||
| Cohort-by-schema therapy | 2.114 | 2.511 | 313 | 0.013 | 8.280 | 1.580–43.383 | ||
| Severity | –1.200 | –5.146 | 313 | <0.001 | 0.301 | 0.190–0.477 | ||
| Medication use during trial | 0.107 | 0.344 | 313 | 0.731 | 1.113 | 0.602–2.057 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.815 | 0.675–0.903 | ||||||
| Clarification-oriented psychotherapy | 0.600 | 0.406–0.767 | ||||||
| Treatment as usual | 0.516 | 0.381–0.649 | ||||||
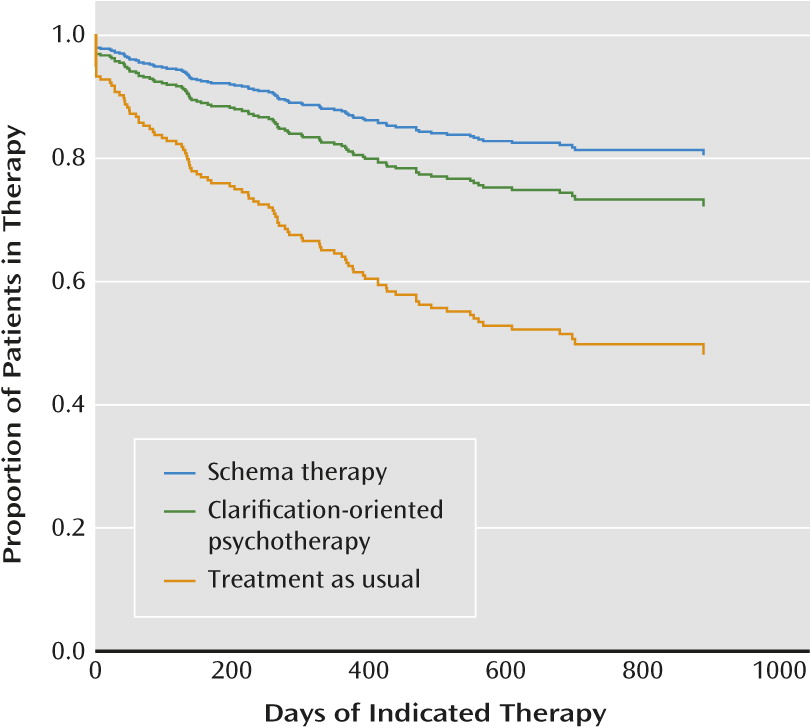
| Dropout analysis | ||||||||
| Dropout controlled for baseline severity | ||||||||
| ST versus TAU | –1.321 | –3.003 | 314 | 0.003 | 0.267 | 0.112–0.634 | ||
| COP versus TAU | –0.951 | –2.003 | 314 | 0.046 | 0.386 | 0.152–0.983 | ||
| ST versus COP | –0.370 | –0.654 | 314 | 0.51 | 0.691 | 0.227–2.103 | ||
| Cohort-by-schema therapy | –2.149 | –2.443 | 314 | 0.015 | 0.117 | 0.021–0.658 | ||
| Severity | 0.287 | 1.383 | 314 | 0.167 | 1.333 | 0.886–2.005 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.154 | 0.076–0.285 | ||||||
| Clarification-oriented psychotherapy | 0.208 | 0.103–0.376 | ||||||
| Treatment as usual | 0.405 | 0.294–0.527 | ||||||
| Dropout not controlled for baseline severity | ||||||||
| ST versus TAU | –1.309 | –2.984 | 315 | 0.003 | 0.270 | 0.114–0.640 | ||
| COP versus TAU | –0.878 | –1.901 | 315 | 0.06 | 0.416 | 0.168–1.031 | ||
| ST versus COP | –0.431 | –0.775 | 315 | 0.44 | 0.650 | 0.218–1.941 | ||
| Cohort-by-schema therapy | –2.137 | –2.435 | 315 | 0.015 | 0.118 | 0.021–0.663 | ||
| Follow-up at 3 years | ||||||||
| Schema therapy | 0.154 | 0.077–0.283 | ||||||
| Clarification-oriented psychotherapy | 0.219 | 0.112–0.384 | ||||||
| Treatment as usual | 0.402 | 0.296–0.519 | ||||||
Treatment Outcomes
Primary outcome.
Secondary outcomes.
| Analysis and Measure | Analysis | Effect Size | ||||||
|---|---|---|---|---|---|---|---|---|
| Mixed-regression repeated-measures analyses | B | 95% CI (B) | t | df | p | rb | dc | Within Conditiond |
| Global Assessment of Functioning Scale score | ||||||||
| Timee | 2.10 | 1.28 to 2.91 | 5.22 | 29.64 | <0.001 | 0.69 | 1.27 | |
| Time-by-condition | ||||||||
| ST versus TAU | 0.83 | 0.03 to 1.62 | 2.05 | 224.87 | 0.042 | 0.14 | 0.50 | |
| COP versus TAU | –0.27 | –1.43 to 0.90 | –0.46 | 135.56 | 0.65 | 0.04 | –0.16 | |
| ST versus COP | 1.09 | –0.04 to 2.22 | 1.92 | 126.62 | 0.057 | 0.17 | 0.66 | |
| Time-by-cohort-by-schema therapy | 1.77 | 0.18 to 3.35 | 2.20 | 224.49 | 0.029 | 0.15 | 0.53 | |
| Change over 3 years | ||||||||
| Schema therapy | 1.76 | |||||||
| Clarification-oriented psychotherapy | 1.11 | |||||||
| Treatment as usual | 1.27 | |||||||
| Social and Occupational Functioning Assessment score | ||||||||
| Timee | 1.97 | 1.13 to 2.81 | 4.82 | 25.89 | <0.001 | 0.69 | 1.05 | |
| Time-by-condition | ||||||||
| ST versus TAU | 1.12 | 0.35 to 1.89 | 2.87 | 217.61 | <0.005 | 0.19 | 0.60 | |
| COP versus TAU | –0.17 | –1.34 to 0.99 | –0.29 | 138.32 | 0.77 | 0.02 | –0.09 | |
| ST versus COP | 1.29 | 0.15 to 2.42 | 2.26 | 128.91 | 0.025 | 0.20 | 0.69 | |
| Time-by-cohort-by schema therapy | 1.44 | –0.10 to 2.99 | 1.85 | 217.21 | 0.066 | 0.12 | 0.39 | |
| Change over 3 years | ||||||||
| Schema therapy | 1.65 | |||||||
| Clarification-oriented psychotherapy | 0.96 | |||||||
| Treatment as usual | 1.05 | |||||||
| Symptom Checklist-90 scoref | ||||||||
| Timee | –0.143 | –0.186 to –0.101 | –6.77 | 50.05 | <0.001 | 0.69 | 0.95 | |
| Time-by-condition | ||||||||
| ST versus TAU | 0.004 | –0.047 to 0.055 | 0.14 | 265.16 | 0.89 | 0.01 | –0.02 | |
| COP versus TAU | –0.027 | –0.097 to 0.043 | –0.77 | 105.34 | 0.45 | 0.07 | 0.18 | |
| ST versus COP | 0.031 | –0.037 to 0.098 | 0.90 | 100.87 | 0.37 | 0.09 | –0.20 | |
| Time-by-cohort-by-schema therapy | –0.059 | –0.160 to 0.043 | –1.14 | 264.72 | 0.26 | 0.07 | 0.19 | |
| Change over 3 years | ||||||||
| Schema therapy | 0.93 | |||||||
| Clarification-oriented psychotherapy | 1.13 | |||||||
| Treatment as usual | 0.95 | |||||||
| Assessment of DSM-IV Personality Disorders Questionnaire trait scoref | ||||||||
| Timee | –0.157 | –0.200 to –0.114 | –7.39 | 35.90 | <0.001 | 0.78 | 1.14 | |
| Time-by-condition | ||||||||
| ST versus TAU | 0.039 | –0.012 to 0.091 | 1.50 | 261.34 | 0.14 | 0.09 | –0.28 | |
| COP versus TAU | –0.001 | –0.152 to 0.054 | –0.04 | 80.57 | 0.97 | 0.00 | 0.01 | |
| ST versus COP | 0.04 | –0.028 to 0.109 | 1.18 | 77.01 | 0.24 | 0.13 | –0.29 | |
| Time-by-cohort-by-schema therapy | –0.049 | –0.152 to 0.054 | –0.93 | 260.58 | 0.35 | 0.06 | 0.18 | |
| Change over 3 years | ||||||||
| Schema therapy | 0.86 | |||||||
| Clarification-oriented psychotherapy | 1.13 | |||||||
| Treatment as usual | 1.14 | |||||||
| Work and Social Adjustment Scale score | ||||||||
| Timee | –1.19 | –1.75 to –0.63 | –4.34 | 29.49 | <0.001 | 0.62 | 0.77 | |
| Time-by-condition | ||||||||
| ST versus TAU | –0.16 | –0.72 to 0.40 | –0.56 | 249.18 | 0.57 | 0.04 | 0.10 | |
| COP versus TAU | –0.31 | –1.14 to 0.51 | –0.75 | 133.65 | 0.45 | 0.06 | 0.20 | |
| ST versus COP | 0.15 | –0.64 to 0.95 | 0.38 | 124.29 | 0.71 | 0.03 | –0.10 | |
| Time-by-cohort-by-schema therapy | –0.52 | –1.64 to 0.60 | –0.91 | 248.74 | 0.36 | 0.06 | 0.17 | |
| Change over 3 years | ||||||||
| Schema therapy | 0.87 | |||||||
| Clarification-oriented psychotherapy | 0.97 | |||||||
| Treatment as usual | 0.77 | |||||||
| Mixed-regression repeated-measures analyses | B | 95% CI (B) | t | df | p | rb | dc | Within Conditiond |
| Miskimins Self-Goal-Other Discrepancy Scale scoref | ||||||||
| Timee | –0.171 | –0.211 to –0.131 | –8.64 | 39.99 | <0.001 | 0.81 | 1.32 | |
| Time-by-condition | ||||||||
| ST versus TAU | 0.006 | –0.041 to 0.053 | 0.25 | 256.34 | 0.80 | 0.02 | –0.05 | |
| COP versus TAU | –0.024 | –0.089 to 0.041 | –0.73 | 107.40 | 0.47 | 0.07 | 0.18 | |
| ST versus COP | 0.030 | –0.033 to 0.093 | 0.95 | 100.52 | 0.35 | 0.09 | –0.23 | |
| Time-by-cohort-by-schema therapy | –0.101 | –0.195 to –0.007 | –2.12 | 255.65 | 0.035 | 0.13 | 0.78 | |
| Change over 3 years | ||||||||
| Schema therapy | 1.27 | |||||||
| Clarification-oriented psychotherapy | 1.55 | |||||||
| Treatment as usual | 1.32 | |||||||
| World Health Organization Quality of Life Assessment scoreg | ||||||||
| Timee | 10.14 | 7.14 to 13.14 | 6.83 | 40.44 | <0.001 | 0.73 | 1.04 | |
| Time-by-condition | ||||||||
| ST versus TAU | –0.60 | –4.03 to 2.82 | –0.35 | 255.43 | 0.73 | 0.02 | –0.06 | |
| COP versus TAU | 1.44 | –3.36 to 6.24 | 0.60 | 115.86 | 0.55 | 0.06 | 0.15 | |
| ST versus COP | –2.04 | –6.70 to 2.61 | –0.87 | 110.08 | 0.39 | 0.08 | –0.21 | |
| Time-by-cohort-by-schema therapy | 3.12 | –3.73 to 9.96 | 0.90 | 254.98 | 0.37 | 0.06 | 0.16 | |
| Change over 3 years | ||||||||
| Schema therapy | 0.98 | |||||||
| Clarification-oriented psychotherapy | 1.19 | |||||||
| Treatment as usual | 1.04 | |||||||
| Multiple imputation logistic regression analysesh | B | SE(B) | p | Odds Ratio | 95% CI | Estimated Proportion | ||
| Depressive disorders (at 3 years) | ||||||||
| Baseline depressive disorder | 1.94 | 2.41 | 0.46 | 6.95 | 0.01–3868.76 | |||
| Severity | 1.08 | 0.82 | 0.24 | 2.94 | 0.40–21.69 | |||
| ST versus TAU | –1.45 | 0.68 | 0.033 | 0.23 | 0.06–0.89 | |||
| COP versus TAU | –1.83 | 1.43 | 0.23 | 0.16 | 0.01–3.70 | |||
| ST versus COP | 0.37 | 1.30 | 0.78 | 1.45 | 0.10–21.93 | |||
| Cohort-by-schema therapy | –2.00 | 1.32 | 0.13 | 0.14 | 0.01–1.81 | |||
| Presence at follow-up by conditioni | ||||||||
| Schema therapy | 0.135 | |||||||
| Clarification-oriented psychotherapy | 0.122 | |||||||
| Treatment as usual | 0.252 | |||||||
| Anxiety disorders (any at 3 years) | ||||||||
| Number of baseline anxiety disorders | 0.32 | 0.69 | 0.67 | 1.37 | 0.224–8.40 | |||
| Severity | 0.83 | 0.42 | 0.066 | 2.30 | 0.94–5.65 | |||
| ST versus TAU | 0.09 | 0.64 | 0.89 | 1.10 | 0.27–4.44 | |||
| COP versus TAU | 0.03 | 0.72 | 0.97 | 1.03 | 0.25–4.22 | |||
| ST versus COP | 0.07 | 0.78 | 0.93 | 1.07 | 0.23–5.09 | |||
| Cohort-by-schema therapy | –0.87 | 1.31 | 0.52 | 0.42 | 0.02–7.41 | |||
| Presence at follow-up by conditioni | ||||||||
| Schema therapy | 0.275 | |||||||
| Clarification-oriented psychotherapy | 0.351 | |||||||
| Treatment as usual | 0.274 | |||||||
Discussion
Schema Therapy
Acknowledgments
Footnote
Supplementary Material
- View/Download
- 312.64 KB
References
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

