Electrocardiogram (ECG) is the primary tool for detecting long QT syndrome, the most common cause of marketed drug withdrawal (
1) and a surrogate marker for the propensity to develop specific ventricular arrhythmias called torsade de pointes. The term was coined in 1966 to describe a malignant polymorphic ventricular tachycardia characterized by a twisting pattern of the QRS complex (
2). The probability of torsade de pointes increases with the extent of heart rate-corrected QT (QTc) prolongation, but no threshold has been established below which the risk can be considered absent. Most torsade de pointes episodes are transient and self-limited. The transition probability to sudden death may be distributed between 1% and 17%, a wide range that reflects uncertainty around the estimate (
3). In spite of methodological heterogeneity across studies, a recent meta-analysis reported consistent associations between prolonged QT interval and both increased total mortality and sudden cardiac death (
4).
QT interval prolongation occurs with noncardiac medications, particularly antipsychotic drugs (
5). Epidemiological studies indicate that the propensity of torsade de pointes and fatal outcome increases with the dosage of conventional and atypical antipsychotics (
6), as well as antidepressants, mood stabilizers, and methadone (
7). In a large study based on Medicaid data, users and nonusers of antipsychotic drugs were followed for the occurrence of sudden cardiac death; users of either conventional or atypical antipsychotics had higher rates of sudden cardiac death than nonusers, with incidence rate ratios of 1.99 and 2.26, respectively (
8). Furthermore, administration of QT-prolonging drugs appears more likely to generate ventricular arrhythmias if associated with exacerbating conditions that are commonly observed in hospitalized patients (
9). Well-documented risk factors for drug-induced torsade de pointes include older age, female sex, electrolyte abnormalities, renal or hepatic dysfunction, preexisting heart disease (e.g., infarction), bradycardia or rhythms with pauses, treatment with more than one QT-prolonging drug, and genetic predisposition (
9,
10).
The ECG Screening Outcome in Psychiatry (ESOP) study reviewed all ECG recordings performed at hospital admission for psychiatric inpatients over a 5-year period. Its objectives were to determine the prevalence of drug-induced long QT and to identify associated factors based on pharmacovigilance data.
Results
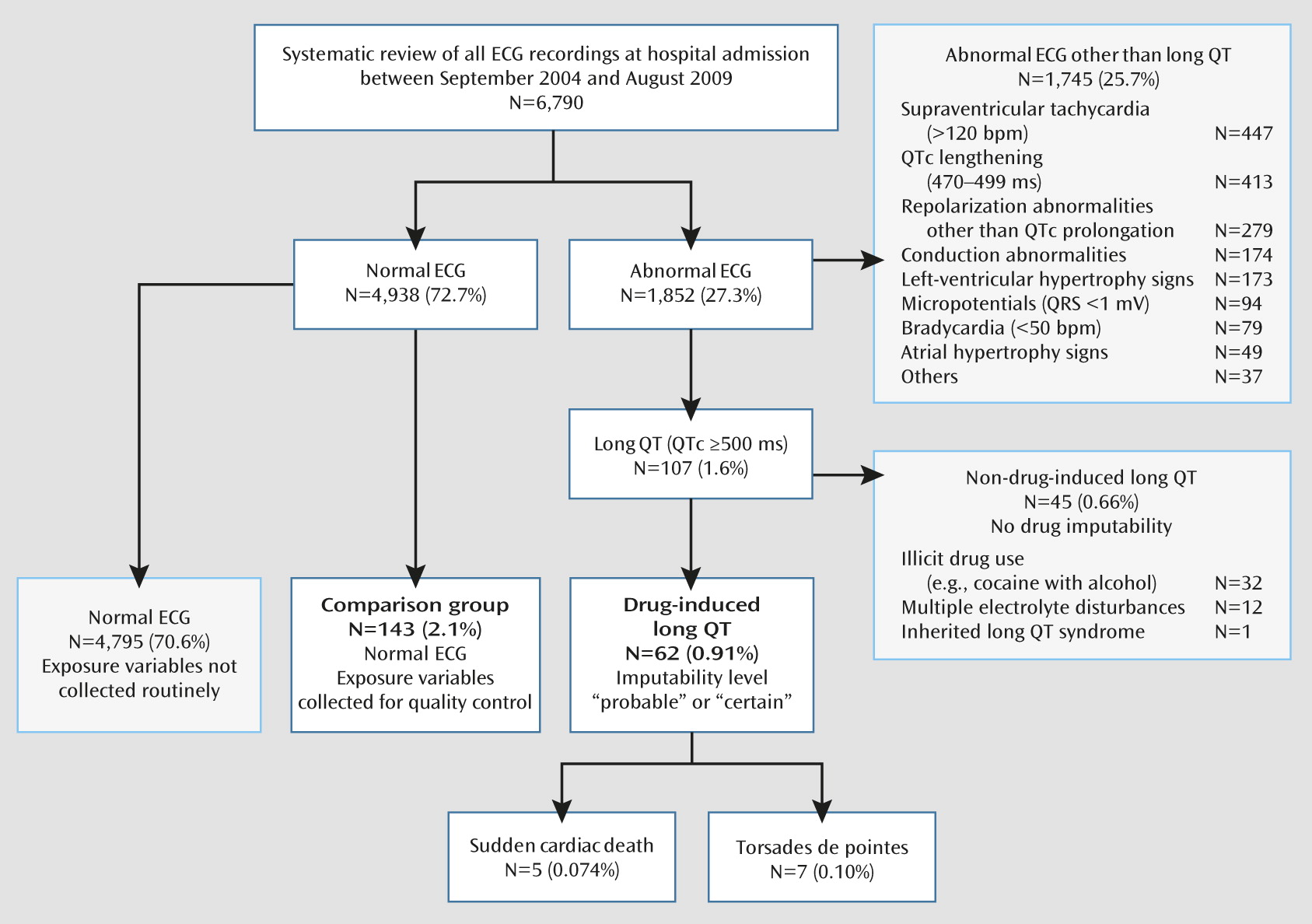
The study flowchart is illustrated in
Figure 1. Of 6,790 ECG recordings, 27.3% were abnormal. Long QT was diagnosed in 107 patients (1.6%), of whom 62 (0.9%) met criteria for drug-induced long QT, with probable or certain drug imputability according to World Health Organization–Uppsala Monitoring Centre criteria.
Sudden death was recorded in five patients and torsade de pointes in seven patients within 72 hours following drug-induced long QT detection, indicating that a time relationship was plausible (
Table 1). Although these events were rare (<0.2% of the entire sample with ECG recordings at admission), they represented 19.4% of patients identified with drug-induced long QT. Eleven of these 12 patients had concomitant T wave abnormalities, and seven had received methadone. All torsade de pointes patients recovered after drug de-challenge.
Patients with drug-induced long QT did not differ significantly from patients with normal ECG with respect to age, sex, obesity, cardiovascular risk factors, and coronary heart disease (
Table 2). In contrast, drug-induced long QT patients had significantly higher frequencies of hypokalemia (19.4% compared with 5.6%, p=0.004), HCV infection (41.9% compared with 9.8%, p=0.001), HIV infection (24.2% compared with 6.3%, p=0.001), and abnormal T wave morphology (35.5% compared with 15.4%, p=0.003).
The association between prolonged QTc interval and drugs prescribed to at least 10 patients was first investigated with univariate statistics (
Table 3). The antipsychotics clotiapine (a dibenzothiazepine, not marketed in the United States), haloperidol, phenothiazines (promazine and levomepromazine), and sertindole were significantly more frequent among drug-induced long QT patients, but no difference was observed for aripiprazole, clozapine, olanzapine, quetiapine, and risperidone (including paliperidone). The serotonin-selective reuptake inhibitors citalopram (including escitalopram) and fluoxetine were significantly associated with drug-induced long QT, unlike trazodone and venlafaxine. Prolonged QTc was significantly associated with methadone, which was the most frequent drug among patients with drug-induced long QT (37.1%). A significant inverse association was found for flurazepam, which was less frequent in the prolonged QTc sample than in the comparison group. Other benzodiazepines and drugs such as zolpidem, lamotrigine, valproic acid, biperiden, and omeprazole were not associated with drug-induced long QT.
In a multivariate model adjusted for hypokalemia (odds ratio=6.5, p=0.005), HCV infection (odds ratio=4.4, p=0.009), HIV infection (odds ratio=3.9, p=0.036), and abnormal T wave morphology (odds ratio=4.0, p=0.004), the drugs haloperidol, clotiapine, phenothiazines, and citalopram (including escitalopram) remained significantly associated with drug-induced long QT, whereas sertindole, fluoxetine, and methadone did not, despite adjusted odds ratios above 3 (p<0.10;
Table 3). The correlation matrix of estimated coefficients did not reveal any multicollinearity problem, despite expected associations between some predictors (e.g., HCV infection, HIV, and methadone prescription). No other drug was significantly associated with long QT when added into the multivariate model.
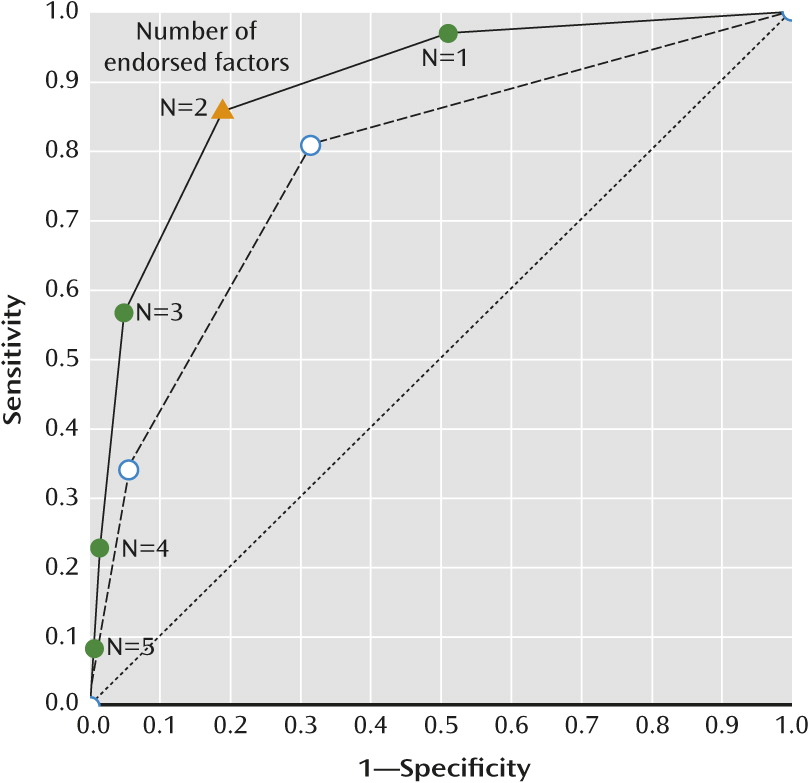
Considering the four clinical factors (hypokalemia, HCV infection, HIV, and abnormal T wave morphology) and the seven drugs associated with drug-induced long QT (clotiapine, haloperidol, phenothiazines, sertindole, citalopram, fluoxetine, and methadone), we counted the number of factors endorsed by each individual patient (median=1, range=0–5 in normal ECG patients; median=3, range=0–5 in long QT patients). As illustrated in
Figure 2, the area under the receiver operating characteristic curve was 0.89 (95% CI=0.84–0.94) when taking into account clinical conditions and medication and 0.78 (95% CI=0.71–0.84) when only clinical conditions were counted (p<0.001). Whereas 81.1% of patients with normal ECG endorsed fewer than two factors (specificity), 85.5% of patients with drug-induced long QT endorsed two or more factors (sensitivity).
Discussion
In this 5-year study, 6,790 patients had a routine ECG at admission to the psychiatric hospital. Prevalence of drug-induced long QT (QTc >500 ms and probable or certain drug imputability) was 0.9%, in agreement with previous studies that reported prevalence rates between 1.2% and 2.6% (
16–
18). Almost 20% of patients in whom drug-induced long QT was detected were subsequently documented for torsade de pointes (N=7) and sudden death (N=5). Because seven of these 12 patients were prescribed methadone for opioid substitution, a possible role of illicit drug use cannot be ruled out. Nevertheless, this observation emphasizes that the detection of a QTc interval >500 ms at admission to the psychiatric hospital should lead to prompt action, including discontinuation of the offending drug unless the benefits of treatment clearly outweigh the risk, correction of electrolyte disturbances, and careful cardiac monitoring (
19).
The ESOP study indicated significant associations between drug-induced long QT and clinical conditions, such as hypokalemia, HIV, and HCV infection, and concomitant ECG features, such as morphological T wave abnormalities. Hypokalemia is the most common electrolyte abnormality in clinical practice, with potassium values <3.6 mmol/L in over 20% of inpatients (
20). It is a well-known risk factor for torsade de pointes (
9).
In HIV-infected individuals, high viral load and low CD4+ cell count (cutoff values, 17,900 copies/mL and 144 cells/mm
3, respectively) were associated with QT lengthening (
21). Autonomic neuropathy was reported as a possible explanation (
22). Another mechanism might be through the HIV Tat protein, which inhibits human ether-a-go-go-related gene (hERG) potassium channels (
23). A large cross-sectional study in HIV-infected patients revealed no significant effect of anti-HIV medication on QTc (
24).
HCV infection frequently causes impaired liver function, which is a documented risk factor for long QT because of the increased likelihood of drug-drug interactions. HCV infection nearly doubled the propensity of QTc ≥470 ms in patients with concurrent HIV infection (29.6% compared with 15.8%) (
25). Furthermore, HCV-triggered liver-kidney-microsomal type 1 antibodies (LKM−1) are associated with reduced CYP2D6 activity (
26), a crucial metabolic pathway for many antipsychotics and antidepressants. The effects of HIV and HCV infections most likely encompass indirect effects as well, through uncontrolled variables such as injection drug use and risk behaviors.
In addition to QTc interval, T wave morphology descriptors are valuable covariates in cardiac safety trials. Basic (peak amplitude and area under the curve) and advanced descriptors (notch, asymmetry, and flatness) are sensitive to drug-induced alterations (
27,
28). T-U wave distortion, T wave alternans, and new-onset ventricular ectopies are further ECG features promoting arrhythmias by increasing the heterogeneity of repolarization across the myocardial wall (
13). A composite score of T wave morphology, either alone or in combination with the QT interval, allowed efficient discrimination between normal and abnormal repolarization (
29).
The ESOP study examined 23 drugs for a possible association with drug-induced long QT. Seven drugs were associated with QTc >500 ms (odds ratio >3), of which five had been previously documented for conditional, possible, or actual risk of torsade de pointes and two showed structural and pharmacological similarities to QT-prolonging drugs (
Table 3).
A previous study in methadone maintenance patients indicated that QT lengthening was dosage-dependent and increased with concomitant administration of CYP3A4 inhibitors, hypokalemia, and impaired liver function (
11). A modeling approach using pooled data from five clinical trials supported the need for ECG monitoring and arrhythmia risk assessment in patients receiving methadone dosages greater than 120 mg/day (
30). Substitution of racemic methadone with the R-methadone enantiomer, which mainly mediates the opioid effect, was associated with reduced QTc interval and thus safer cardiac profile (
31).
The antipsychotic haloperidol is associated with an increased risk of torsade de pointes, particularly for intravenous administration and at high dosage (
32). As far as we know, promazine and levomepromazine have not been associated with QT prolongation. However, these phenothiazines have properties similar to chlorpromazine and thioridazine, for which cases of ventricular arrhythmias and torsade de pointes have been reported (
33). Thus, similar caution may apply for these different drugs. To our knowledge, QT prolongation had not been documented for clotiapine, an atypical antipsychotic agent with a dibenzothiapine structure and properties similar to those of phenothiazines. The present study suggests that risk of drug-induced long QT with clotiapine might be of the same order of magnitude as for phenothiazines and haloperidol. Sertindole is associated with a possible risk of torsade de pointes. However, a multicenter postmarketing surveillance study indicated that QT interval prolongation might not translate into increased overall mortality (
34).
The antidepressants citalopram and escitalopram (its
S-enantiomer) increase QTc in a dose-dependent manner at therapeutic dosages (
35), leading to a safety announcement by the U.S. Food and Drug Administration, updated in March 2012 (
http://www.fda.gov/Drugs/DrugSafety/ucm297391.htm). Fluoxetine has been associated with QTc prolongation and torsade de pointes in case reports (
36). It is a potent inhibitor of CYP2D6, and pharmacokinetic interactions may result in a synergistic effect on QTc prolongation when fluoxetine is taken with QT-prolonging CYP2D6 substrates.
Exploratory multivariable analysis suggested that all four clinical conditions (hypokalemia, HCV infection, HIV, and abnormal T wave morphology) and seven drugs (clotiapine, haloperidol, phenothiazines, sertindole, citalopram, fluoxetine, and methadone) may independently contribute to drug-induced long QT. The analysis emphasized that drug-induced long QT may depend on the co-occurrence of several risk factors. Indeed, we observed that more than 85% of patients with drug-induced long QT endorsed two or more factors, as compared with less than 20% in the comparison group. This observation is in line with a review of 249 cases of torsade de pointes as a result of noncardiac medication (
37).
Strengths of the ESOP study include a systematic review of a large number of ECG recordings at admission to the psychiatric hospital over a 5-year period. Long QT is a rare event and such a survey allowed us to identify a relatively large sample that had been thoroughly documented as part of an ongoing pharmacovigilance program.
Nonetheless, some limitations need to be acknowledged. First, cross-sectional design provides no information about the temporal relationship between exposure and outcome and does not allow risk estimation and further causality assessment. Second, the comparison sample may not have been representative of all patients admitted in the 2004–2009 period. A selection bias cannot be excluded, due to medication withdrawal from the market (thioridazine in 2005), drug reintroduction (sertindole in 2006), increased use of generic drugs (e.g., citalopram, clozapine, and lithium salts), and evolving prescription patterns. A third limitation is sample size. The lack of routinely collected reliable data did not allow us to include the entire population with ECG results at hospital admission or to select a larger random sample of patients with normal ECG. Furthermore, the small numbers of patients taking some drugs resulted in limited statistical power to detect their possible associations with long QT and uncertainty in estimating effect size, as reflected by wide confidence intervals in
Table 3. Sample size also prevented investigating possible dosage-related effects and interactions between different factors. Fourth, associations based on data collected in hospital settings may not reflect associations in the general population because of admission rate bias, sometimes called Berkson’s fallacy (
38). This bias would occur if exposure (e.g., psychotropic medication) was associated with hospitalization rate on its own right, which cannot be fully excluded. Using QTc >500 ms as a single outcome variable may be considered a fifth limitation. Although an absolute threshold has not been established, a cutoff at 500 ms is widely accepted as indicative of a high risk for arrhythmic events. Finally, it should be emphasized that the complex interplay between the different factors responsible for QT prolongation deserves further investigation in large samples. Whereas some degree of collinearity between the investigated factors was possible in the present study, additional risk factors (e.g., hypomagnesemia) or possible confounders (e.g., illicit drug use) were not taken into account. In addition, some psychotropic drugs were not investigated for QT prolongation because they were rarely prescribed (e.g., amisulpride) or unavailable in Switzerland (e.g., ziprasidone).
The American Heart Association and the American College of Cardiology Foundation published a scientific statement in order to raise awareness about risk factors, ECG monitoring, and managing drug-induced long QT in hospital settings (
9). Incidence of sudden cardiac death in patients taking antipsychotic medication is about 2.9 events per 1,000 patient-years (
39), as compared with 0.2 events per 1,000 patient-years for death from clozapine-induced agranulocytosis (
40). Yet no formal risk-management program has been established to detect prolonged QT at the psychiatric hospital, in contrast with white blood cell count monitoring for clozapine prescription. While the ESOP study speaks in favor of ECG surveillance in psychiatric inpatients, in particular when several QT-prolonging drugs and clinical conditions are identified, the cost-utility of a formal detection program deserves further analysis.