Development of Schizoaffective Psychosis in the Course of a Long-Term Occupation as Spiritual Healer: Coincidence or Causality?
Abstract
Case Presentation
All human beings are surrounded by an aura, which appears as a radiant energy field including several energy centers, the so-called chakras. They shine in different colors depending on the individual’s personality and mood. The healer is able to perceive these auras by her third eye chakra, which is located between the eyebrows. It serves as a channel between the healer’s mind and his surroundings. In order to activate it, the healer has to reach an intense state of trance by concentrated meditation.
Discussion
Culture-Sensitive Differential Diagnosis
| Features Suggesting Nonpathological Experiences | Features of our Patient |
|---|---|
| Lack of suffering | Suffering from the change in her experience |
| Lack of social or functional impairment | Severe cognitive and functional impairment |
| Compatibility with the patient’s cultural background; recognition by others | Experiences assessed as incompatible with the regular practice of spiritual healing |
| Absence of psychiatric comorbidities | Depressive symptoms, negative symptoms |
| Control over the experience | Loss of control over spiritual experiences |
| Personal growth over time | Decline of personal, social, and cognitive skills |
Exceptional Features
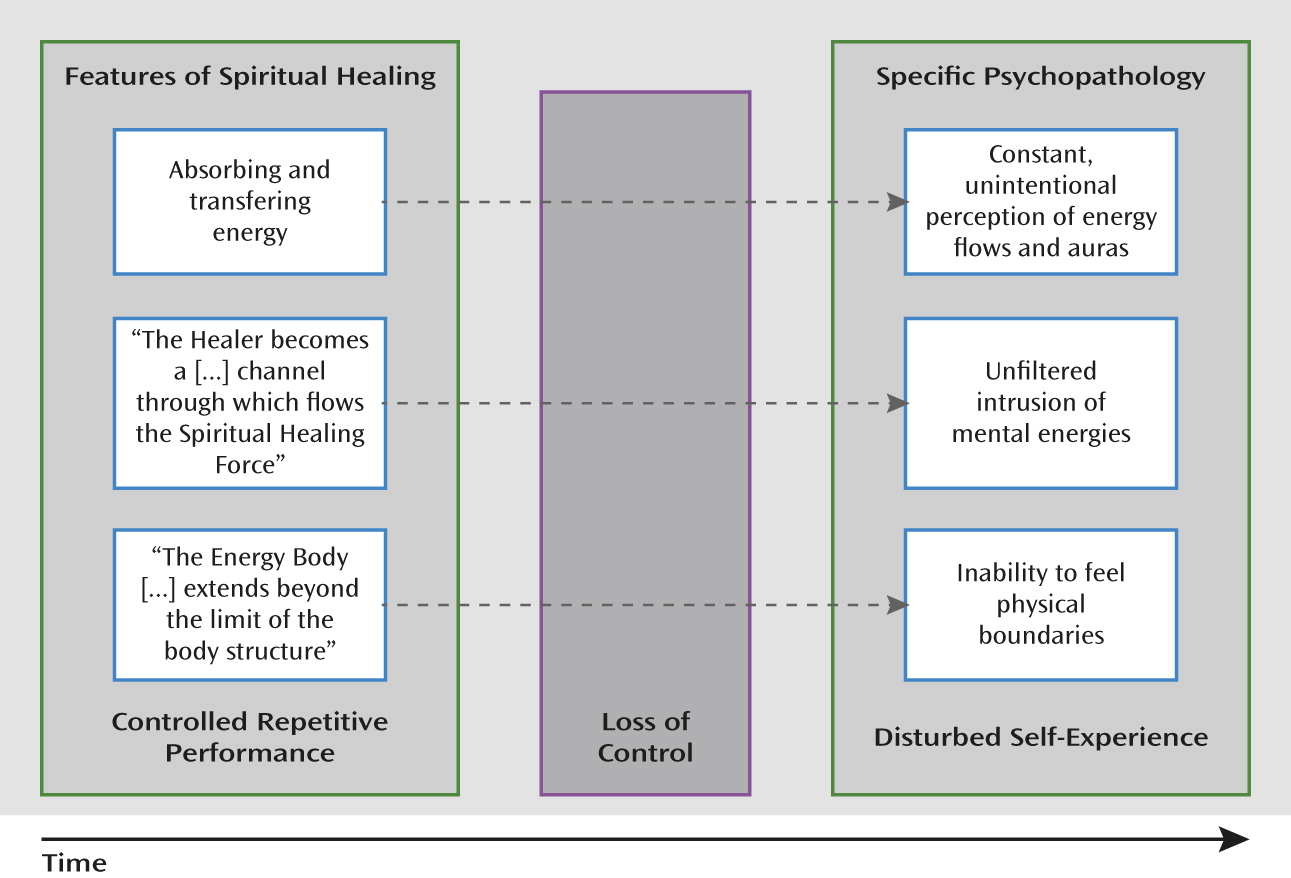
A Causal Link Between Spiritual Healing and Psychosis?
Conclusions
References
Information & Authors
Information
Published In
History
Authors
Author Contributions
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

