Low-Intensity Transcranial Current Stimulation in Psychiatry
Abstract
Section 1: Electrical Engineering and Neurophysiology
Spatial Targeting: Electrode Montages
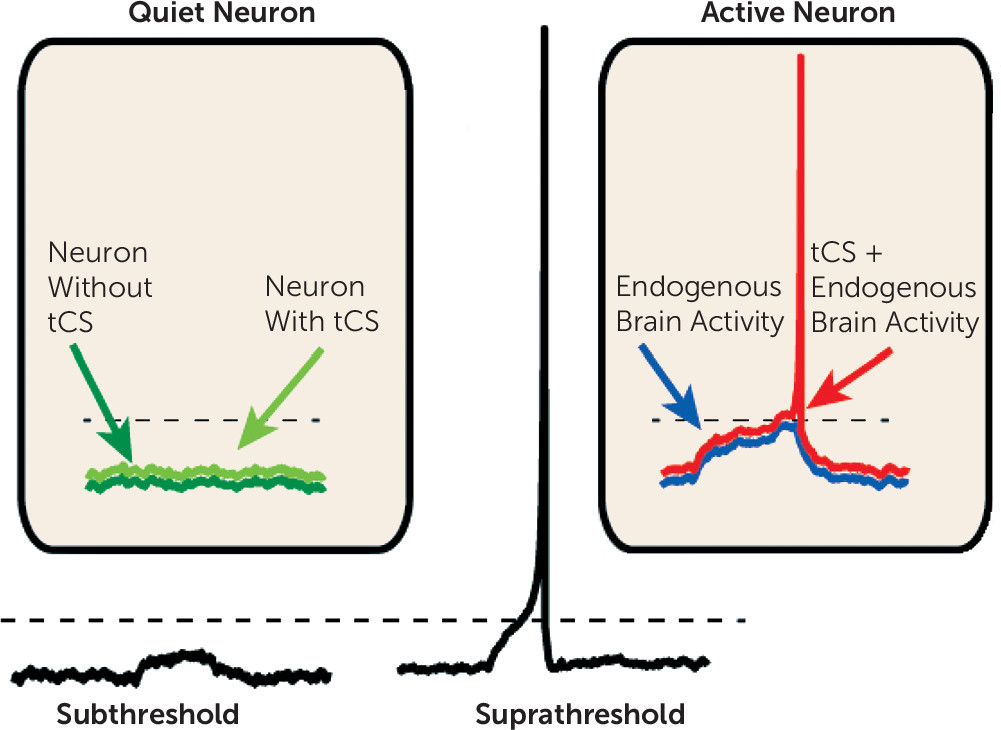
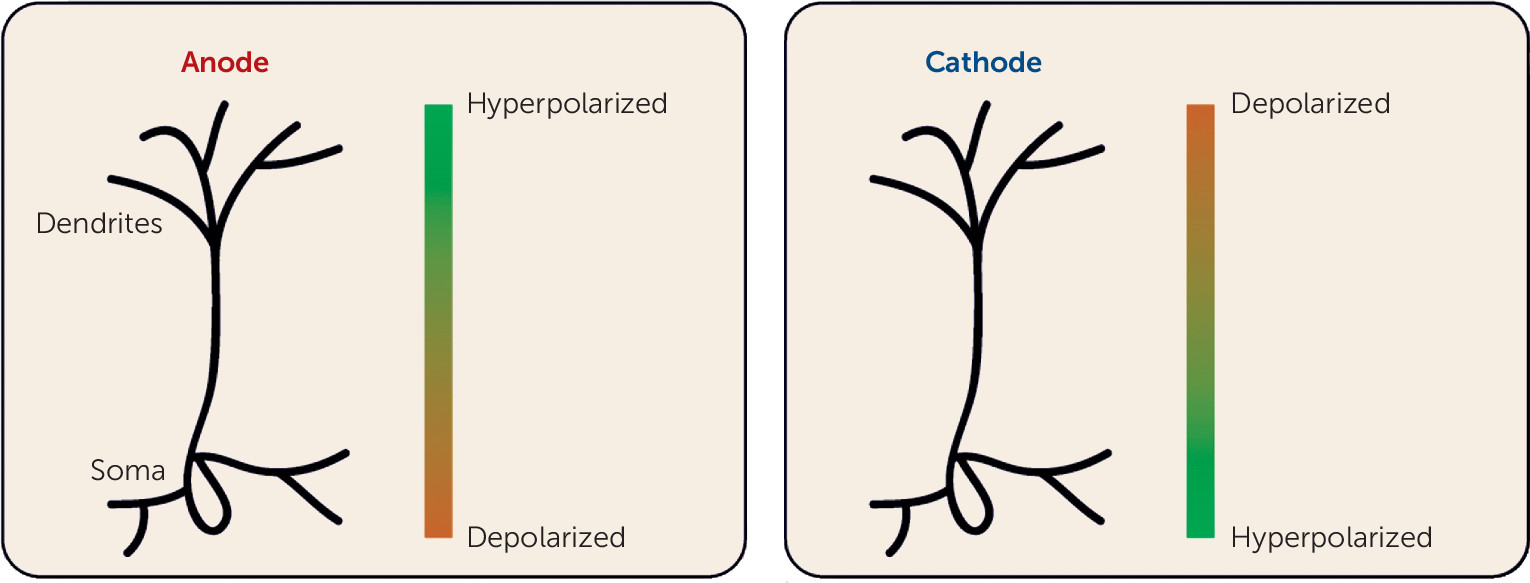
Neurophysiological Effects of tCS
Section 2: Review of Published Randomized Controlled Trials
Randomized Controlled Trials and Meta-Analyses of tCS for Major Depression
| Stimulation Type and Study | N per Group | Anatomical Target(s) | Stimulation Strength | Session Duration and Frequency (Total Sessions) | Main Findingsb | Quality Score (%)c |
|---|---|---|---|---|---|---|
| Transcranial direct current stimulation (tDCS) | ||||||
| Bennabi et al., 2015 (21) | Sham 12 Active 12 Total 24 | L DLPFC | 2 mA | 30 min twice/day for 5 days (10) | No difference between active and sham tDCS in depression | 68 |
| Blumberger et al., 2012 (22) | Sham 11 Active 13 Total 24 | L DLPFC | 2 mA | 20 min/day, 5 times/wk for 3 wk (15) | No difference in depression remission between active and sham tDCS | 74 |
| Boggio et al., 2008 (23) | Sham 10 Active control 9 Active 21 Total 40 | L DLPFC | 2 mA | 20 min/day, 5 times/wk for 10 days (10) | Active stimulation reduced depressive symptoms | 68 |
| Brunoni et al., 2013 (4) | PBO/sham 30 Sert/sham 30 PBO/active 30 Sert/active 30 Total 120 | L DLPFC | 2 mA | 30 min/day, 5 times per wk for 2 wk, then 2 sessions every other wk (12) | Sert/active tDCS superior to sert/sham, PBO/active, and PBO/sham groups | 89 |
| Brunoni et al., 2014 (24) | Therapy/sham 17 Therapy/active 20 Total 37 | L DLPFC | 2 mA | 30 min/day for 10 days (10) | No difference between active and sham tDCS in depression | 79 |
| Fregni et al., 2006 (25) | Sham 5 Active 5 Total 10 | L DLPFC | 1 mA | 20 min/day for 5 alternate days (5) | Active tDCS reduced depressive symptoms | 32 |
| Loo et al., 2010 (26) | Sham 20 Active 20 Total 40 | L DLPFC | 1 mA | 20 min/day, 3 times per wk (M/W/F) for 5 sessions (5) | No difference between active and sham tDCS in depression | 79 |
| Loo et al., 2012 (27) | Sham 31 Active 33 Total 64 | L DLPFC | 2 mA | 20 min/day, 5 days per wk for 3 wk (15) | Active tDCS reduced depressive symptoms | 89 |
| Palm et al., 2012 (28) | Sham 11 Active 11 Total 22 | L DLPFC | 1–2 mA | 20 min/day, 5 days per wk for 4 wk (20) | No difference between active and sham tDCS in depression | 74 |
| Segrave et al., 2014 (5) | Therapy/active 9 Therapy/sham 9 Sham therapy/active 9 Total 27 | L DLPFC | 2 mA | 24 min/day for 5 sessions (5) | Active tDCS reduced depressive symptoms | 68 |
| Vanderhasselt et al., 2015 (29) | Sham 14 Active 19 Total 33 | L DLPFC | 2 mA | 30 min/day for 10 sessions (10) | No difference between active and sham tDCS in depression | 53 |
| Cranial electrical stimulation (CES) | ||||||
| Barclay et al., 2014 (30) | Sham 55 Active 60 Total 115 | Cortex | 100 μA, 0.5 Hz | 1 hr/day, 5 days/wk for 5 wk (25) | Active CES reduced anxiety and depressive symptoms | 63 |
| Lyon et al., 2015 (31) | Sham 81 Active 82 Total 163 | Cortex | 100 µA, 0.5 Hz | 1 hr/day, 7 days/wk for 2 wk (14) | No difference between active and sham CES in depression | 63 |
| Mischoulon et al., 2015 (32) | Sham 13 Active 17 Total 30 | DLPFC | 1–4 µA | 20 min/day, 5 days per wk for 3 wk (15) | No difference between active and sham CES in depression | 84 |
| McClure et al., 2015 (33) | Sham 9 Active 7 Total 16 | Cortex | 2 mA, 5 Hz, 500 Hz, 15,000 Hz | 20 min/day, 5 days per wk for 2 wk (10) | Active CES reduced depressive symptoms | 67 |
| Trigeminal nerve stimulation (TNS) | ||||||
| Shiozawa et al., 2015 (34) | Sham 20 Active 20 Total 40 | Trigeminal nerve | 120 Hz, 250 μs | 30 min/day for 10 days (10) | Active TNS reduced depressive symptoms | 74 |
Randomized Controlled Trials of tCS for Schizophrenia
| Stimulation Type and Study | N per Group | Anatomical Target(s) | Stimulation Strength | Session Duration and Frequency (Total Sessions) | Main Findingsb | Quality Score (%)c |
|---|---|---|---|---|---|---|
| Transcranial direct current stimulation (tDCS) | ||||||
| Brunelin et al., 2012 (40) | Sham 15 Active 15 Total 30 | L DLPFC, L TPJ | 2 mA | 20 min, twice a day for 5 days (10) | Active tDCS reduced auditory and verbal hallucinations | 63 |
| Fitzgerald et al., 2014d (41) | Sham 12 Active 12 Total 24 | Bilateral (N=11): L+R DLPFC (both anodal), L+R TPJ (both cathodal); unilateral (N=13): L DLPFC, L TPJ | 2 mA | 20 min/day, 5 days/wk for 3 wk (15) | No difference between active and sham tDCS in hallucinations or negative symptoms | 37 |
| Frohlich et al., 2016 (42) | Sham 13 Active 13 Total 26 | L DLPFC, L TPJ | 2 mA | 20 min/day for 5 days (5) | No difference between active and sham tDCS in auditory hallucinations | 74 |
| Mondino et al., 2016e (43) | Sham 12 Active 11 Total 23 | L DLPFC, L TPJ | 2 mA | 20 min, twice a day for 5 days (10) | Active tDCS reduced auditory and verbal hallucinations | 42 |
| Palm et al., 2016 (44) | Sham 10 Active 10 Total 20 | L DLPFC | 2 mA | 10 min/day for 5 days (10) | Active tDCS reduced negative symptoms | 81 |
| Smith et al., 2015 (45) | Sham 16 Active 17 Total 33 | L DLPFC | 2 mA | 20 min/day for 5 days (5) | Active tDCS improved cognition; no effects on psychiatric symptoms or smoking | 84 |
| Transcutaneous vagus nerve stimulation (tVNS) | ||||||
| Hasan et al., 2015 (46) | Sham 10 Active 10 Total 20 | Vagus nerve | 25 Hz, 250 µs pulse width, 0.1–10 mA | Morning to bedtime, daily for 12 weeks (84) | No difference between active and sham tVNS in schizophrenia symptoms | 84 |
Randomized Controlled Trials of tCS for Dementia or Cognitive Deficits
| Study | N per Group | Anatomical Target(s) | Stimulation Strength | Session Duration and Frequency (Total Sessions)) | Dementia Type | Main Findingsb | Quality Score (%)c |
|---|---|---|---|---|---|---|---|
| Boggio et al., 2012 (47) | Total 15d | Temporal cortex | 2 mA | 30 min for 5 days (5) | AD | No difference on most measures; active tDCS improved visual recognition | 52 |
| Manenti et al., 2016 (48) | Sham 10 Active 10 Total 20 | DLPFCe | 2 mA | 25 min/day, 5 days/wk for 2 wk (10) | PD | No difference between active and sham tDCS in motor ability or depressive symptoms | 42 |
| Suemoto et al., 2014 (49) | Sham 20 Active 20 Total 40 | L DLPFC | 2 mA | 20 min/day, 3 days/wk for 2 wk (6) | AD | No difference between active and sham tDCS in apathy | 68 |
Randomized Controlled Trials of tCS for Substance Use Disorders
| Substance and Study | N per Group | Anatomical Target(s) | Stimulation Strength | Session Duration and Frequency (Total Sessions) | Main Findingsb | Quality Score (%)c |
|---|---|---|---|---|---|---|
| Cocaine | ||||||
| Batista et al., 2015 (53) | Sham 19 Active 17 Total 36 | L DLPFC | 2 mA | 20 min/day, every other day for 5 days (5) | Active tDCS reduced craving | 62 |
| Conti et al., 2014 (54) | Sham 6 Active 7 Total 13 | Frontopolar cortex | 2 mA | 20 min/day, every other day (5) | No difference between active and sham tDCS on cocaine use | 58 |
| Smoking | ||||||
| Boggio et al., 2009 (55) | Total 27d | L & R DLPFC | 2 mA | 20 min/day for 5 days (5) | Active tDCS reduced craving | 42 |
| Fecteau et al., 2014 (56) | Total 12d | R DLPFC | 2 mA | 30 min/day for 5 days (5) | Active tDCS reduced number of cigarettes smoked | 58 |
| Alcohol | ||||||
| Da Silva et al., 2013 (57) | Sham 7 Active 6 Total 13 | L DLPFC | 2 mA | 20 min, once a week for 5 wk (5) | Active tDCS reduced depressive symptoms and craving | 58 |
| Klauss et al., 2014 (58) | Sham 17 Active 16 Total 33 | L & R DLPFC | 2 mA | 13 min, twice a day for 5 days (10) | Active tDCS reduced relapse | 68 |
Proof-of-Concept Studies of tCS for Other Neuropsychiatric Disorders
Section 3: Potential Risks Of tCS
Device-Related Risks
Risk of Adverse Cognitive Effects
Risk of Interference With Psychiatric Treatment
Summary: Efficacy and Safety Of tCS In Psychiatric Disorders
Acknowledgments
Footnotes
Supplementary Material
- View/Download
- 467.15 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).