Normal brain maturation, as determined in cross-sectional studies (e.g.,
1–
3) with longitudinal confirmation (e.g.,
4–
10), is characterized as increasing in cortical gray matter volume through the first decade, followed by continuous decline thereafter. Concurrently with the gray matter decline, supratentorial white matter volume continues growing throughout adolescence, with a slowing of the growth trajectory in the third decade (e.g.,
11). Although there are local regional differences in rates of change (
5,
11–
14), these complementary tissue changes define the nature of brain structural maturation. These significant and predictable changes in normal neurodevelopment have led to the speculation that the evolution of the adolescent brain is especially vulnerable to environmental insult. Given that adolescence is also a time of risk-taking and experimentation with “adult behaviors,” such as alcohol drinking, a likely prediction is that excesses of such potentially deleterious agents may result in accelerated gray matter loss, attenuated white matter growth, or both (
15,
16).
Abnormal growth patterns were observed in two recent longitudinal studies of youths who initiated and continued heavy drinking. The first study examined 55 youths, ages 14–19 at baseline, none of whom had ever consumed any alcohol or drugs (
15). At that study’s 2-year follow-up, structural MRI revealed “greater than expected decreased cortical thickness in the right middle frontal gyrus” and “blunted development” in some regional white matter volumes in the 30 youths who initiated “regular” but also “subclinical“ alcohol use (1 to 10 drinks per occasion several times weekly) compared with the 25 youths who remained alcohol and drug free. It is notable, however, that the youths who refrained from drinking showed increasing rather than the typically observed decreasing cortical gray matter thickness, which has implications for interpreting the relative decreasing thickness reported in the drinking group. The second, larger study examined youths over 1- to 8-year intervals and found accelerated gray matter volume reductions in the lateral frontal and temporal cortices and attenuated white matter volume growth of the corpus callosum and pons in 75 heavy drinkers relative to 59 light or nondrinking youths, a pattern common to both sexes (
16). Moderate drinkers were excluded from these reports, however, leaving unaddressed the question of whether highly prevalent, moderate drinking levels (
17) could interfere with normal developmental trajectories.
To address this and related questions, we conducted a longitudinal analysis of structural MRI data collected at baseline (
18) and 1 and 2 years later in 483 youths participating in the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) study (
19). At baseline, all participants met the study entry criteria for no or low drinking and drug use. As anticipated, however, a proportion of these youths (N=127) initiated drinking to levels that exceeded, to varying degrees, the study entry criteria, thereby enabling pursuit of a naturalistic study on the effects of drinking on the adolescent brain. Accordingly, our study had two primary aims: 1) to establish normal growth trajectories, which would be predicted to show declines in regional gray matter volume concurrent with growth of white matter volumes in the youths who continued to meet the no or low age-dependent criteria (“no/low” participants); and 2) to test whether the developmental trajectories of youths who transitioned to exceeding the initial alcohol consumption criteria would conform to patterns identified in previous work in heavy drinking youths showing accelerated gray matter declines with attenuated white matter growth. In light of previous reports, expected group differences would be greatest in frontal and temporal cortices and detectable in white matter volumes (
15,
16). We speculated that the trajectories of moderate drinkers would show accelerated volume loss at a level intermediate between normal decline and accelerated decline of the heavy drinkers. Consideration of these different drinking levels enabled testing for a dose effect based on reported quantities of drinking and seeking correlations between consumption quantities and cortical volume slopes showing group differences by drinking levels. Exploratory analyses examined potential differences related to family history of alcoholism (e.g.,
20,
21) and compounding effects of marijuana and alcohol co-use on brain volume trajectories.
Discussion
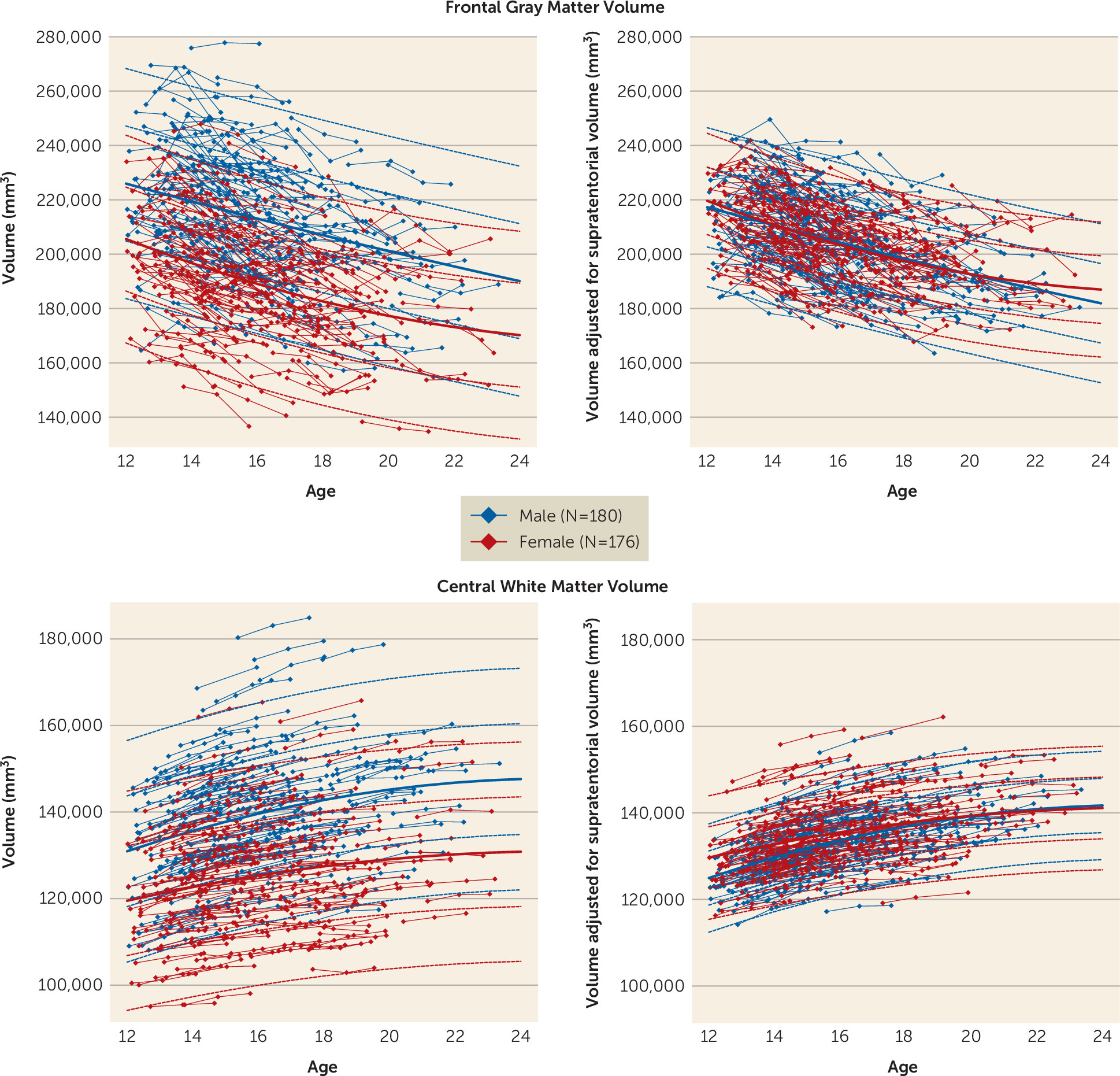
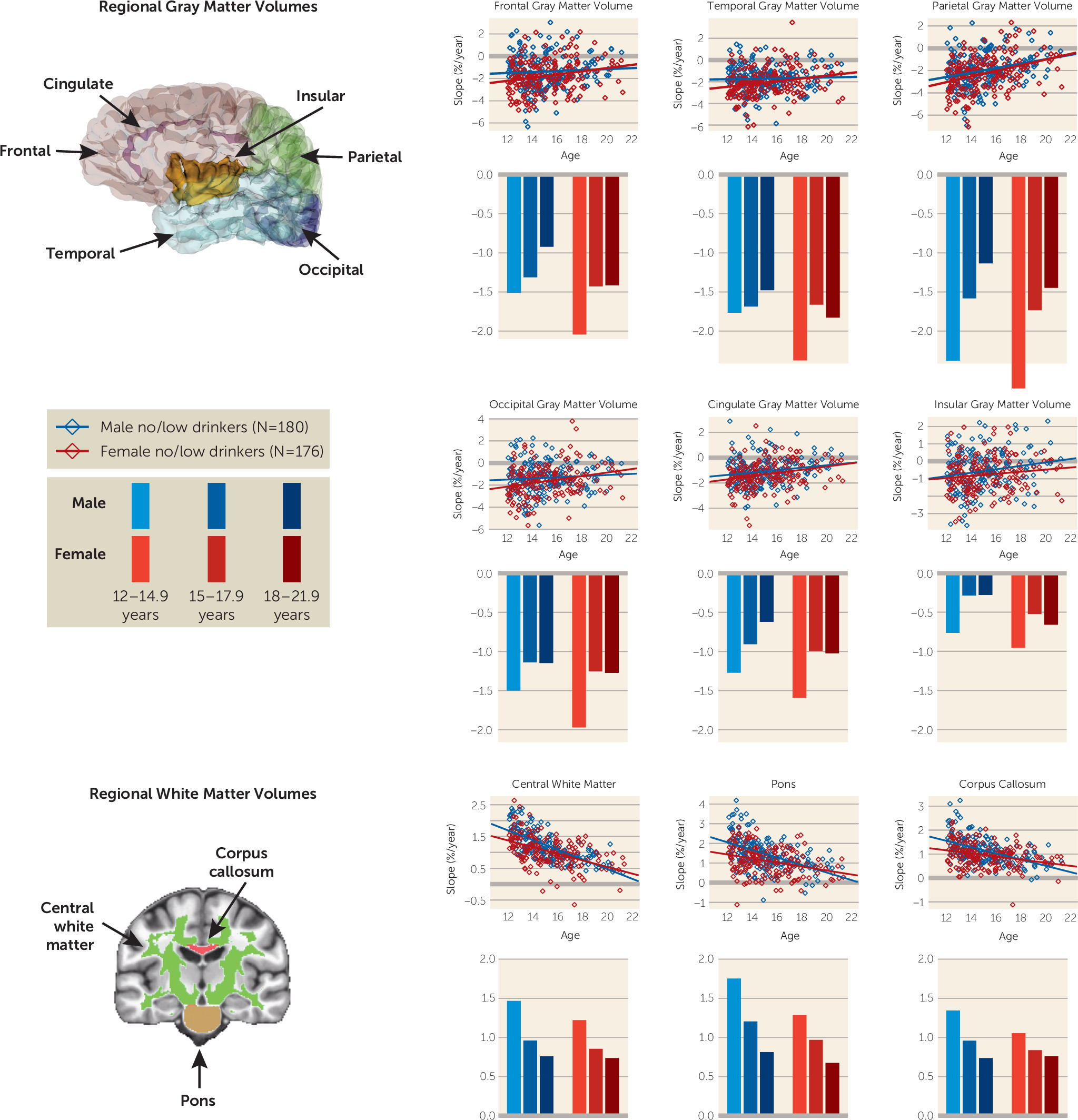
This longitudinal study revealed tissue-specific neuromaturational age-linked rates and patterns of regional volume regression and expansion over 2 years that occur in normally developing adolescents. For cortical gray matter, the general pattern followed a steeper trajectory of volume decline in early adolescence followed by a deceleration in this rate as youths approached young adulthood. Trajectories for both sexes were relatively constant (monotonic), although they were steeper in girls than boys. The parietal cortex exhibited the greatest change per year, with an average decline of about 2.5% per year in the youngest boys and about 3% per year in the youngest girls. Complementing the gray matter volume decline was evidence for growth of white matter volume, which grew at faster rates in the younger ages, especially in boys, and slowed in later adolescence and young adulthood. For example, central white matter volume expanded by about 1.5% annually in the younger adolescents but annual increases fell below 0.75% in the older adolescents. This dynamic growth pattern formed the context for addressing whether and how initiation of moderate or heavy drinking altered components of these developmental trajectories.
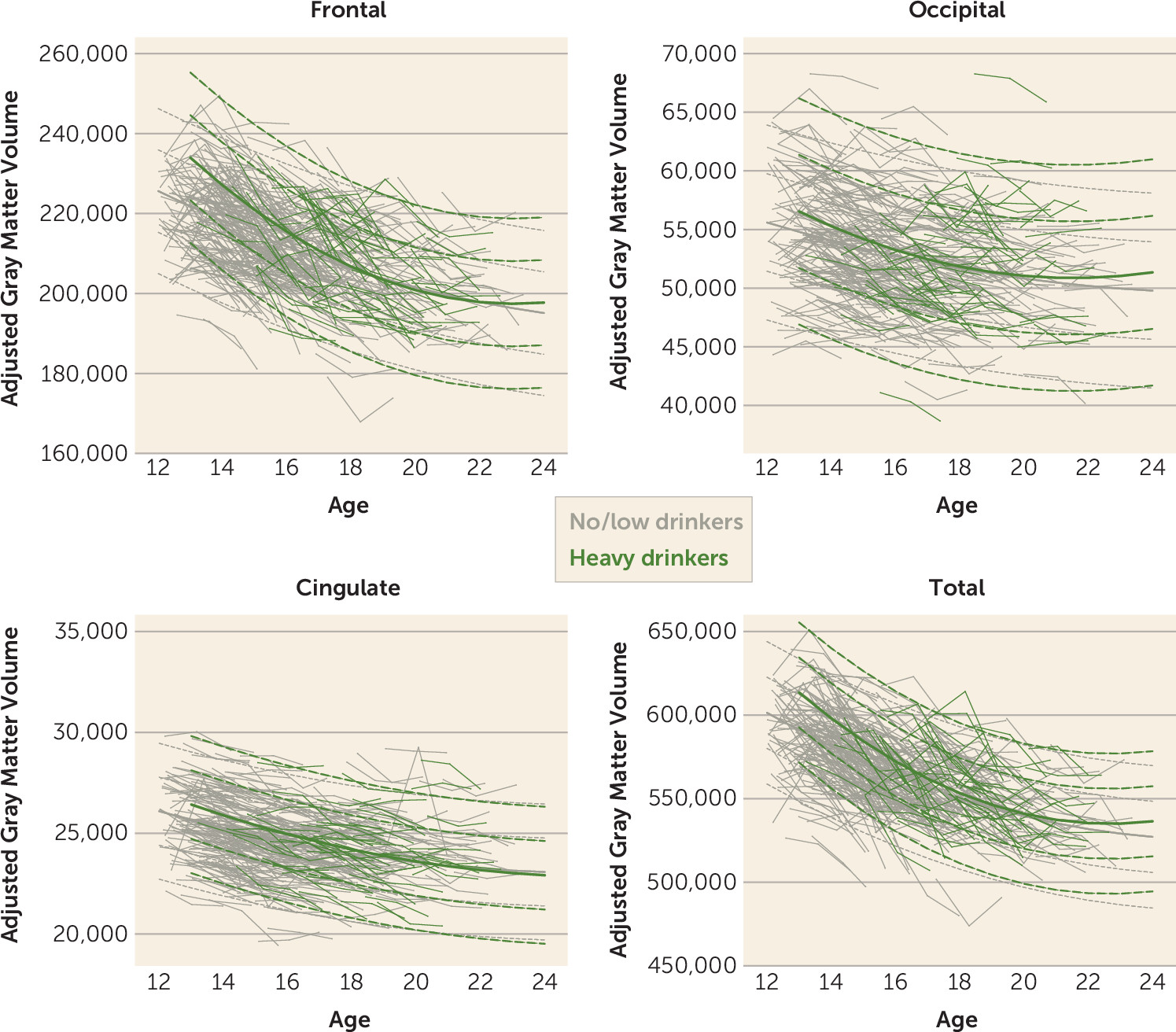
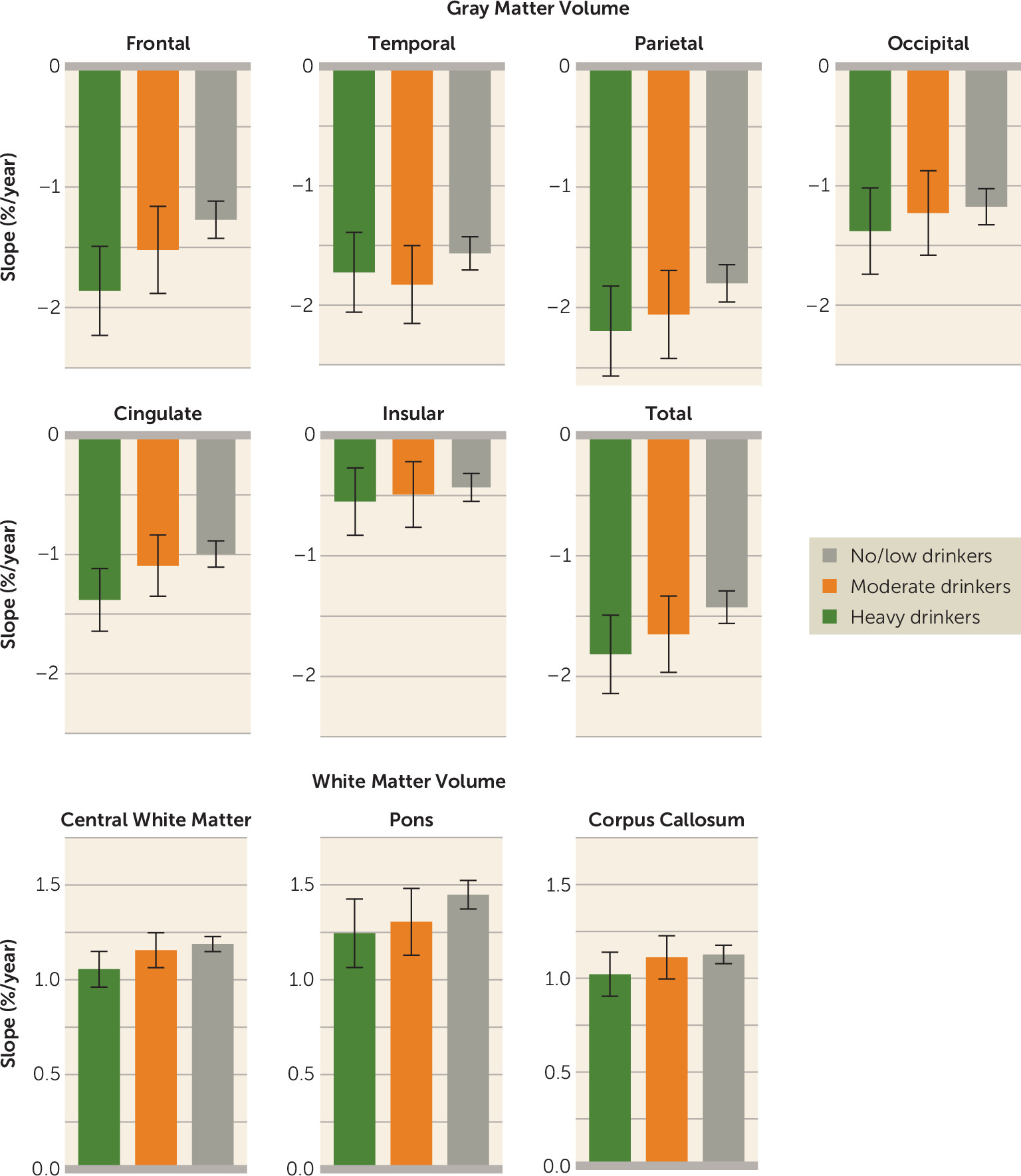
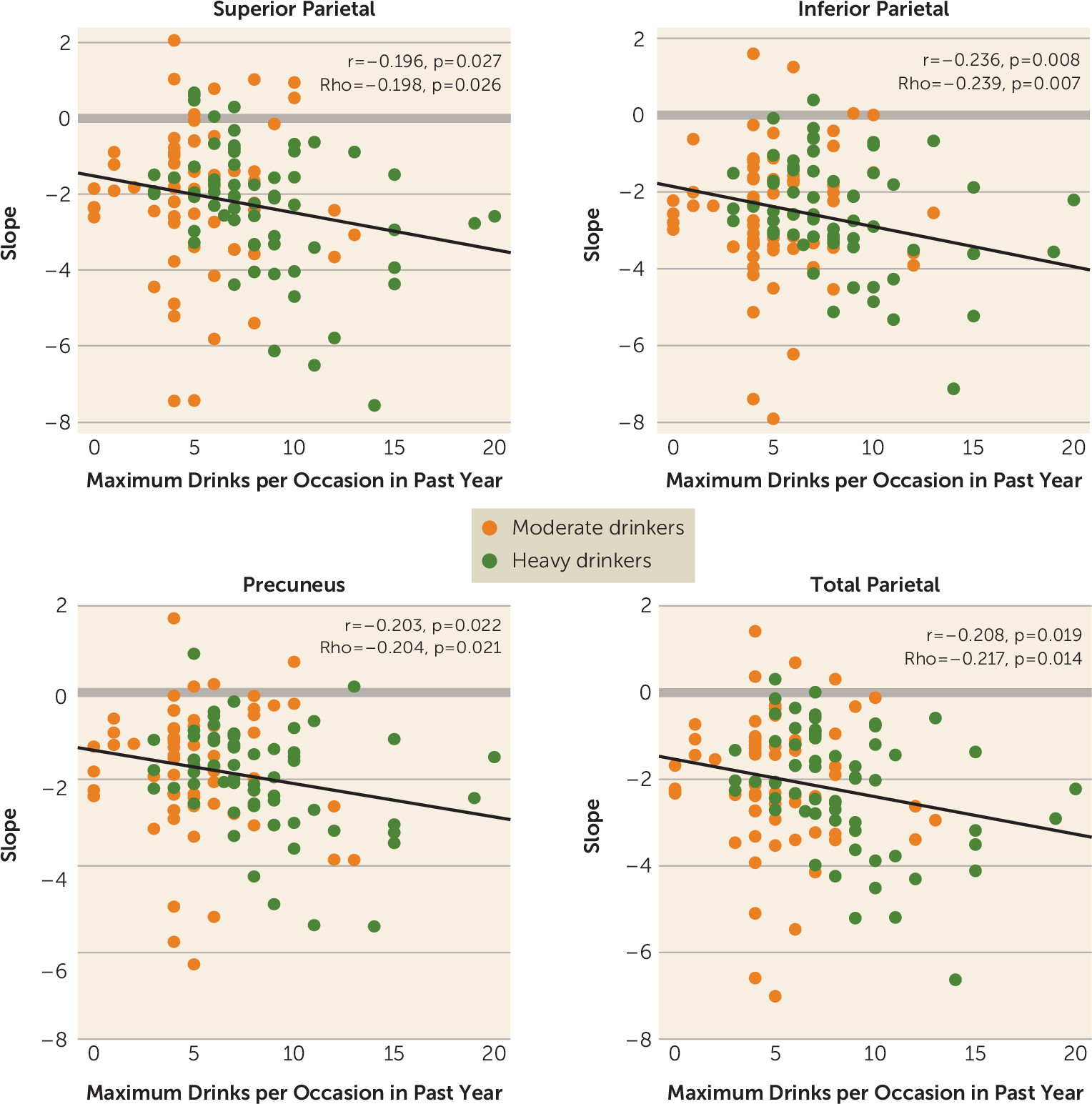
In search of evidence for a dose effect of alcohol consumed on volume trajectories, we combined two sets of quantitative criteria based on drinking patterns over the past year to distinguish moderate from heavy drinkers. The heavy drinking initiators showed significantly steeper slopes than the no/low drinkers. In no case did the volume trajectories of the moderate drinkers differ statistically from the no/low drinkers, even though their arithmetic means were intermediate between the no/low and heavy drinking groups for frontal cortical slopes. Modest support for a dose effect derives from correlations between steeper regional parietal slopes, indicative of faster volume loss, and the maximum number of drinks consumed per occasion in the past year. One speculative interpretation of this apparent acceleration of the pruning trend notable in young adolescent drinkers is an overexuberance of the typical synaptic refinements, suggesting an alteration of progression into the later stages of neurodevelopment.
Although the heavy drinking youths met strict drinking criteria that significantly exceeded drinking reported in the no/low drinkers, we determined from published data that, on average, our heavy drinkers consumed alcohol at lower levels and less frequently than youths in two other longitudinal MRI studies of heavy drinking initiation. We estimated that the number of days drinking per year was 47 in the Luciana et al. study (
15), 115 in the Squeglia et al. study (
16), and 43 for the heavy drinkers but only 15 for the moderate drinkers in the present study. Also estimated were the number of drinks consumed per year: 268 in the Luciana et al. study and 157 for the heavy drinkers and 36 for the moderate drinkers in the present study. Taken together, this study and the two earlier longitudinal studies of more heavily drinking youths reported greater than normal age-related cortical thinning or volume reduction in the frontal and cingulate cortices in two studies (the Luciana et al. study and the present study) and in the frontal cortex in all three studies. Developmentally, the frontal cortex is the last region to mature, and it may retain the plasticity for modification from environmental factors throughout late adolescence and into early adulthood.
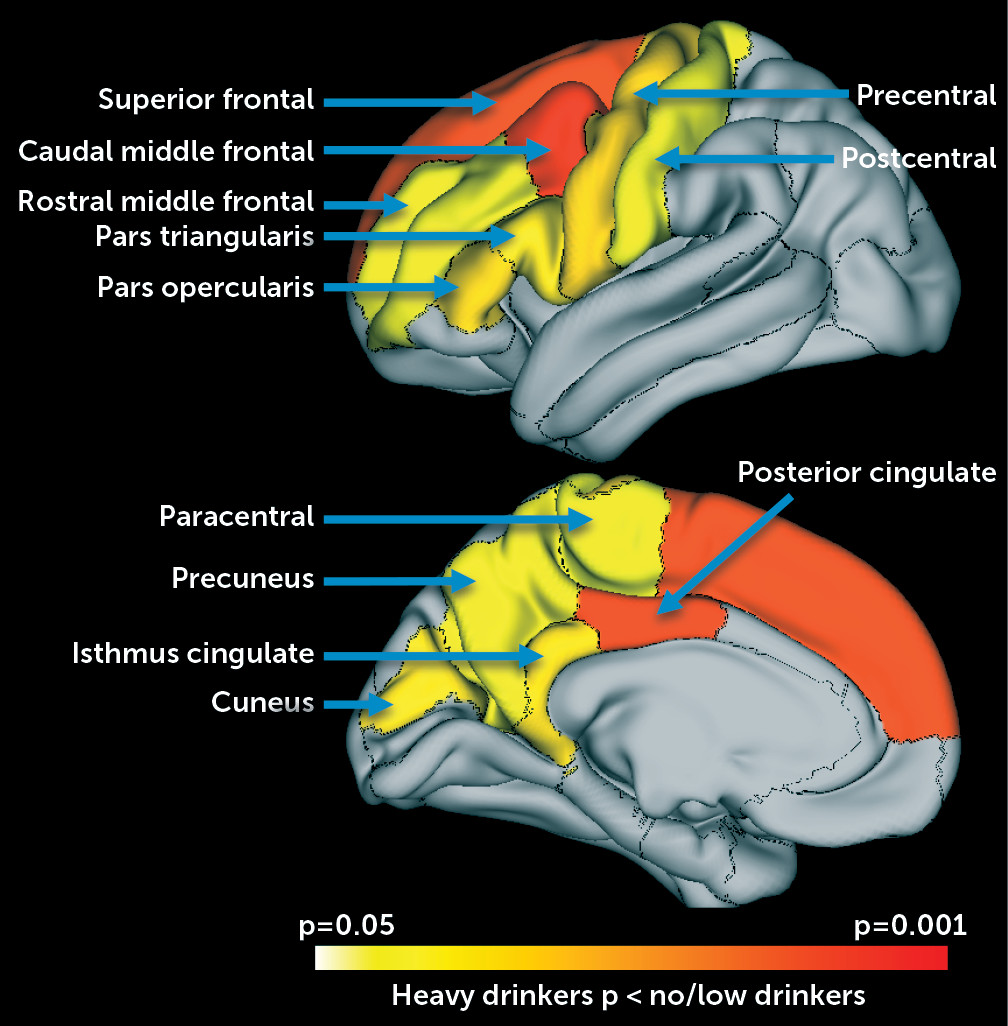
The more finely grained parcellation analysis of cortex revealed substantially faster declines in the heavy drinkers than in the no/low drinkers in a constellation of superior and caudal middle frontal and posterior cingulate cortical volumes. The posterior cingulate cortex has been found to have the highest cerebral blood perfusion to acute alcohol infusion, as measured with arterial spin labeling MRI (
31). Given that this region has been observed as affected in heavy drinking youths (
15,
16), it is tempting to speculate that there is a relationship between repeated acute regional perfusion experiences with high doses of alcohol and ultimate effects on local tissue volumes.
To the extent that alcohol history documented retrospectively in interviews reflects accurate assessment of consumption, quantity and frequency metrics of alcohol consumption provide estimates of amount consumed. Exploration of available drinking variables (lifetime drinking days, lifetime drinks, lifetime binges, and maximum drinks per occasion in the past year) identified greater maximum drinks as a correlate of accelerating brain structural change slopes, but only in the total and regional parietal volumes. These relationships present novel support for an alcohol dose effect on volume declines in recently initiated adolescent drinkers. The stepwise steeper slopes in no/low to moderate to heavy drinking youths indicating volume declines also suggest a dose-response effect, with the moderate drinkers falling (statistically nonsignificantly) between the other drinking groups, a pattern most apparent for frontal and total gray matter volumes (see
Figure 4). Other studies, too, have found maximum drinks per occasion to be useful in understanding drinking patterns and their consequences. For example, a trajectory analysis of young adults’ alcohol consumption in the Collaborative Study on the Genetics of Alcoholism revealed the utility of maximum drinks per occasion in predicting drinking patterns (
32). An escalation of maximum drinks has been found to be predictive of greater impulsivity/compulsivity scores and disturbance of fronto-parietal control mechanisms (
33).
The developmental trajectories of the no/low drinking participants are consistent with the general literature. The accelerated longitudinal study design and geographically widespread multisite recruitment provided some assurance of broad age sampling over just a few years and a measure of generalizability. Nonetheless, even this controlled, longitudinal study design has limitations. The results remain limited in age sampling, demographic representation (especially with respect to family history of alcoholism), and finely grained quantification of alcohol consumption. Despite the prospective nature of the study, factors unmeasured at baseline could present pre-existing conditions underlying the ostensibly alcohol-related effects on brain structure. Indeed, having a positive family history of alcoholism may have compounded the abnormal slope accelerations observed in the youths who transitioned into heavy drinking.
An earlier study reported smaller brain volumes at baseline in youths who initiated drinking at hazardous levels compared with low drinking control subjects (
29), whereas we found no volume difference at baseline between our no/low and heavy drinkers. The former study had smaller samples, recruited participants at high risk for substance use disorders, had an underrepresentation of female participants, and had a higher proportion of drinkers with a positive family history than our NCANDA sample. Recognizing these sampling differences, we believe that the lack of regional differences at baseline in the NCANDA sample is a strength, supporting the possibility that the greater decline in volumes across age in the drinkers was attributable to drinking rather than to pre-existing conditions.
In conclusion, these results provide evidence that initiation of heavy alcohol drinking during adolescence can disrupt normal, differential growth trajectories of specific cortical gray matter regions. Although significant effects on brain volumetric trajectories were not observed in moderate drinkers, this group’s intermediate position between no/low and heavy drinkers on many measures suggests a dose or threshold effect. A factor potentially contributing to the abnormally smaller cortical volumes, notably in frontal regions, may be alcohol-related acceleration of normal pruning mechanisms (
34) in regions with high cerebral blood perfusion during acute alcohol use (
31,
35). The question of whether reduction in drinking restores the normal trajectories or acceleration in alcohol consumption to dependence levels results in further acceleration of gray matter volume declines and attenuation of white matter growth awaits continued longitudinal study of these NCANDA participants.