T
o the E
ditor: Over the last decade, the detection of autoantibodies against neurotransmitter receptors in patients with neuropsychiatric disorders has raised hopes for a better understanding of the molecular cascades underlying these pathologies and for providing appropriate therapy (
1). The link between psychotic disorders and autoimmunity has regained strong support following the discovery of anti–
N-methyl-
d-aspartate receptor (NMDAR) autoantibody encephalitis, which is associated with psychotic symptoms (
2). However, the biological significance of circulating NMDAR autoantibodies from psychotic patients remains poorly understood (
3). Indeed, most studies have focused on autoantibody detection assays and prevalence (
3) but have hardly addressed whether NMDAR autoantibodies have the potency to alter the localization and, thus, the function of NMDAR, as predicted by the well-established model of NMDAR hypofunction in psychosis (
4). Here, we directly addressed this important question by employing the innovative and sensitive single nanoparticle imaging method to examine the functional effect of NMDAR autoantibodies from patients with first-episode psychosis.
Schematically, NMDAR autoantibody seropositive patients with first-episode psychosis (4.7%), having minimal or no exposure to antipsychotics, were identified from the OPTIMIZE project (
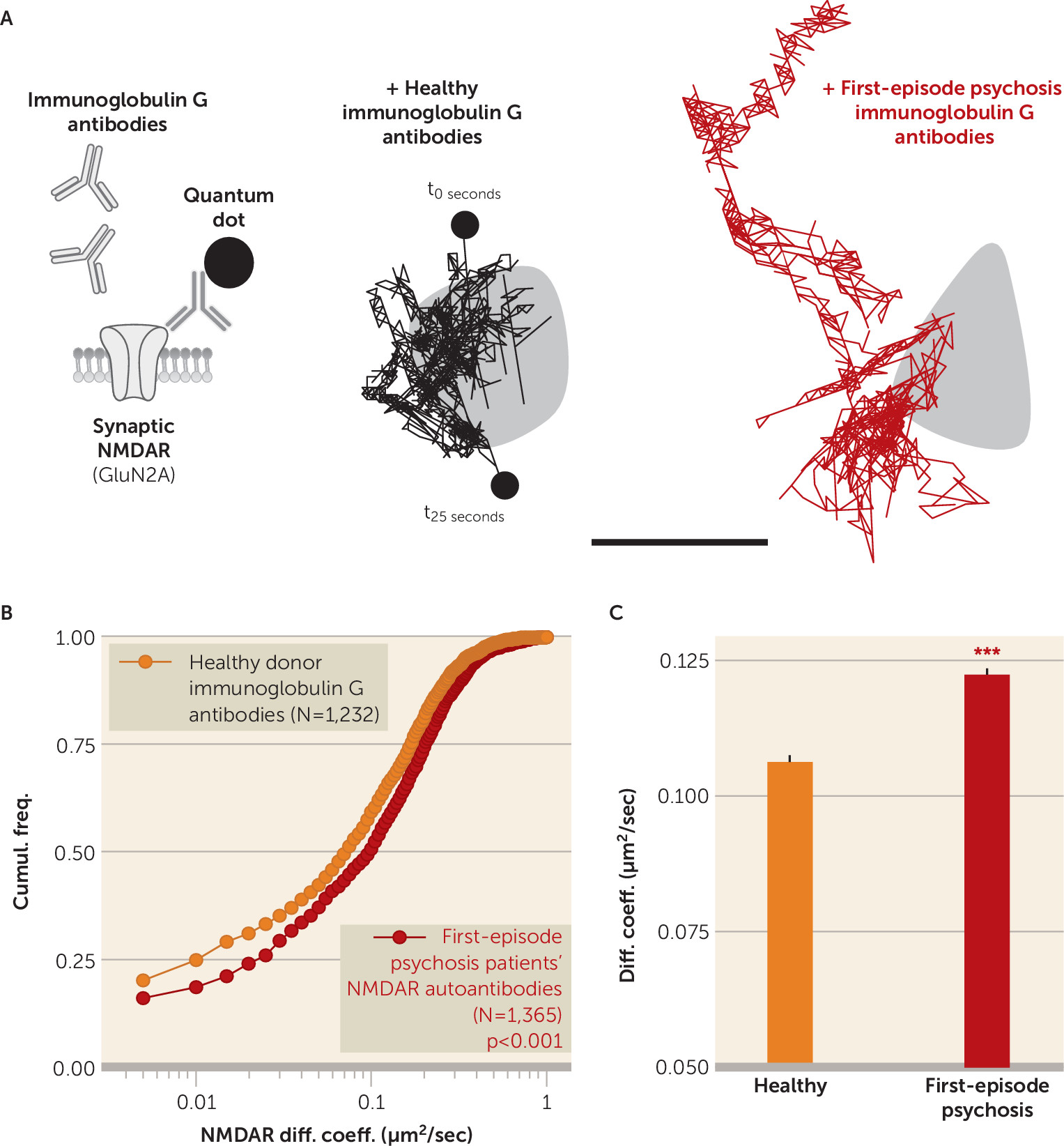
5). To determine whether these patients’ immunoglobulin G antibodies alter the synaptic function of NMDAR in live hippocampal neurons, we used single molecule imaging to localize and track membrane synaptic NMDAR exposed to NMDAR autoantibodies. Indeed, contrary to bulk imaging approaches, the development of single molecule imaging has provided unprecedented information about the dynamic organization of single NMDARs and their pathophysiological regulation.
As previously demonstrated (
6), membrane NMDARs explore the dendritic and synaptic area, in which they specifically stabilize and contribute to the NMDAR-mediated transmission. When hippocampal neurons were acutely exposed to psychotic patients’ NMDAR autoantibodies, the synaptic NMDARs were clearly destabilized with increased dynamics that contrast with the behavior of receptors exposed to purified immunoglobulin G antibodies from healthy seronegative donors (
Figure 1). It is noteworthy that the synaptic disorganization observed with NMDAR autoantibodies in patients with first-episode psychosis resembles the one previously described with NMDAR autoantibodies from anti-NMDA encephalitis patients (
7). Thus, because of single molecule imaging, we could determine that NMDAR autoantibodies from patients with first-episode psychosis displaced synaptic NMDAR, leading to an NMDAR hypofunction that constitutes the core hypothesis of psychosis (
4). The molecular pathogenicity of NMDAR autoantibodies in patients with first-episode psychosis, which would be relevant in vivo
, should prompt clinicians to screen for these autoantibodies because it may open the possibility to use immunotherapy to treat patients with first-episode psychosis who are antibody-positive.