The Burden of Bereavement: Early-Onset Depression and Impairment in Youths Bereaved by Sudden Parental Death in a 7-Year Prospective Study
Abstract
Objective:
Methods:
Results:
Conclusions:
Methods
Participant Recruitment
Assessments
Data Analyses
Results
Sample Description
| Characteristic | Total | Nonbereaved | Bereaved | Test | df | p | |||
|---|---|---|---|---|---|---|---|---|---|
| Offspring | |||||||||
| N | 388 | 172 | 216 | ||||||
| Mean | SD | Mean | SD | Mean | SD | ||||
| Age (years)a | 12.0 | 3.0 | 12.0 | 2.8 | 12.0 | 3.1 | t=–0.05 | 386 | 0.96 |
| N | % | N | % | N | % | ||||
| Female | 188 | 48.5 | 84 | 48.8 | 104 | 48.1 | χ2=0.02 | 1 | 0.89 |
| White | 311 | 80.2 | 144 | 83.7 | 167 | 77.3 | χ2=2.47 | 1 | 0.12 |
| History of psychiatric disordersb | |||||||||
| Depression diagnosis | 42 | 10.9 | 14 | 8.2 | 28 | 13.0 | χ2=2.30 | 1 | 0.13 |
| Bipolar disorder diagnosis | 3 | 0.8 | 0 | 0.0 | 3 | 1.4 | Fisher’s | — | 0.26 |
| Anxiety diagnosis | 33 | 8.5 | 12 | 7.0 | 21 | 9.7 | χ2=0.90 | 1 | 0.34 |
| Posttraumatic stress disorder diagnosis | 4 | 1.0 | 1 | 0.6 | 3 | 1.4 | Fisher’s | — | 0.63 |
| Attention deficit hyperactivity disorder diagnosis | 56 | 14.6 | 19 | 11.2 | 37 | 17.2 | χ2=2.78 | 1 | 0.10 |
| Behavioral disorder diagnosis | 21 | 5.5 | 6 | 3.5 | 15 | 7.0 | χ2=2.19 | 1 | 0.14 |
| Alcohol or substance abuse diagnosis | 4 | 1.0 | 2 | 1.2 | 2 | 0.9 | Fisher’s | — | >0.99 |
| Any psychiatric history | 111 | 28.8 | 39 | 22.9 | 72 | 33.5 | χ2=5.15 | 1 | 0.02 |
| Physical or sexual abuse | 21 | 5.4 | 3 | 1.7 | 18 | 8.3 | χ2=8.12 | 1 | 0.004 |
| Psychiatric disorders at baseline | |||||||||
| Depression diagnosis | 45 | 11.6 | 7 | 4.1 | 38 | 17.6 | χ2=17.08 | 1 | <0.001 |
| Bipolar disorder diagnosis | 8 | 2.1 | 2 | 1.2 | 6 | 2.8 | Fisher’s | — | 0.31 |
| Anxiety diagnosis | 41 | 10.6 | 14 | 8.1 | 27 | 12.5 | χ2=1.93 | 1 | 0.17 |
| Posttraumatic stress disorder diagnosis | 18 | 4.6 | 0 | 0.0 | 18 | 8.3 | χ2=15.03 | 1 | <0.001 |
| Attention deficit hyperactivity disorder diagnosis | 53 | 13.7 | 19 | 11.1 | 34 | 15.7 | χ2=1.79 | 1 | 0.18 |
| Behavioral disorder diagnosis | 18 | 4.6 | 6 | 3.5 | 12 | 5.6 | χ2=0.92 | 1 | 0.34 |
| Alcohol or substance abuse diagnosis | 2 | 0.5 | 1 | 0.6 | 1 | 0.5 | Fisher’s | — | >0.99 |
| Any psychiatric disorder at baseline | 116 | 29.9 | 33 | 19.2 | 83 | 38.4 | χ2=16.91 | 1 | <0.001 |
| Mean | SD | Mean | SD | Mean | SD | ||||
| Functioningc | 78.6 | 11.8 | 82.2 | 10.1 | 75.7 | 12.2 | t=5.72 | 384.6 | <0.001 |
| Self-reported clinical measures | |||||||||
| Depression z score | 0.23 | 1.09 | –0.04 | 0.94 | 0.48 | 1.16 | t=–4.64 | 349.5 | <0.001 |
| Anxiety z score | 0.25 | 1.05 | 0.13 | 0.98 | 0.36 | 1.10 | t=–2.09 | 355.8 | 0.04 |
| Suicidal ideation | 21.5 | 11.4 | 19.7 | 9.9 | 23.0 | 12.41 | t=–2.75 | 345.5 | 0.01 |
| Impulsive aggression | 69.6 | 22.4 | 66.6 | 20.4 | 72.2 | 23.9 | t=–2.38 | 354 | 0.02 |
| Posttraumatic stress disorder | 2.98 | 5.86 | 0.47 | 2.22 | 5.72 | 7.23 | z=–11.46 | — | <0.001 |
| Negative coping strategies z score | 0.16 | 1.00 | 0.16 | 0.98 | 0.15 | 1.02 | t=0.12 | 336 | 0.91 |
| Family climate | 52.7 | 8.9 | 53.8 | 8.3 | 51.7 | 9.3 | t=2.22 | 343 | 0.03 |
| Intercurrent life events z score | 0.82 | 1.15 | 0.55 | 1.00 | 1.03 | 1.21 | t=–4.29 | 383.5 | <0.001 |
| Social support z score | –0.05 | 1.02 | 0.11 | 1.00 | –0.18 | 1.02 | t=2.70 | 353 | 0.01 |
| Surviving caretaking adult | |||||||||
| N | 240 | 99 | 141 | ||||||
| Mean | SD | Mean | SD | Mean | SD | ||||
| Age (years) | 43.3 | 7.7 | 42.4 | 6.3 | 43.8 | 8.4 | t=–1.37 | 226 | 0.17 |
| Hollingshead scale score | 43.5 | 12.4 | 45.8 | 10.7 | 42.1 | 13.2 | t=1.81 | 154 | 0.07 |
| N | % | N | % | N | % | ||||
| Female | 195 | 81.3 | 75 | 75.8 | 120 | 85.1 | χ2=3.34 | 1 | 0.07 |
| White | 203 | 84.6 | 86 | 86.9 | 117 | 83.0 | χ2=0.67 | 1 | 0.41 |
| Spouse or significant other of the deceased | 173 | 75.9 | 80 | 92.0 | 93 | 66.0 | χ2=19.87 | 1 | <0.001 |
| History of psychiatric disordersb | |||||||||
| Depression diagnosis | 99 | 41.4 | 31 | 31.6 | 68 | 48.2 | χ2=6.56 | 1 | 0.01 |
| Bipolar disorder diagnosis | 7 | 2.9 | 1 | 1.0 | 6 | 4.3 | Fisher’s | 1 | 0.25 |
| Psychosis diagnosis | 1 | 0.4 | 1 | 1.0 | 0 | 0.0 | Fisher’s | — | 0.41 |
| Anxiety diagnosis | 61 | 25.4 | 15 | 15.2 | 46 | 32.6 | χ2=9.37 | 1 | 0.002 |
| Posttraumatic stress disorder diagnosis | 25 | 10.4 | 9 | 9.1 | 16 | 11.3 | χ2=0.32 | 1 | 0.57 |
| Alcohol or substance abuse diagnosis | 66 | 27.8 | 28 | 28.3 | 38 | 27.5 | χ2=0.02 | 1 | 0.90 |
| Personality disorder diagnosis | 8 | 3.3 | 2 | 2.0 | 6 | 4.3 | Fisher’s | — | 0.48 |
| Any psychiatric history | 150 | 63.0 | 51 | 52.0 | 99 | 70.7 | χ2=8.63 | 1 | 0.003 |
| Mean | SD | Mean | SD | Mean | SD | ||||
| Functioningc | 76.8 | 12.2 | 82.0 | 9.2 | 73.6 | 12.7 | t=5.78 | 219.2 | <0.001 |
| Deceased parent | |||||||||
| N | 241 | 98 | 143 | ||||||
| Mean | SD | Mean | SD | Mean | SD | ||||
| Age (years) | 43.9 | 7.7 | 43.4 | 7.0 | 44.3 | 8.2 | t=–0.86 | 239 | 0.39 |
| Hollingshead scale score | 43.4 | 13.4 | 46.6 | 11.4 | 41.0 | 14.3 | t=2.67 | 150.02 | 0.01 |
| N | % | N | % | N | % | ||||
| Male | 186 | 77.5 | 74 | 76.3 | 112 | 78.3 | χ2=0.14 | 1 | 0.71 |
| White | 199 | 82.9 | 84 | 86.6 | 115 | 80.4 | χ2=1.56 | 1 | 0.21 |
| History of psychiatric disordersb | |||||||||
| Depression diagnosis | 93 | 39.1 | 31 | 32.3 | 62 | 43.7 | χ2=3.11 | 1 | 0.08 |
| Bipolar disorder diagnosis | 18 | 7.5 | 2 | 2.0 | 16 | 11.2 | χ2=7.04 | 1 | 0.01 |
| Psychosis diagnosis | 3 | 1.3 | 0 | 0.0 | 3 | 2.1 | Fisher’s | — | 0.28 |
| Anxiety diagnosis | 56 | 23.6 | 25 | 26.0 | 31 | 22.0 | χ2=0.52 | 1 | 0.47 |
| Posttraumatic stress disorder diagnosis | 23 | 9.6 | 13 | 13.4 | 10 | 7.0 | χ2=2.74 | 1 | 0.10 |
| Alcohol or substance abuse diagnosis | 131 | 54.4 | 43 | 43.9 | 88 | 61.5 | χ2=7.31 | 1 | 0.01 |
| Personality disorder diagnosis | 39 | 16.2 | 4 | 4.1 | 35 | 24.5 | χ2=17.83 | 1 | <0.001 |
| Any psychiatric history | 177 | 73.8 | 66 | 68.0 | 111 | 77.6 | χ2=2.74 | 1 | 0.10 |
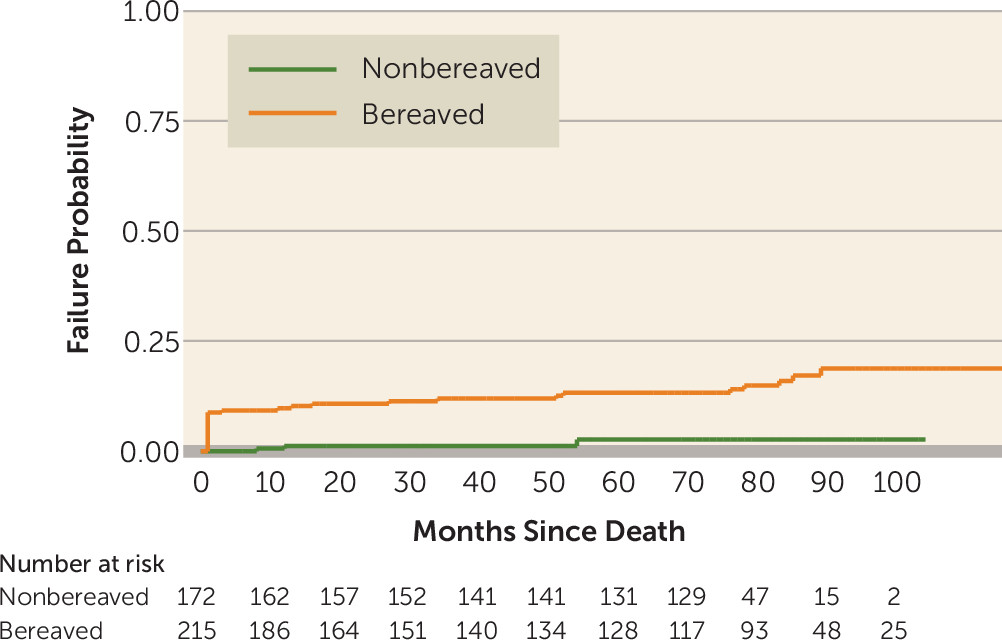
Incidence


Prevalence

Incidence and Course of Impairment
| Variable | Hazard Ratio | 95% CI | t | p |
|---|---|---|---|---|
| Bereavement | 2.07 | 1.43, 2.99 | 3.89 | <0.001 |
| Age at parent’s death | 0.95 | 0.90, 0.99 | –2.19 | 0.03 |
| Female | 1.34 | 0.98, 1.82 | 1.85 | 0.06 |
| White | 0.59 | 0.40, 0.88 | –2.57 | 0.01 |
| Socioeconomic status | 0.99 | 0.98, 1.01 | –0.94 | 0.35 |
| History of psychiatric disorder (offspring) | 4.02 | 2.86, 5.66 | 7.97 | <0.001 |
| History of psychiatric disorder (parent) | 1.17 | 0.71, 1.94 | 0.62 | 0.54 |
| Physical or sexual abuse | 1.48 | 0.93, 2.36 | 1.64 | 0.10 |
Pathways for the Relationship Between Bereavement and Impairment

Discussion
Acknowledgments
Footnote
Supplementary Material
- View/Download
- 557.26 KB
- View/Download
- 857.02 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).