Family psychiatric history is a strong and consistent risk factor for psychiatric disorders outside the perinatal period (
9,
10). Perinatal mood disorders may be more heritable than other mood disorders; the heritability for perinatal depression is estimated to be 44% (
11), compared with 37% for major depressive disorder (
12,
13). Heritability of other types of perinatal psychiatric disorders is unknown. A family history of a postpartum mood disorder in a mother or sister doubles or triples the risk of experiencing a postpartum mood disorder (
14–
16), and postpartum psychosis in a mother or sister increases the risk of postpartum psychosis fivefold (
14). A family history of nonpostpartum mood disorders is also associated with postpartum mood disorders, especially for bipolar disorder and the most severe postpartum episodes, such as postpartum psychosis (
14,
16–
19). Studies of postpartum psychosis, however, have been conducted primarily in high-risk populations of women and their families with previously diagnosed psychiatric disorders. Much less is known about how familiality of psychiatric disorders outside the perinatal period influences postpartum psychiatric disorders for the broader spectrum of psychiatric disorders, particularly in women without a personal psychiatric history. The few existing population-based studies examining the association between family history of nonpostpartum mood disorders and postpartum mood disorders have not investigated specific types of psychiatric disorders among different degrees of familial relationships (
3,
20).
Previous work has not explored whether the familial associations of postpartum psychiatric disorders are related to a specific female vulnerability (e.g., mother to daughter). Because previous studies of familiality of postpartum psychiatric disorders have primarily evaluated the relationship between postpartum mood disorders in proband mothers and postpartum mood disorders in first-degree relatives, most have exclusively evaluated pairs of female relatives (e.g., mother–daughter or sister–sister pairs) (
11,
14–
16,
21,
22). Among studies that included both male and female relatives with psychiatric disorders outside the perinatal period, none have evaluated the difference in recurrence risk among female relatives compared with male relatives (
11,
17). Understanding the degree to which familial history of psychiatric disorders predicts risk for postpartum psychiatric disorders would substantially aid our ability to identify women at greatest risk for postpartum psychiatric disorders and intervene early.
We aimed to address this gap in the literature by evaluating how family history of psychiatric disorders influences risk for postpartum psychiatric episodes. We wanted to evaluate whether familial risk of postpartum psychiatric disorders differs by degree of relationship and sex of the family members in women both with and without a prior personal psychiatric history. To address these aims, we conducted a population-based study of recurrence risk (the likelihood that a trait in one family member will occur in another family member) (
23–
25), a study design frequently applied in psychiatric genetics (
10,
14,
16,
25,
26). Recurrence risk studies typically evaluate the same disorder in family members (e.g., postpartum depression in both a proband mother and her sister). In our study, we sought to determine the unique familial contributions of psychiatric disorders outside the perinatal period to psychiatric events within the postpartum period; thus, we considered the recurrent event (a psychiatric diagnosis within the postpartum period) to be different from the familial event (a psychiatric diagnosis at any time point). We refer here to this specific type of recurrence risk as “familial risk.”
Method
Study Population
We conducted a population-based cohort study within the Danish Civil Registration System (
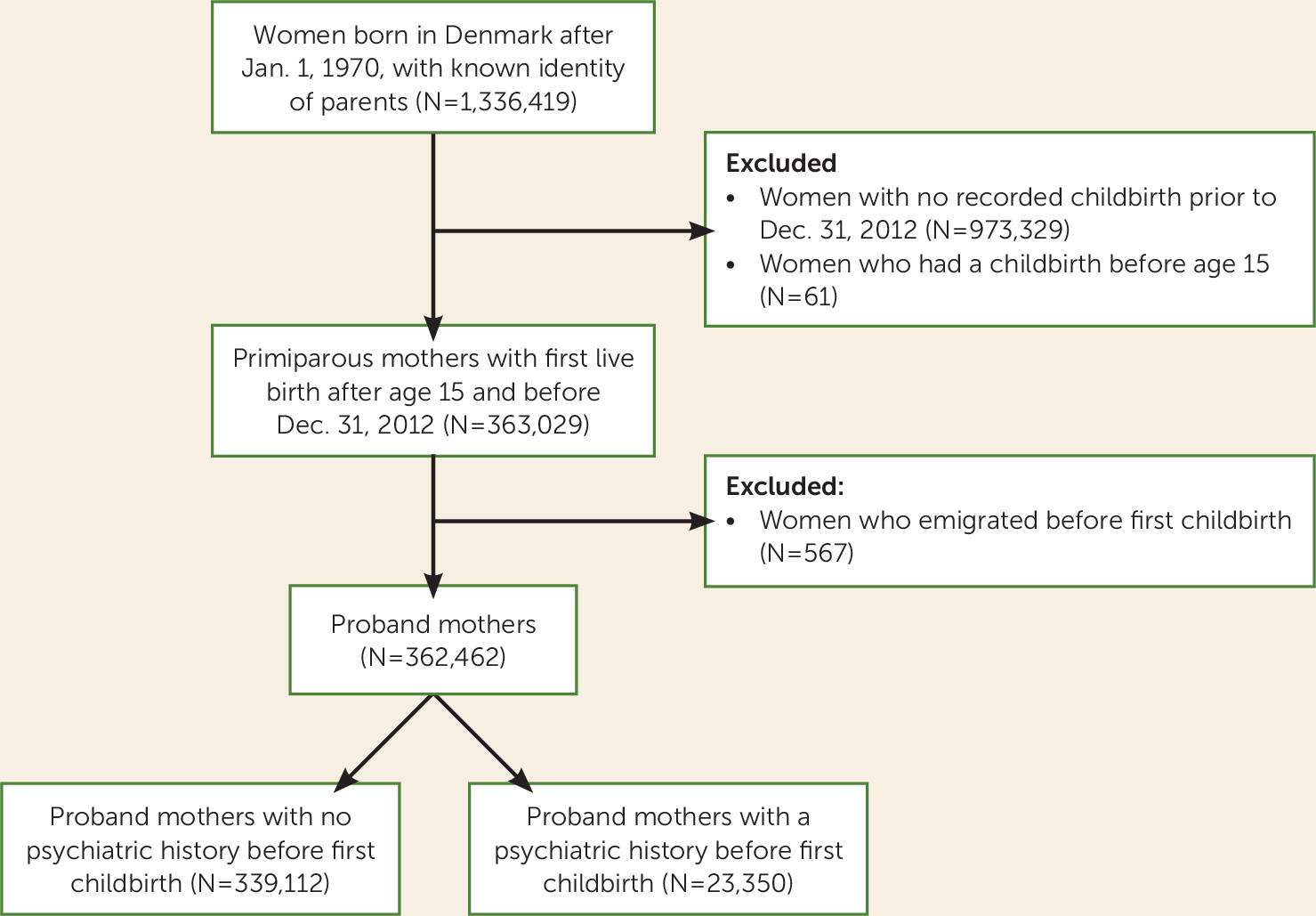
27). A unique personal identifier for every person living in Denmark allows comprehensive linkages with multiple health-related national registers as well as linkages to family members. Proband mothers were selected from among all women born in Denmark from 1970 onward with nonmissing links to both parents (N=1,336,419). Proband mothers were all first-time mothers who gave live birth when at least 15 years of age and before the end of follow-up on Dec. 31, 2012. A total of 362,462 proband mothers were included in our study (
Figure 1).
Identification of Postpartum Psychiatric Episodes
Our outcome of interest was a psychiatric episode diagnosis during the postpartum period in proband mothers. Information on psychiatric episodes was obtained from the Psychiatric Central Register (
28), which contains information on inpatient treatment since 1969 and outpatient treatment since 1995. Outpatient diagnoses come from specialty psychiatric clinics and do not include diagnoses from primary care settings. Diagnoses are recorded using ICD codes (ICD-8 before 1994 and ICD-10 1994 and later). We defined a postpartum psychiatric disorder as a treated psychiatric episode (ICD-8 codes 290–315; ICD-10 codes F00–F99), excluding organic mental disorders (ICD-8 codes 290.09, 290.10, 290.11, 290.18, 290.19, 292.x9, 293.x9, 294.x9, and 309.x9; ICD-10 codes F00–F09), substance abuse (ICD-8 codes 291.x9, 294.39, 303.x9, 303.20, 303.28, 303.90, and 304.x9; ICD-10 codes F10–F19), and mental retardation (ICD-8 codes 310–315; ICD-10 codes F70–F79), which have been well validated in these registries (
28,
29). For our primary analysis, we considered the postpartum period to be 0 to 6 months after childbirth. Previous work in our data has indicated increasing vulnerability for depressive episodes up to 6 months after childbirth (
2), and we wanted to ensure that we accounted for a potential delay between symptom onset and recorded diagnosis. In sensitivity analyses, we also examined two other periods separately: 0 to 3 months postpartum, a more narrowly defined and possibly more etiologically similar phenotype (
30–
32); and 0 to 12 months postpartum, an increasingly applied clinical definition for the postpartum period (
30,
33,
34).
Identification of Relatives of Proband Mothers and Family History of Psychiatric Episodes
To identify relatives, proband mothers were linked to their parents by unique identifier, and subsequent family relationships were identified through these linkages. The degree of relationship of family members was defined as follows: first-degree relatives included mother, father, and full sibling; second-degree relatives included grandparents, half siblings, uncles, and aunts; third-degree relatives included cousins. Because the Danish Civil Registration System (
27) was established in 1968, we were unable to identify all people born before that time; thus, second- and third-degree relationships are less complete.
Among the proband mothers included in our study population, we considered the association between a postpartum psychiatric disorder and any psychiatric disorder in our categorized relatives. Furthermore, we investigated specifically five hierarchical diagnostic groups of psychiatric disorders in the relatives: 1) schizophrenia and related disorders (highest in hierarchy; ICD-10 codes F20–F29); 2) bipolar disorder (ICD-10 codes F30–F31); 3) unipolar disorder (ICD-10 codes F32–F33); 4) other mood disorders, excluding bipolar and unipolar disorders (ICD-10 codes F34–F39); and 5) other psychiatric disorders (lowest in hierarchy; ICD-10 codes F40–F69 and F80–F99). This hierarchical system is built into the ICD diagnostic system and accounts for individuals with more than one recorded diagnosis.
Statistical Analysis
We started follow-up at the date of childbirth for each proband mother and followed her until a postpartum psychiatric episode, 6 months postpartum (3 or 12 months in sensitivity analyses), death, emigration, or Dec. 31, 2012, whichever came first. We restricted proband mothers to first-time mothers for several reasons: history of postpartum depression increases risk in subsequent pregnancies; previous birth outcome may influence later reproductive behavior; and environmental factors during the postpartum period are different after first and subsequent births. To ensure that detection of a psychiatric diagnosis in a relative occurred before the postpartum psychiatric diagnosis and was not dependent on the proband mother’s age at childbirth, we assessed whether the relatives had a diagnosis of a psychiatric disorder on or before the proband mother’s 15th birthday, going back to 1970. We adjusted for calendar year and the proband mother’s age at childbirth.
We evaluated the association by determining familial risk, a register-based estimate of the risk of experiencing a postpartum psychiatric disorder when a relative of a proband mother had a psychiatric disorder. We further examined the association of postpartum psychiatric disorders with each of the five hierarchical psychiatric disorders. We used Cox regression analysis to calculate hazard ratios. Given that postpartum psychiatric disorders among proband mothers with a psychiatric history prior to childbirth may be a distinct psychiatric phenotype, we separately examined the associations in proband mothers with and without previous psychiatric history.
To estimate whether the associations between family history of psychiatric disorders and postpartum psychiatric disorders were due to a genetic contribution or shared environmental factors, we repeated the analyses by first-, second-, and third-degree relatives and sex of the relatives with a psychiatric disorder. If an increased risk is due to familial factors attributable to nongenetic factors shared by nuclear families, we would expect to see excess risk only among first-degree relatives. Conversely, if the increased risk is due, at least in part, to a genetic contribution, we would expect to see excess risk among both close and distant relatives in line with their coefficient of relationship.
Statistical analyses were performed using Stata, version 13.1 (
www.stata.com).
Results
The final population-based cohort consisted of 362,462 proband mothers who gave birth to their first child in Denmark between 1985 and 2012. The mean age of proband mothers was 27.0 years (SD=4.3) at time of delivery. Of these mothers, 2,603 (0.7%) experienced a psychiatric disorder within 6 months postpartum and 4,085 (1.1%) within 12 months postpartum (
Table 1).
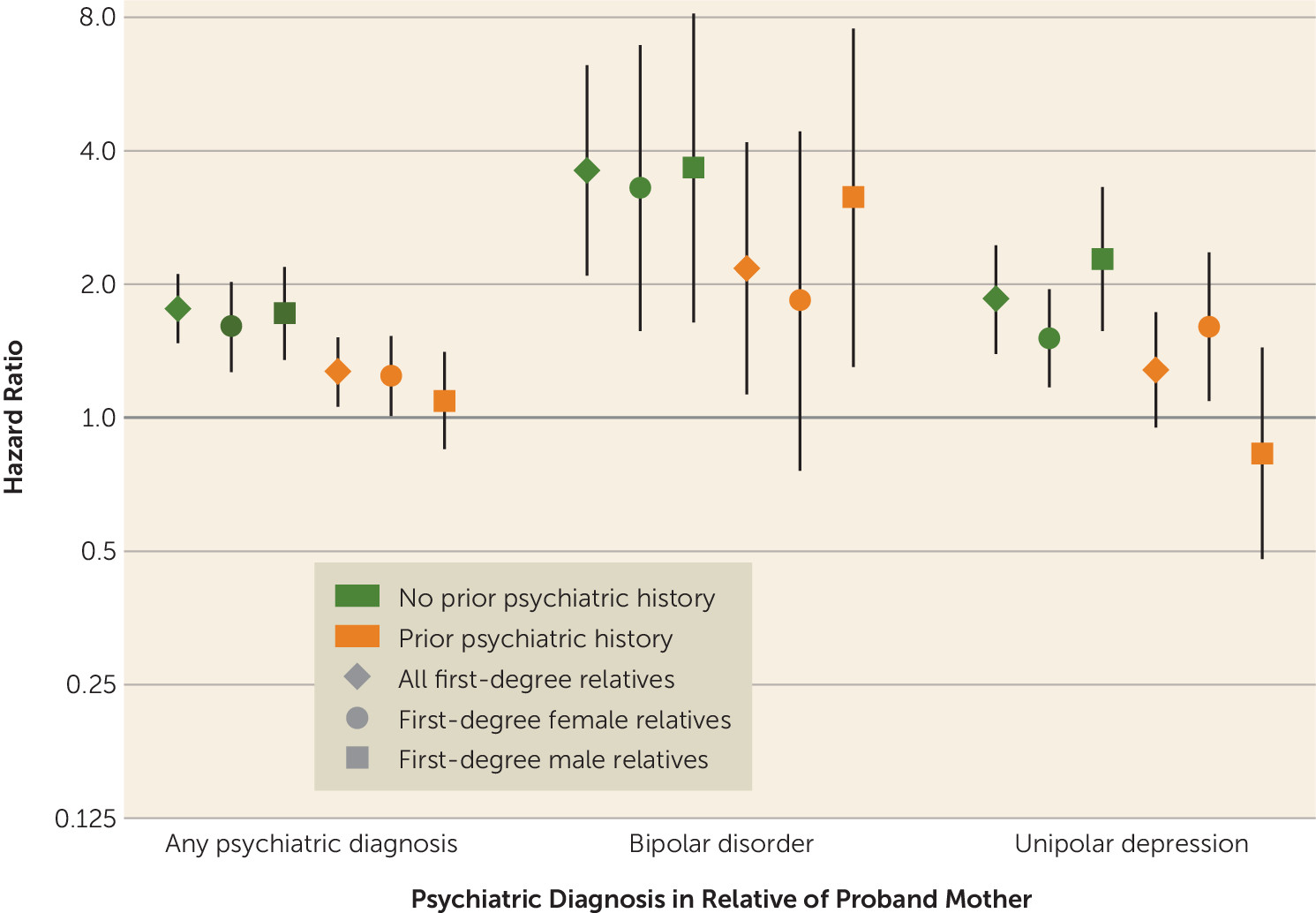
As described, we evaluated familial risk, a register-based estimate of the risk of experiencing a postpartum psychiatric disorder when a relative of a proband mother had a psychiatric disorder. Results are presented for familial risk of postpartum psychiatric episodes within 6 months postpartum, but results were similar for the 0- to 3-month and 0- to 12-month periods postpartum (see Tables S1 and S2 in the
data supplement that accompanies the online edition of this article). Overall, the hazard of experiencing a psychiatric disorder within the first 6 months postpartum was higher among proband mothers with a first-degree relative who had experienced any psychiatric disorder compared with proband mothers whose relatives did not experience any psychiatric disorder (hazard ratio=1.45, 95% CI=1.28–1.65). The hazard ratio of experiencing a postpartum psychiatric episode was highest when proband mothers had a first-degree relative with bipolar disorder (hazard ratio=2.86, 95% CI=1.88–4.35). Familial risk was also elevated for those who had a first-degree relative with schizophrenia (hazard ratio=1.58, 95% CI=1.27–1.95), unipolar disorder (hazard ratio=1.52, 95% CI=1.24–1.87), or other mood disorder (hazard ratio=1.78, 95% CI=1.03–3.06), but not other psychiatric disorders (hazard ratio=0.90, 95% CI=0.70–1.16). The point estimates tended to be larger for proband mothers with no previous psychiatric history (
Table 2,
Figure 2). We found that prior psychiatric history was a strong risk factor for postpartum psychiatric disorders (hazard ratio=8.66, 95% CI=7.97–9.40 for postpartum disorders in women with a prior psychiatric history compared with women with no psychiatric history, adjusted for psychiatric disorders in first-, second-, and third-degree relatives).
Familial risk of postpartum psychiatric disorders was elevated when first-degree relatives had experienced psychiatric disorders, as described above, and slightly elevated for familial psychiatric disorders among more distant relatives (for any psychiatric disorder, second-degree relatives: hazard ratio=1.16, 95% CI=1.02–1.31; third-degree relatives: hazard ratio=1.27, 95% CI=1.03–1.58). More distant relatives share both a reduced coefficient of relationship (see Figure S1 in the online data supplement) and reduced shared family environment.
The familial risk of postpartum disorders in proband mothers whose mothers had psychiatric disorders (hazard ratio=1.50, 95% CI=1.27–1.77 for mothers) was similar to that of proband mothers whose fathers had psychiatric disorders (hazard ratio=1.54, 95% CI=1.27–1.87 for fathers). This pattern persisted for all five diagnostic groups of psychiatric disorders (
Table 2). Likewise, when we assessed familial risk separately in female and male relatives more generally, we did not observe differences by sex for either any psychiatric disorder or specific diagnostic groups of psychiatric disorders for any degree of relationship (
Table 3,
Figure 2).
Discussion
We used linked Danish birth and psychiatric registry data to determine familial risk of postpartum psychiatric disorders associated with family history of psychiatric disorders within five hierarchical diagnostic groups. To our knowledge, this study is the first to use a large population-based cohort to investigate familial risk of postpartum psychiatric disorders with psychiatric disorders outside the perinatal period. Our analysis of first-ever postpartum psychiatric disorders provides evidence of the importance of psychiatric disorders in family members, even among women with no personal history of mental illness.
To our knowledge, this is the first study to address whether familial risk of postpartum psychiatric disorders differs by sex of the family member. Since only women can experience a postpartum psychiatric disorder, previous studies of recurrence risk of postpartum psychiatric disorders have exclusively studied female relative pairs (e.g., mother–daughter, sisters) (
11,
14–
16,
21,
22). However, both males and females experience nonpostpartum psychiatric disorders, and it is unknown whether family history of nonpostpartum psychiatric disorders experienced by male or female relatives differentially influences risk of postpartum psychiatric disorders. Studies of other psychiatric conditions (
35) and small studies of mood disorders in selected populations (
36,
37) have shown some evidence of greater female heritability or transmission, but larger population-based studies of psychiatric disorders have not found sex differences (
10,
38). Consistent with this, we found that although postpartum psychiatric disorders are uniquely female events, a history of psychiatric disorders in male relatives was just as influential as a history of psychiatric disorders in female relatives. Thus, when assessing risk for postpartum episodes, clinicians should inquire about family history of psychiatric disorders broadly and not limit discussion to postpartum psychiatric disorders or psychiatric disorders in female relatives.
We found that familial risk for postpartum psychiatric disorders was higher for family history of bipolar disorder compared with family history of psychiatric disorders, which had previously only been identified for the most severe postpartum psychiatric episodes (
14,
17) or among women with a personal history of mood disorders (
14–
17). Outside the perinatal period, familial risk for bipolar disorder is greater than that of unipolar depression (for bipolar disorder [
10], risk ratio=6.4–7.9; for unipolar depression [
12], risk ratio=2.8). We found similar patterns in our study of psychiatric disorders within the postpartum period; familial risk was higher with a family history of bipolar disorder than for a family history of unipolar depression (for postpartum episodes with bipolar depression, hazard ratio=2.86, 95% CI=1.88–4.35; for postpartum episodes with unipolar depression, hazard ratio=1.52, 95% CI=1.24–1.87). Our estimates, particularly for familial risk of postpartum disorders with familial bipolar disorder, were similar to previous estimates for postpartum mood disorders overall (risk ratio=2.3–3.9) (
14–
16). It should be noted that previous recurrence risk studies of postpartum psychiatric disorders have all been conducted in cohorts of women with a prior psychiatric history, whereas we evaluated familial risk separately in women with and without a prior psychiatric history. The link between bipolar disorder and postpartum psychosis is well established (
6,
39–
42), and recent work in these same data showed that onset of symptoms closer to the time of delivery was associated with a higher risk of conversion to bipolar disorder (
18). These findings, together with our findings in the present study demonstrating that family history of bipolar disorder is more strongly associated with any postpartum psychiatric disorder and not only the most severe episodes, provide evidence for a genetic vulnerability or other etiologically similar mechanisms linking bipolar disorder and psychiatric episodes specifically in the postpartum period, which is supported by the literature (
6,
14,
17,
39–
42).
Our analysis of a large population-based cohort provides the ability to investigate several types of psychiatric events and makes our results more generalizable to the broader population. Most previous studies of familiality of postpartum psychiatric disorders have been conducted in small cohorts or cohorts of high-risk women recruited specifically to study recurrent major depressive disorder and bipolar disorder. This study specifically captured psychiatric disorders in the postpartum period among proband mothers with and without a prior psychiatric history. Previous studies typically have not distinguished between incident episodes and those that may reflect an ongoing psychiatric disorder that recurs during the postpartum period. Differentiating between new-onset episodes and recurrent episodes can have important implications for both screening and treatment. We also considered timing of onset of postpartum psychiatric episodes and separately analyzed three different periods: 0 to 3 months postpartum, 0 to 6 months postpartum, and 0 to 12 months postpartum. There is evidence that the etiology of postpartum psychiatric disorders may differ by timing of symptom onset (
2,
31,
32,
43) and that the first few weeks after childbirth may be the most biologically vulnerable period (
30,
31). However, because our data provide information about timing of diagnosis or treatment but not about the onset of symptoms, there is likely a potential lag between onset of symptoms and when a mother seeks care. This is an intrinsic limitation in nearly all studies of postpartum psychiatric disorders, and we sought to address this limitation by analyzing the 0- to 6-month period. We also selected 0 to 12 months postpartum as a clinically relevant period (
30,
33,
34). External environmental factors change during the first year postpartum, which may influence each time period differently. Despite the potential for differences, we found that the way family psychiatric history affects postpartum psychiatric disorders is similar across all three periods.
Use of registry data improves generalizability to broader populations, but there are also limitations to the data available in the registers. Our data included inpatient hospital admissions and outpatient psychiatric clinic records but not records from general practitioners. Rates of postpartum psychiatric disorders were lower compared with typically reported rates because cases were of patients who obtained psychiatric care in a specialty clinic or hospital, which captured the most severe psychiatric episodes but not patients seeking care from their primary care provider. Therefore, these results are most generalizable to development of severe postpartum psychiatric disorders and potentially not for postpartum psychiatric disorders overall. Additionally, because outpatient diagnoses were not included in the registers until 1995, psychiatric diagnoses prior to 1995 include only the most severe inpatient hospitalizations. To account for the secular trends, we adjusted for calendar year of delivery and age of the proband mother at first delivery in the models. Moreover, to assess how this differentially defined exposure might influence our results, we repeated our analyses in a restricted cohort of mothers who had children born after 1995. A similar trend was observed in this subanalysis, although the interval estimates became wider and less precise because of small numbers of cases. We also acknowledge that our results are only generalizable to primiparous women. Finally, proband mothers were included only if they could be linked to their parents in the registry data. The inability to identify many of the grandparents makes our groupings of second- and third-degree relatives incomplete. Despite our large sample size, there were not enough pairs of sisters or mothers and daughters in whom both experienced incident psychiatric disorders in the postpartum period following the birth of their first child to address the recurrence risk of only postpartum psychiatric disorders. Our sample size also limited our ability to subdivide our outcome into specific types of psychiatric disorders, as we did for our exposure. We also did not see an expected pattern of familial risk aligned with the coefficient of relationship and our study was underpowered to evaluate familial risk by type of disorder for third-degree relatives, both likely because of incomplete identification of third-degree relatives.
Predicting who will experience a postpartum psychiatric disorder is a challenge but also of great importance. The results of this study provide compelling evidence that assessment of risk for postpartum psychiatric illness, with a particular focus on history of bipolar disorder, should include inquiring about family history of psychiatric disorders in any male or female first-degree relative. Thus, inquiring about family history in fathers and brothers is as important as obtaining a history of postpartum psychiatric disorders in mothers and sisters. Furthermore, as expected, we found personal psychiatric history to be a stronger independent predictor of postpartum psychiatric disorders than family history. However, we found associations of family history of psychiatric disorders to be stronger among women without a personal psychiatric history, indicating that family history may be particularly helpful in a risk assessment tool for new-onset postpartum psychiatric episodes among women with no record of psychiatric disorders. Previously, a woman who has a brother with bipolar disorder but no personal history of mental illness would not necessarily be identified as being at higher risk for experiencing a postpartum psychiatric disorder. However, this research provides evidence that such characteristics may identify novel risk groups to which clinicians could direct additional screening efforts, earlier education about symptoms, or earlier referral to mental health resources. Few clinical practice guidelines include family history, but those that do suggest planning the timing of pregnancies in periods of stable mood (
44) and increasing surveillance for symptoms of postpartum psychosis in the first 2 weeks after childbirth (
45), which should also be considered for these novel risk groups.
Clinical practice guidelines in the United States have recently been updated to reflect a growing emphasis on the importance of perinatal mental health screening, but the current guidelines of the U.S. Preventive Services Task Force (
46) and the American College of Obstetricians and Gynecologists (
33) do not include family history as a consideration for postpartum psychiatric disorders. This is in contrast to other women’s health conditions, such as breast cancer, in which family history of breast cancer in a first-degree relative is described extensively as an important screening consideration, despite the magnitude of familial risk being similar to that of postpartum psychiatric disorders (
47). Therefore, obtaining a family history of psychiatric disorders is highly valuable information that should be acknowledged as an important factor in identifying at-risk women and operationalized in clinical practice to improve prediction of risk for postpartum psychiatric illness.