T
o the E
ditor: The article by Olfson and colleagues (
1), published in the August 2017 issue of the
Journal, reports findings from a study of risk factors for suicide following nonfatal deliberate self-harm in a national cohort of Medicaid-financed adults. A main finding of the study was that patients using a violent method, firearms in particular, for the initial episode of nonfatal self-harm were at a very high risk of committing suicide later—especially during the first month following the initial self-harm. As pointed out by Olfson et al. (
1) and by Nordentoft et al. (
2) in an accompanying editorial, these findings call for action. Specifically, Olfson et al. suggest that adults treated for deliberate self-harm, especially those having used a violent method, should be carefully assessed and closely followed to reduce the risk of repeat self-harm and suicide (
1). Nordentoft et al. point to the possibility that restricting access to violent means of suicide, firearms in particular, is likely to be lifesaving among individuals surviving deliberate self-harm (
2). Both suggestions seem highly relevant for clinical practice and underline the value of the study conducted by Olfson and colleagues.
Another finding reported by Olfson et al. (
1) was that male sex was a strong risk factor for suicide following nonfatal deliberate self-harm. Male sex is among the most consistently reported risk factors for suicide and, according to the World Health Organization, the global male-to-female ratio of age-standardized suicide rates was 1.7 in 2015 (
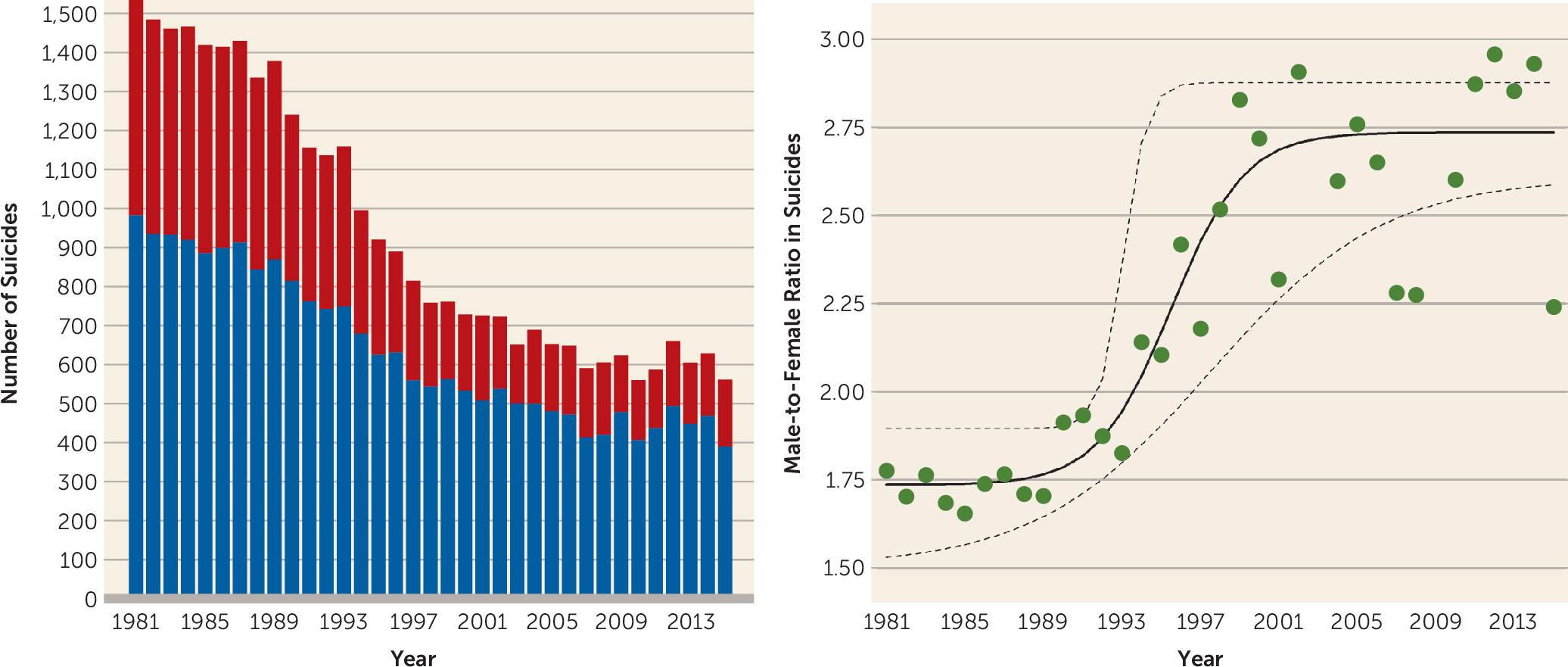
3). In Denmark, where the number of suicides has been more than halved over the past three decades, the male-to-female ratio in suicides has increased dramatically over the same period (
Figure 1). Notably, suicide statistics in the United States have shown the exact opposite trend. From 1999 through 2014, the age-adjusted suicide rate in the United States increased by 24%—and more so for women (a 45% increase) than for men (a 16% increase)—resulting in a decrease in the male-to-female suicide rate ratio from 4.5 in 1999 to 3.6 in 2014 (
4).
A potential explanation for the increase in the male-to-female suicide ratio that took place in Denmark from 1981 to 2015 is that the reduction in suicides during this period was partly driven by improved treatment of depression (and other mental disorders), which may have had a relatively larger beneficial effect on the female suicide rate compared with the male rate. Indeed, such a sex-differential effect was observed in the so-called Gotland Study from Sweden in which education of general practitioners in the detection and treatment of depression gave rise to a significant reduction in the female suicide rate, while the male suicide rate remained virtually unaffected (
5). This observation led to the conception of the “male depressive syndrome” as operationalized by the Gotland Male Depression Rating Scale (
6). This male depressive syndrome is characterized by irritability; restlessness; lowered stress threshold; low impulse control; acting-out behavior; substance abuse; and family history of depression, risky behavior, or suicide attempts (
6).
Based on the line of thinking outlined above, it seems likely that a substantial fraction of the relatively large number of male suicides in both the cohort described by Olfson et al. (
1) as well as in the world’s population at large (
3) may be attributable to unrecognized and untreated male depression (
5). I therefore urge my colleagues to raise awareness about male depression and to subject this understudied phenotype to further investigation.