Against this background, this essay reviews a radical idea: A single dimension is able to measure and maybe even explain a person’s liability to mental disorder, comorbidity among disorders, persistence of disorders over time, and severity of symptoms. This is a relatively new idea but one with surprising historical roots. It is an idea that is being vigorously researched. It may be wrong or it may be useful, or it may end up somewhere in between. Our goal here is to briefly review it, articulate its research and treatment implications, and suggest testable hypotheses and research directions.
How Did We Get Here? A Brief History of Research on the Structure of Psychopathology
The history of classification in psychiatry—from the four humors of ancient Greek medicine to Kraepelinian natural disease entities to the gathering of uniform health statistics in mental hospitals to DSM—has been told by others. The present story begins with DSM-III, which heralded the arrival of explicit criteria for reliably diagnosing each disorder, along with interview schedules for use in research and clinical settings (
4).
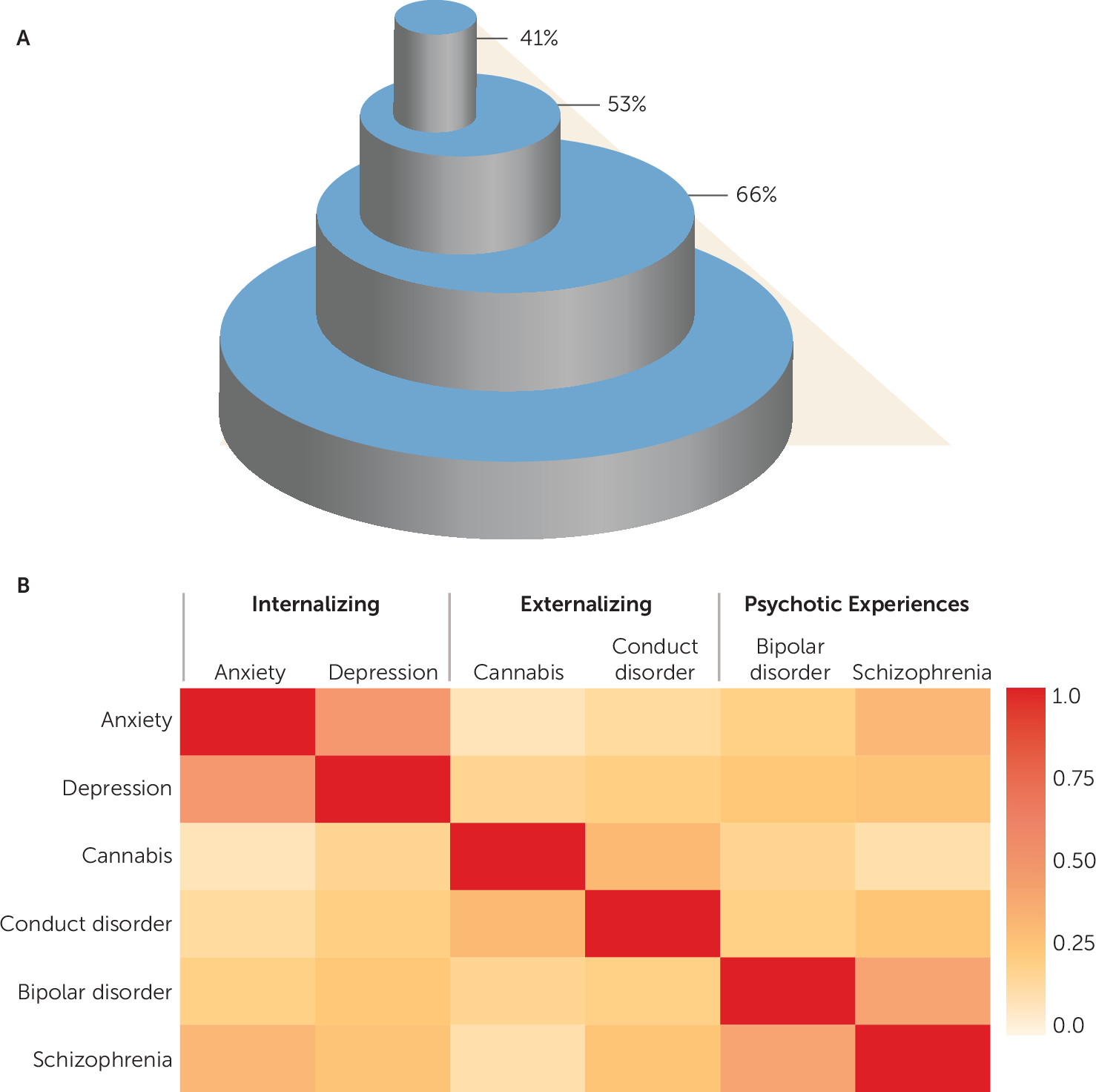
One of the earliest empirical challenges to DSM-III and its successors was comorbidity, the coexistence of two or more conditions or disorders (
5). Comorbidity rates are very high in psychiatry (
6); most individuals who meet diagnostic criteria for one disorder meet diagnostic criteria for a second disorder; most who meet criteria for two meet criteria for a third; and so forth (
Figure 1A). Such high rates of comorbidity suggested the possibility that there may be a more parsimonious structure to psychopathology than implied by nosologies that identify many separate and distinct disorders. In the mid-1990s, clinical scientists called on researchers to study patterns of comorbidity in order to “elucidate the broad, higher-order structure of phenotypic psychopathology” (
7).
We responded to this call by using confirmatory factor analysis to evaluate alternative hypotheses about the latent structure underlying 10 common mental disorders in adults (
8). In contrast to the prominence of categorical models in the classification of adult psychopathologies, dimensional models had long enjoyed success in research on the classification of childhood psychopathologies, and empirical studies of children had converged on two primary dimensions as a way to characterize childhood disorders: these were labeled internalizing (including anxious and depressive symptoms) and externalizing (including aggressive, delinquent, and hyperactive-impulsive symptoms) (
9). We could see no reason why this highly replicable two-dimensional structure of psychopathologies should suddenly vanish when research participants and patients reached age 18. Indeed, our data suggested that a two-factor model could account for the comorbidity of different adult disorders—a two-factor model that resembled that of childhood psychopathologies. This initial finding led to the hypothesis that common DSM psychiatric disorders in adults may be characterized by two underlying psychopathological processes: an internalizing dimension indicating liability to experience mood and anxiety disorders, such as major depression, generalized anxiety disorder, panic disorder, and social phobia, and an externalizing dimension indicating liability to experience substance use disorders and antisocial disorders. Multiple studies in different parts of the world, in different age groups, in general community samples, and in clinical populations have supported the utility of using this empirical framework to understand and classify common adult mental disorders (
10,
11).
Notably absent from this conceptualization were psychotic experiences, largely because most of the data used to evaluate the structure of psychopathology came from community studies and epidemiological surveys that did not assess psychotic symptoms; it was presumed that people could not or would not report on such symptoms in a survey. But emerging research on the continuum of psychosis brought attention to the fact that psychotic symptoms were more commonly experienced in the general population than previously thought and could actually be reported (
12). This possibility, it should be noted, had been anticipated in Achenbach’s childhood classification system, whose thought problems dimension inquired about seeing and hearing things and strange ideas (
9). The empirical model of psychopathology was consequently expanded to accommodate a third dimension, psychotic experiences, indicating liability to experience dissociation, disorganized thoughts, unusual beliefs, fantasies, and hallucinations, with some lingering uncertainty about whether mania, obsessions, and compulsions belong on this spectrum too (
1,
13).
The three-factor empirical model was intended to impose sense and order on the comorbidity that was observed between many closely related pairs of disorders, such as anxiety and depression (internalizing), substance dependence and conduct disorder (externalizing), and bipolar disorder and schizophrenia (psychotic experiences) (
Figure 1B). But three lines of evidence suggested that even these higher-order dimensions overlapped to a considerable degree. First, cross-sectional studies showed that covariation is not limited to closely related disorders such as anxiety and depression, but transcends diagnostic domains; the correlations between the higher-order dimensions internalizing, externalizing, and psychotic experiences hover around 0.5 (
13). Second, longitudinal data revealed strong patterns of both homotypic and heterotypic sequential comorbidity; across the life course, mental disorders at one time predict the future occurrence of the same disorder as well as the future occurrence of different disorders (
14–
16). Third, psychiatric disorders do not simply breed true; parental psychopathology is strongly linked with offspring psychiatric disorders, but with very little specificity (
17–
19).
The upshot is that psychiatric phenotypes share a large amount of variance, at a given point in time, across the life course, and across generations. This knowledge gave rise to the new idea that there may be one underlying factor that summarizes individuals’ propensity to develop any and all forms of common psychopathologies. Whereas the correlated factor model identified propensities to specific forms of psychopathology (e.g., internalizing, externalizing, psychotic experiences) (
Figure 2A), the general factor model suggested that there is one common liability to all forms of psychopathology (
Figure 2B,C), an idea harkening back to psychometric research on intelligence, which first proposed a general factor that is common to all items on mental tests. Indeed, a useful way to think about the meaning of a general factor in psychopathology is by analogy, in relation to cognitive abilities. Cognitive abilities are dissociable into separate abilities, such as verbal skills, visuospatial skills, working memory, and processing speed. Nonetheless, the general factor in intelligence (called the “g” factor) summarizes the observation that individuals who do well on one type of cognitive test tend to do well on all other types of cognitive tests (
20–
22). The g factor accounts for the positive correlation among all test scores. Just as there is a general factor of cognitive ability, it is possible that there is also a general factor of psychopathology. Lahey et al. (
23) provided the initial evidence for this model, and subsequently we replicated it and called the general factor “
p” (
24).
Interestingly, we have learned that this idea was anticipated by Ernest Jones (
25), the neurologist and psychoanalyst as well as Freud’s biographer, who offered this prediction in his 1946 valedictory address to the British Psycho-Analytical Society:
There may well be an innate factor akin to the General Intelligence G, the nature of which it still remains to elucidate, but which may be of cardinal importance in the final endeavour to master the deepest infantile anxieties, to tolerate painful ego-dystonic impulses or affects, and so to attain the balanced mentality that is our ideal.… If such a factor can ever be isolated it may prove to have a physiological basis which will bring us back to the often neglected problems of heredity. The capacity to endure the non-gratification of a wish without either reacting to the privation or renouncing the wish, holding it as it were in suspense, probably corresponds with a neurological capacity, perhaps of an electrical nature, to retain the stimulating effects of an afferent impulse without immediately discharging them in an efferent direction (
25, p. 10).
In the brief period following initial reports, evidence has quickly accumulated that establishes the replicability of a general factor of psychopathology (
26). This evidence has involved both direct and conceptual replications (
27). Several features of this burgeoning research merit mention: A general factor of psychopathology is identifiable in studies that assay internalizing, externalizing, and psychotic symptoms among children, adolescents, and adults; in different parts of the world; when these symptoms are reported on by different sources, including self-reports, parent reports, and teacher reports; and even though the instruments that assay symptoms do not always cover the same exact content (e.g., some studies do not evaluate psychotic symptoms, and other studies also evaluate personality disorders) (
17,
28–
33).
What Does the p Factor Mean?
Studies of the so-called underlying structure of psychopathology extract latent (i.e., unobserved) variables from the correlations among symptoms and disorders. But the statistical models are agnostic about—and certainly do not reveal—the causes of the correlations (
34,
35). It is thus reasonable to ask whether the
p factor is statistical tomfoolery or a window onto new insights. We think the latter, but before discussing these possibilities, there are alternatives that future research will need to evaluate and rule out.
First, whereas latent variable analysis posits that the positive correlations between symptoms (as well as disorders) arise from a g-like causal factor, there is an alternative view, called network analysis. The network approach argues that the positive correlations could also result from causal processes between symptoms (as well as disorders) (
36). This is depicted in
Figure 2D, which makes no recourse to a common latent pathogenic trait or pathway. This alternative conceptualization of the correlations among psychiatric symptoms has animated methodological debates (
37,
38). This conceptualization also has radical clinical implications. It suggests that intervening on a central keystone symptom or disorder can bring about effective treatment by breaking up the network of causation (
39).
Second, it is possible that
p is not a substantive dimension but merely a response style. According to this scenario,
p reflects individual differences in the tendency to report on oneself in a generally negative or positive way. To address this possibility, several studies have used non-self-report data (e.g., parent, teacher, or peer reports) to identify a general factor of psychopathology, and at least one study explicitly modeled reporting-source effects when evaluating
p (
28). But just as it is difficult to tease apart substance from social desirability bias when using self-reports, it is difficult to tease apart substance from an evaluative bias when using reports by informants (
40). The key to testing the response style hypothesis may lie in external validation. For example, evidence that
p predicts objective, real-world life outcomes (e.g., suicide) suggests that it may be indexing something substantive, not merely something about how people behave while data are being collected (
24,
41).
Third, a different nonsubstantive possibility is that
p is not a consequence of a unitary cause but instead reflects a unitary outcome. That outcome could be dysfunction in a person’s life (
42). According to this scenario, what all psychiatric disorders have in common is not a cause but impairment that is secondary to the disorders. Thus, in contrast to
Figures 2B and 2C, where the latent variable is thought to cause the various disorders, in
Figure 2E the latent variable is actually made up of the various disorders that lead to common impairments.
But suppose there really is something substantive that accounts for meaningful variance across major forms of psychopathology. What is it?
One hypothesis is that
p represents a diffuse unpleasant affective state, often termed neuroticism or negative emotionality (
26). Cross-sectional and longitudinal studies show that neuroticism predicts many different psychiatric disorders (
43). Twin studies reveal common genetic influences on negative emotionality and a general factor of psychopathology (
44). But it is still not clear whether neuroticism is a cause or perhaps is better regarded as a marker of nonspecific general risk for psychopathology (
45). Indeed, this may explain why neuroticism-saturated screening instruments such as the General Health Questionnaire (
46) and the Kessler Psychological Distress Scale (
47) are so good at detecting many different common mental disorders.
A second hypothesis, which echoes Ernest Jones, is that the core functional mechanism in
p is poor impulse control over emotions (
48). This subsumes a variety of deficits in response inhibition, including impulsive speech and action in response to experienced emotions, cognitive impulsiveness as reflected in rumination about the causes and consequences of one’s distress, and impulsive overgeneralization from negative events. Research about the personality correlates of
p supports this perspective; it is not just high neuroticism but the toxic blend of antagonism, weak impulse control, and neuroticism that sets high
p scores apart (
24,
31). Additional support for this hypothesis comes from longitudinal research that shows that poor childhood self-control, reflecting emotional dysregulation and executive deficits, cuts across all disorder liabilities and is a salient early developmental predictor of the
p factor (
49).
A third hypothesis is that deficits in intellectual function characterize
p. Individuals with higher levels of
p fare less well on tests requiring attention, concentration, and mental control, as well as visual-perceptual processing speed and visual-motor coordination (
17,
24,
31). These deficits are not simply a consequence of lifelong disorders; they are already present in early life, before the onset of most disorders (
Figure 3A). Attesting to the ecological validity of these deficits, individuals with high levels of
p experience cognitive problems in their everyday life according to people who know them well (
Figure 3B). Several testable hypotheses suggest themselves. Deficits in cognitive reserve, as reflected in low childhood IQ, could be related to
p because 1) low cognitive ability is a marker of neuroanatomical deficits that increase vulnerability to multiple different common psychiatric disorders; 2) low cognitive ability increases both exposure to
and vulnerability to life stressors; or 3) low cognitive ability reduces mental health literacy, which precludes early help-seeking, preempts access to evidence-based care, and reduces treatment adherence (
50,
51).
A fourth hypothesis (and the one that intrigues us most) is that
p captures the disordered form and content of thought that permeates the extreme of practically every disorder (
24). Any individual who carries a strong general psychopathology liability might, if their disorder grows severe enough, experience psychotic thought processes, whatever the presenting diagnosis; that is, unwanted irrational thoughts are not just for the formal psychoses. Disordered thought processes occur in the context of affective disorders, anxiety disorders, eating disorders, posttraumatic stress disorder (PTSD), somatoform disorders, dissociative disorders, substance use disorders, and antisocial disorders. Disordered thought processes are illogical, unfiltered, tangential, and reality-distorted and -distorting cognitions. Examples include not only delusions and hallucinations but also thought problems such as difficulty making decisions, rumination, body image disturbances, intrusive thoughts, irrational fears, reexperiencing trauma, dissociative states, beliefs that something terrible will happen if a behavior is not performed, hostile attributions made in response to ambiguous social situations, and attributing failure to internal, stable, and global causes. This leads to the testable proposition that the symptoms of disordered thought processes will prove to be the most diagnostic elements of
p. Consistent with this hypothesis, research on the link between mental disorders and making a plan to end one’s life (arguably among the most disordered of thoughts) shows that suicide attempts are not due to specific disorders but to a broad general psychopathology liability (
52).
How Does p Develop?
If
p is quantitatively distributed in the population, with extreme scores signaling neuroticism, emotion dysregulation, intellectual impairments, and disordered thought, what marks its developmental progression? One possibility that we hypothesized (
24) is that many young children exhibit diffuse emotional and behavioral problems, fewer go on to manifest a brief episode of an individual disorder, still fewer progress to develop a persistent internalizing or externalizing syndrome, and only a very few individuals progress to the extreme elevation of
p, ultimately emerging with a psychotic condition, most likely during late adolescence or early adulthood. This hypothesized developmental progression is supported by evidence from a unique prospective adoption study that showed that biological mothers’
p factor predicted their adopted-away children’s internalizing and externalizing problems by age 3, suggesting the early-life emergence of pleiotropic genetic effects (
53,
54). This developmental progression would also require evidence that brief episodes of single disorders are widespread in the population, which is supported by the high lifetime prevalence rates of individuals with disorders over years of follow-up in longitudinal studies (
55,
56). A developmental progression would also require that individuals who manifest psychosis have an extensive prior history of many other disorders, which has been reported (
57,
58). And, moreover, a developmental progression would anticipate that when individuals are followed long enough, those with the most severe liability to psychopathology will tend to move in and out of diagnostic categories. Today’s patient with schizophrenia was yesterday’s boy with conduct disorder or girl with social phobia (and tomorrow’s elderly person with severe depression). This developmental progression hypothesis is consistent with evidence that sequential comorbidity is the rule rather than the exception (
59) and that individuals experiencing sequentially comorbid disorders also exhibit more severe psychopathology (
16). To the best of our knowledge, this entire developmental progression—from mild, diffuse emotional and behavioral problems to persistent syndromes to extreme, impairing comorbid conditions—has not been described in the same individuals followed over time, and predictors of age-graded transitions along the hypothesized progression have yet to be evaluated.
The Quixotic Pursuit of Specificity and the Promise of Nonspecific Shared Pathogenesis
Taxonomists are often caricatured as falling into two camps: splitters, who see differences between things and divide them into fine categories, or lumpers, who see similarities between things and group them into broad categories. Efforts to rethink psychiatric diagnoses have historically been dominated by splitters. This is reflected in efforts to identify subtypes of a disorder (e.g., depression, attention deficit hyperactivity disorder) on the basis of symptom profiles, or dysfunction in mood-related brain circuits, or biomarkers. The p factor is lumping with a vengeance. The question is whether such lumping can help to make sense of data and whether it can inform treatment.
When searching for the causes of mental disorders, nonspecific variables are often dismissed as unimportant (
60). And yet psychiatry has had difficulty finding single-disorder loyalty in causes. The existence of
p may explain why it has been so difficult to identify etiological factors that confer differential risk to one specific psychiatric disorder but not another. We do not argue that disorder-specific causes can never be found. Just as the existence of g does not preclude a specific cause (e.g., stroke, tumor, head injury) from disrupting one isolated mental function, the existence of
p would not preclude a specific cause from generating an isolated syndrome. Instead, we suggest that specific causes will be challenging to find because if a disorder’s causes covary in a dose-response fashion with the disorder’s severity, then the same causes may characterize other disorders too, because it is severe disorder that tends to be comorbid, concurrently and sequentially, reflecting
p. The hypothesis of shared pathogenesis raised by
p extends to other kinds of variables studied in psychiatry—including biomarkers (
61), consequences (
52), and treatments (
62). We think the absence of causal specificity invites researchers in genetics, neuroscience, and developmental psychopathology to focus on
p itself.
The Genetics of p
The targets of genetic discovery research are typically distinct disorders. Genome-wide association studies (GWAS) have concentrated on increasing sample size and refining phenotypes of individual disorders, with the aim of collecting ever-larger numbers of homogeneous cases to compare with healthy control subjects. There have been suggestions that targeting psychiatric spectra (such as the externalizing dimension) may be a useful adjunct to discovery research (
63), but in the past, the response in the psychiatric genetics community has been lukewarm. Responding to the suggestion that research about the
p factor may stimulate the study of dimensions that cut across traditional disorders, one community member in a chatroom demurred: “So, let’s keep studying schizophrenia and bipolar disorder and not allow ourselves to be RDoC’d out of existence.” Never mind that research on the
p factor and the Research Domain Criteria (RDoC) (
64) have different scientific histories and share little in common (see the Conclusions section); the chatroom statement is revealing because it expresses reluctance to study general liabilities in the population rather than diagnosis-specific cases in a clinic. Interestingly, it turns out that many disorders do share common genetic risks, as revealed by both biometric and molecular genetic studies, raising the possibility that the
p factor may be a reasonable target for genetic investigation after all.
Historically, family, twin, and adoption studies examined one disorder at a time, revealing that every psychiatric disorder is under significant genetic influence (
65). These biometrical studies were then extended to test whether there are common genetic influences on different disorders. This work documented the fact that common genetic influences account for the covariation between different internalizing disorders (e.g., depression and anxiety) and between externalizing disorders (e.g., substance use and antisocial disorders), as well as between schizophrenia and bipolar disorder (
66). Apparently, genetic factors are important not only in the etiology of particular disorders, but shared genetic etiology of core psychopathological processes at the higher-order construct level explains why disorders co-occur in the population (
67). Extending the logic of such inquiries further, the most ambitious study to date (
68) used national register data from over 3 million siblings of various genetic relatedness (full and half siblings) to test the hypothesis that depression, anxiety, attention deficit hyperactivity disorder (ADHD), alcohol use disorder, drug abuse, violent crime, schizophrenia, and schizoaffective disorder share genetic influence. The results provided evidence that a general genetic factor influences all forms of psychopathology.
At the molecular level, it appears that genetic effects on psychiatric disorders are both polygenic and pleiotropic (
69). Cross-disorder comparisons are producing confirming evidence that different disorders may share some of the same illness-associated genetic variation (
70,
71), which may be related to shared global gene expression patterns across different disorders (
72). In addition, there is evidence that genetic risk variants discovered for specific conditions have more general pleiotropic effects; for example, genetic risk variants discovered for ADHD appear to be shared by a general liability toward childhood psychopathology (
73). Identifying genes that are associated with more than one psychiatric disorder might help explain the pathogenesis shared among different psychiatric disorders (
74). But whereas research to date has sought to identify genetic variants that are shared by two or more distinct disorders, one hypothesis is that genetic discovery could be made more efficient by studying the
p factor itself as the phenotype in GWAS. On statistical grounds, studying
p is attractive because power is enhanced when analyzing quantitative traits, when phenotypes are defined using multivariate approaches (e.g., by measuring and analyzing multiple correlated traits), and when multiple traits are analyzed jointly (
75,
76). But on design grounds, there are formidable challenges to putting together adequately powered discovery studies of
p. Case-control studies are not ideal designs in which to calculate a general factor of psychopathology because the selective sampling of clinic cases may yield biased correlations among the full range of dimensions of psychopathology. This is further compounded by the use of exclusionary criteria in case definition, which can artifactually distort correlations between dimensions of psychopathology (e.g., ADHD cases screened to exclude conduct disorder, or depression cases screened to exclude substance dependence, do not accurately represent ADHD and depression). Alternatively, as more population-based studies are turning their attention to measuring the structure of psychopathology—including
p—it may be possible to jointly analyze data from those studies that also have DNA. But because not all such studies have sampled the same psychopathology content, harmonization of the
p factor may be needed for integrative purposes (
77). Finally, new big-data initiatives, such as the UK Biobank and the National Institutes of Health’s All of Us Research Program, will be a boon to this discovery work, but only if they are encouraged to collect comprehensive mental health data on multiple dimensions of psychopathology rather than sampling a small fraction of common disorders.
The Neuroscience of p
Some commentators have questioned the utility of a general factor that underlies shared risk for a wide range of common mental disorders by suggesting that it is analogous to arguing that all forms of physical illness can be represented as a general state of being “unwell” (
78). However, this analogy ignores the fact that all mental disorders are expressed through dysfunction of the
same organ (brain), whereas physical diseases such as cirrhosis, emphysema, and diabetes are manifested through dysfunction of different organ systems. Viewed from this perspective, perhaps the search for nonspecificity in psychiatry is not unreasonable.
To date, psychiatric neuroimaging has offered (and held out) hope of aiding differential diagnosis by identifying specific pathological features that manifest in one psychiatric condition and not in others (
79). The difficulties associated with the search for specificity are highlighted in a meta-analysis of task-related brain activation in people with various mental illnesses compared with healthy control subjects (
80). The meta-analysis focused on functional MRI studies of schizophrenia, bipolar disorder, obsessive-compulsive disorder, anxiety disorders, and major depressive disorder and analyzed the results of brain activation in tasks that were intended to tap mental processes in cognitive, interpersonal, reward, and threat circuits. While there was a tendency for parts of the brain (e.g., amygdala, hippocampus) to be activated in people who met criteria for different psychiatric disorders, there were few differences between the different disorders; that is, patient-control differences were observed in the same brain regions, regardless of the disorder. It is tempting to overgeneralize from these results, but caution is required; after all, the meta-analysis selected only those studies that found significant differences between case subjects and healthy control subjects, and it did not include disorders on the externalizing spectrum. At minimum, these results serve as a reminder of the joint perils of comparing cases to healthy controls while also failing to compare cases against other psychiatric controls (
81). Beyond that, it can be hoped that these results may also stimulate efforts to probe the shared (versus specific) neural bases of psychiatric problems.
Transdiagnostic headway is being made using both structural and functional imaging studies (
82). A meta-analysis of volumetric differences in six diagnostic groups (schizophrenia, bipolar disorder, obsessive-compulsive disorder, depression, anxiety, and addiction) pointed to reduced gray matter volume across diagnoses in three brain regions: the dorsal anterior cingulate cortex and the left and right anterior insulae. This collection of regions is thought to be part of a network that is involved in attention and cognitive control (
83). A parallel analysis of brain activation in people with these disorders found evidence for transdiagnostic alterations in regions overlapping with those identified in the gray matter analysis, suggesting that cognitive control impairments are shared by all of the disorders analyzed (
84).
As in genetic discovery research, a question for neuroscience is whether there is anything to be gained by focusing on the general factor of psychopathology per se, rather than by searching for commonalities shared by different disorders. An initial study of over 1,000 adolescents and young adults (
85) found that higher
p factor scores were associated with altered intrinsic connectivity of the anterior cingulate cortex, which echoes the aforementioned transdiagnostic meta-analyses. Another study (
86) conducted exploratory whole-brain analyses of the structural integrity of white matter pathways and regional gray matter volume correlates of the
p factor in a sample of 1,200 undergraduate students. The results implicated alterations in the structure of cerebellar circuitry, in the form of reduced white matter integrity of pontine pathways encompassing cerebellar afferents and reduced cerebellar gray matter volume. Although the cerebellum is most widely known as a region involved in basic motor processing and coordination, it has also been implicated in higher-order cognitive and emotional processes through its structural and functional connectivity with various cerebral structures, especially the prefrontal cortex (
87). More generally, the cerebellum has been hypothesized to function as a “forward controller,” creating internal models of how a given behavioral output will fit with contextual information (
88). Thus, reduced cerebellar gray matter volume and pontine white matter integrity associated with higher
p factor scores may reflect impaired processing and monitoring of information—including one’s own thoughts and emotions—necessary to guide behavior. This possibility fits the hypothesis that
p captures the disordered thought processes that permeate the extreme of practically every disorder.
These are early days. Transdiagnostic studies have relied primarily on meta-analytic strategies to search for commonalities, but this method may fall prey to publication bias. Neuroscience investigations of the p factor itself are too new to have accumulated a replication record. It remains to be seen whether psychiatric disorders reflect aberrations in shared neural substrates and networks, in contrast to the specificity implied and pursued by research that adheres to current nosologies.
Psychological Trauma and p
Different disorders share common biological risks. Do they have the same or different environmental risks? In the realm of cognitive development, it has been hypothesized that many of the same genes that influence one ability (e.g., reading) are also the same genes that influence other abilities (e.g., mathematics) but that what differentiates abilities are environmental influences. This has been termed the “generalist genes, specialist environments” hypothesis (
89). While there has been some suggestion that this model might also apply to some psychiatric disorders (
90), we are much more struck by a commonality across psychiatric disorders: trauma exposure.
Consider childhood maltreatment, whose multiple forms (including physical, sexual, and emotional abuse, and neglect) appear to share nonspecific consequences. Three research findings stand out. First, it is more difficult to identify a disorder to which childhood maltreatment is
not linked than to identify a disorder to which it
is linked with specificity (
91). Childhood maltreatment is a risk factor in the history of people with mood disorders, anxiety disorders, behavioral disorders, and substance use disorders as well as schizophrenia, psychosis, and psychotic-like experiences and symptoms (
92–
94). Childhood maltreatment also predicts disorder that is comorbid, persistent, and even treatment resistant (
95–
97). Research on the higher-order structure of psychopathology documents the fact that childhood maltreatment influences broad, general factors (e.g., internalizing, externalizing) common to multiple different types of disorders rather than those that give rise to specific disorders or clusters of symptoms (
98,
99). And, at the general factor level, initial tests suggest that the association between maltreatment and disorders on the internalizing and psychotic experience spectrum are accounted for by
p, although
p does not fully account for all of the link from childhood maltreatment to externalizing problems (
100,
101). Second, different forms of maltreatment appear to have equivalent consequences (
102). Physical abuse, sexual abuse, and neglect are all similarly associated with risk of psychiatric disturbance; when stronger effects are observed for some maltreatment types (e.g., sexual abuse), this is not so much due to the specific experience per se as it is attributable to excess polyvictimization associated with that experience (
100). Third, while traumatologists have trained their lenses on childhood exposures, at least in human studies there is no decisive evidence pointing to sensitive periods during development in which maltreatment becomes psychically embedded. In fact, some have hypothesized that exposure to maltreatment during adolescence may be associated with a physiological response that is both larger in magnitude and more difficult to down-regulate than an equivalent exposure in childhood (
103). In sum, the most compelling evidence about the psychiatric sequelae of trauma points to the toxicity of cumulative, recurring, and multiple exposures operating in a dose-response manner. We use the word “sequelae” advisedly. When evaluating research on maltreatment, the elephant in the room is whether maltreatment “causes” mental health problems. Children cannot be randomly assigned to maltreatment to evaluate its effects, and causal inference has been constrained by observational designs. Designs are required that rule out alternative, noncausal explanations—longitudinal twin studies that control for preexposure vulnerabilities and that can rule out unmeasured genetic and shared environmental risk factors by comparing monozygotic twins with different trauma histories. Studies with such designs lend confidence that causal effects are likely present (
100,
104).
What this research (and clinical experience) implies is that loss, intimidation, humiliation, betrayal—fundamental threats to one’s physical and psychological safety—increase the risk of mental disorder, broadly. How this happens most likely involves an etiological chain with at least four processes.
Stress embedding occurs as neural changes in threat systems lay down a vulnerability to later disorders. Some theorists have speculated that these neural responses may reflect an initially adaptive response—rather than a damaged response—but that in the long term this response becomes increasingly maladaptive when it is not recalibrated in new, nonthreatening contexts (
105,
106).
Stress generation occurs as individuals who are maltreated behave in ways that contribute to the occurrence of other negative events in their lives, including further and new forms of victimization (revictimization) (
101,
107,
108).
Stress sensitization occurs as individuals who are exposed to early maltreatment are more vulnerable to disorders that are triggered by later, proximal stressors, many of which are brought about through stress generation (
109). Finally, although maltreatment is a potent risk factor for developing psychiatric disorders, it is apparent that there are marked individual differences in response to it, and many people who are victimized remain healthy (
110), suggesting
stress sensitivity (a process distinct from stress sensitization), which refers to the hypothesis that some individuals are more or less sensitive to stress due to a putative, most likely genetically mediated trait (
111,
112). Unfortunately, the study of such gene-by-environment interactions was swept up (and almost away) in the hand-wringing about candidate gene research. This was because of the inappropriate conflation of a hypothetical process (genetic sensitivity to the environment) and the availability of methods for studying it (early studies only had candidate genes at their disposal) (
113). It is hoped that new methods and designs, including large-scale studies of populations exposed to childhood adversity, can invigorate the search for genetic vulnerability and resilience to the environmental cause of a general liability to psychopathology (
114). Constructing and decoding this full etiological chain to
p—rather than single-adversity–single-disorder research—is a priority.
Implications of p in Treatment and Prevention of Mental Disorders
The idea of
p will seem unsurprising to mental health practitioners because although comorbidity is common among respondents in epidemiological surveys, it is even more intensely concentrated among the subset of patients who seek treatment (
115–
117). In our view, prescriptions related to treatment are premature, given that research into
p is still young. Therefore, in this section we adopt a “what if” view: If
p were real, how might clinical practice change? The most radical implication of
p is that clinicians could potentially deliver the same treatment to all, regardless of a patient’s diagnosis at the time he or she presents to the clinician. This hypothesis might not seem so radical if we recall that today’s prevailing mode of multiple manual-guided treatment protocols, each tailored to a different DSM diagnosis, is of relatively recent origin (
118). According to some commentators, disorder-specific psychotherapies arose after the 1980s as a result of the structure of DSM, which encouraged disorder-specific clinical trials. Before the 1980s, clinicians tended to apply a treatment approach derived from their own theoretical orientation to the etiology of psychopathology in general (e.g., psychodynamic, behavior modification). In this new century, the pendulum may be swinging back, in the form of transdiagnostic therapies, whose success could have been anticipated by
p.
Transdiagnostic therapies are gaining appeal for good pragmatic reasons: Treating a patient for each of his or her multiple disorders one after another in turn rapidly exhausts resources, including clinician time, health insurance, and the patient’s tolerance. But in view of emerging evidence on the structure of psychopathology and
p, a universal therapy makes theoretical as well as pragmatic sense (
62). Transdiagnostic treatment protocols are being tested with several notable successes (
62,
119). Some psychotherapies developed for one disorder have become transdiagnostic because they were subsequently found to be effective for several other disorders; an example is dialectical behavior therapy (
120,
121). Other psychotherapies have been deliberately designed to treat multiple related disorders; an example is the unified protocol for transdiagnostic treatment of emotional disorders (
122). Such treatments are able to help patients who have very different symptom pictures, because the protocols target emotion dysregulation and neuroticism, and they correct patients’ incorrect thoughts (
123), all of which are etiological factors of
p.
If a universal psychotherapy protocol is needed to reduce high levels of
p, how could this be achieved? One strategy is to identify and distill the therapeutic elements that are common across disorder-specific protocols, then cobble those elements that have proven efficacy into a single universal
p-therapeutic protocol (
124–
126). For example, a large number of cognitive-behavioral protocols for treating different disorders comprise the same evidence-based modules: psychoeducation, setting treatment goals, cognitive restructuring, behavioral activation, recognizing physiological responses, emotion regulation, problem solving, exposure, identifying triggers, relapse prevention, motivation enhancement, social skills training, and mindful emotion awareness (
62). These elements appear in protocols tailored to eating disorders, anxiety disorders, depression, personality disorders, substance abuse, PTSD, aggression, and psychoses, suggesting that they treat the constituents of
p, and possibly
p itself.
Our focus in this section has been on psychotherapies, but the same hypothesis that all disorders should respond to one treatment can also be extended to pharmacotherapies. Atypical antipsychotics and antidepressants could be considered “broad spectrum” because they work for multiple disorders (
118). For example, paroxetine (used for multiple disorders) has been shown to be therapeutic for personality trait neuroticism—an underpinning of
p—and greater improvement in neuroticism has been found to predict less subsequent major depression (
127). In addition to established pharmacotherapies, evidence that immune response is dysregulated in many psychiatric disorders—including depression, schizophrenia, and autism—has prompted the hypothesis that psychiatric diseases might respond to anti-inflammatory medications (
128). Whether or not anti-inflammatory therapies might turn out to be broad spectrum is unknown (
129).
We are aware that the hypothesis of an evidence-based universal psychotherapy or pharmacotherapy runs counter to the notion of personalized medicine. And yet personalized treatment for every patient is based on the idea that every patient’s disorder has its own specific etiology, whereas the science of
p raises serious questions about causal specificity among mental disorders. Nevertheless, uniform etiology does not guarantee uniform treatment response. Therefore, clinical research could evaluate the hypothesis that transdiagnostic psychotherapy and pharmacotherapy can be the first-line treatment in a staged, stepped-care system, in which patients who do not improve go forward to more specialized treatment. Transdiagnostic treatments may be ideal for individuals who present with a mixture of anxious distress, motivational problems, emotional dysregulation, and aberrant thinking (
130), all of which are part of
p.
The idea of p has special relevance for primary prevention. By definition, primary prevention cannot be indicated by a diagnosis, pointing to the need for transdiagnostic rather than disorder-specific prevention strategies. In addition, p implies that many different disorders share common risk factors, pointing to the need for prevention strategies that target malleable, nonspecific risk factors. Population-wide programs that reduce exposure to childhood adversities and that foster early-life brain health may offer the greatest promise of tackling risk factors for the development of p, such as maltreatment, intellectual impairment, neuroticism, emotion dysregulation, and disordered thought.
Conclusions
Mental disorders are pervasive in the population; they do not breed true across generations in families; they show little causal specificity; and they do not simply go away, instead often morphing with time into other, different conditions. Indeed, people who experience one condition often experience other co- and future-occurring conditions. These facts possibly reflect a quantitatively distributed, stable, generalized liability to develop any and all forms of psychopathology across the life course, which we called p. We have heard concerns that invoking p might encourage a pejorative attitude toward mental illness because p seems like an amorphous dimension, and not a diagnosed medical condition with a paired indicated treatment. Seen from this perspective, p could invite entre nous diagnoses such as FLK (“funny looking kid”) or “high serum porcelain.” However, p need not remain amorphous if it is aggressively researched, and here we put forward a research agenda. Noting that the Journal is commemorating its 175th year of publication, we suggest five possibilities for what can be done before its 200th.
First, we need more prospective longitudinal studies that model psychiatric data over the life course. The
p factor is a life-course concept—a general liability to manifest disorder that extends from childhood through adulthood—but most researchers are still approaching it cross-sectionally. Some questions that bedevil cross-sectional research could be reframed by longitudinal data. One example question arises from the fact that the bifactor model (see
Figure 2C) shows that there are independent factors that statistically influence a smaller subset of internalizing and externalizing symptoms in addition to
p. The question is, What is the substantive meaning of the residual parts of internalizing and externalizing that do not overlap with
p? One hypothesis is that they may appear to have meaning in cross-sectional analyses, when disorders are assessed at any one point in a life, but given the ubiquity of sequential comorbidity, they have less substantive meaning with repeated measurements taken over the course of a life, as people move in and out of disorder groups over time. In this way, the bifactor analogy of intelligence assessment breaks down. People do not change from having great verbal skills to having great spatial skills, but they do change from conduct disorder to depression to psychosis. Another example question is: If some individuals have a greater susceptibility to all symptoms of psychiatric disorders, why is this liability expressed as any particular disorder at specific ages? Hypotheses to be tested range from age-graded changes in the opportunity to express certain symptoms to age-graded neurobiological changes. A short-term snapshot view of an individual’s psychiatric symptoms may raise questions that are resolvable when the individual is viewed across the life course.
Second, p needs to be measured. At present, p is a statistical abstraction, a latent liability to develop multiple psychiatric problems that is estimated by analyzing data on multiple symptoms and disorders. To be useful in clinical and research settings, p needs to be rendered concrete by developing reliable and valid measures that capture an individual’s liability. We hypothesize that such a measurement tool will include the underpinnings of p, including neuroticism, emotional dysregulation, and disordered thought, as well as the assessment of intellectual impairments, developmental trauma history, and family psychiatric history. Other efforts to rethink classification in psychiatry (e.g., RDoC) are eschewing the existing diagnostic system and studying multiple constructs (e.g., cognitive control, fear, arousal) in hopes of achieving a new diagnostic system. In contrast, p has been abstracted from the existing diagnostic system (which, after all, describes the universe of psychopathology pretty well), and we now need new measures that will tap constructs that capture p. Seen in this light, the idea of p is not so radical. It does not call for an overthrow; it calls attention to the possibility that blurred diagnostic boundaries are not a problem but an opportunity.
Third, new discoveries need to be made in biological psychiatry, and p has the potential to enhance discovery. The hypothesis is that there is a factor that accounts for meaningful variance across all forms of psychopathology. If it can be measured, it can be used to identify the causes shared by psychiatric disorders. Using p as an outcome in biological psychiatry is a more expedient route to finding shared causation than comparing disorder pairs. We look forward to the use of p in genome-wide association studies and brain-wide mapping.
Fourth, when specificity is desirable, research designs could test for it, not assume it. If p is real, researchers might not expect to find single-disorder loyalty in causes (e.g., genes, maltreatment), biomarkers (e.g., neuroimaging findings, cognitive task performance, inflammation), consequences (e.g., suicide attempts, impaired relationships), or treatments (e.g., psychotherapy, pharmacotherapy). As a research example, if theory of mind—the ability to understand that others have perspectives that are different from one’s own—was thought to be the salient core deficit in autism, this could be demonstrated by testing for this deficit in other disorders too. Similarly, if a drug is meant to treat one disorder, the clinical trial should include an arm with other disorders as a counterfactual, to determine whether or not the drug has therapeutic specificity.
Fifth, p may encourage the willingness to develop and experiment with transdiagnostic treatments. The most radical hypothesis is that if all common psychiatric disorders share core risk factors, all disorders will respond to the same treatment(s). High on the research agenda is the need to develop and apply a measure of p as an outcome in clinical trials, including of first-line treatments that aim to delay or derail progression to diagnostic threshold, and of tertiary transdiagnostic treatments aimed at patients with already diagnosed disorders. Above all, p should be evaluated as an outcome testing interventions aimed at the primary prevention of mental illness.