Media coverage of catastrophic violence by people thought to have psychiatric disorders raises public alarm and stigmatizes patients. Much of the media coverage fails to acknowledge that serious violence by people diagnosed with mental illness is rare and that psychiatric patients are more often the victims of violence than the perpetrators. The alarmist quality of this reporting notwithstanding, mental health providers have a responsibility to reduce the risk of violence, to the extent that it is possible, through appropriate care. To do this, they need knowledge of the correlates of violence in the populations they treat.
Schizophrenia affects less than 1% of the population, yet it is the fourth leading cause of disability in developed countries among people ages 15–44 (
1). Only about 10% of people with schizophrenia will engage in violence during their lifetime (
2,
3); however, they are three to four times more likely to act violently compared with the general population, after adjustment for socioeconomic factors (
4). Risk factors for violence in the general population, such as youth, a history of childhood abuse, a history of substance use, and, in particular, a recent history of violence (
5–
7), also apply to people with schizophrenia (
2).
Research has not yet clarified whether and to what extent the symptoms and signs of schizophrenia, which often fluctuate in severity, are themselves risk factors for violent behavior (
8). Paranoid ideation has been linked to violence in community samples (
9), but delusions, including persecutory delusions, have not shown a consistent association (
10–
12). Positive symptoms of psychosis, which include hallucinations in addition to delusions (
13), were linked to serious violence in one cross-sectional analysis of data from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) study. Negative symptoms, which include blunting of affect and poverty of speech, were associated with less violence in these individuals (
14) but not in other cohorts (
15).
Why are these findings inconsistent? First, the correlates of violence appear to vary with its severity (
4), and research has not always focused on the types of violence that are of greatest concern. Second, research has not always included evidence of recent violent behavior, a recognized risk factor for violence, among independent variables (
13).Third, cross-sectional surveys examine risk factors and violence within the same time period, allowing the possibility that some correlates of violent behavior, such as psychotic symptoms, occur after the violent act. Despite their cross-sectional association, for example, positive symptoms have not been found to predict violence in schizophrenia over the subsequent 6-month period (
13).
In this study, we sought to identify correlates of violence in schizophrenia. To enable us to address questions unanswered by previous research, we 1) used an outcome that is of particular concern to clinicians and the public, namely, violence that caused injury to others; 2) employed as an independent variable a description of each participant’s recent violent behavior corresponding to information available to any assessing clinician in real-world practice; 3) examined separately the predictors of violence in participants who did not describe injurious violence at baseline; and 4) examined correlates of violence only prospectively so that any correlate identified had to have been present before the act.
Methods
Sample and Data
The CATIE schizophrenia trial was a randomized double-blind effectiveness trial of antipsychotic medication conducted at 57 U.S. sites and funded by the National Institute of Mental Health. Data from one site were removed because of quality concerns. The study was approved by the institutional review board at each site. Written informed consent was obtained from the patients or their legal guardians.
The trial collected data on more than 1,400 patients with schizophrenia who were initially considered by their clinicians to need a change in their antipsychotic medication. Assessments of the participants’ clinical condition and violent behavior were conducted at baseline and thereafter every 6 months to a maximum of 18 months. Full details of the study, including the measures used and methods of data collection, have been published elsewhere (
16–
18).
Measures
Dependent variable (violent behavior).
Data on violent behavior were gathered using the 19-item MacArthur Community Violence Interview (
13), which assesses the past 6 months. Interview items include questions such as “Have you pushed, grabbed or shoved anyone?”; “Have you kicked, bitten, or choked anyone?”; “Have you tried to force anyone to have sex against their will?”; and “Have you used a knife or fired a gun at anyone?” A positive response to an item triggers a supplementary question about injury: “Was anyone hurt?” A final summary question further asks, “Did you physically hurt or injure anyone?”
We created a dichotomous outcome measure comprising a report of any injurious violence indicated by a positive response to any of the supplementary injury questions or a positive response to the final summary question that asked whether anyone was physically hurt or injured. We generated a second outcome measure reflecting noninjurious violence in which neither any of the supplementary questions nor the final overall injury question was answered in the positive. The third outcome, no violence, comprised negative responses to all items. The assessment of violent behavior was conducted at the time of study entry and at 6, 12, and 18 months.
Independent variables (risk factors).
The independent variables were chosen to include correlates of violence identified in previous studies of patients with schizophrenia. With the exception of medication adherence, which was rated from multiple sources (clinical records, patient self-report, and pill counts by independent research assistants), independent variables were based on either self-report or the results of using standardized instruments with established reliability and administered by independent trained raters. When more than one measure of a risk factor with acceptable psychometric qualities was available, as was the case for current substance abuse, we selected the measure that was most practical for use by evaluating clinicians.
The independent variables are summarized in
Table 1. Race was self-defined by participants. Vocational activity was rated as present if the participant was regularly engaged in either competitive or supported employment. “Married” included nonmarried cohabitation. Monthly income was dichotomized and rated “yes” if it was above the median for the cohort. Economic scarcity was rated as present if the participant reported having insufficient funds to pay for any one of the following essentials over the past 6 months at any point: food, clothing, housing, or essential travel.
Childhood sexual abuse was rated from the answer to the question, “Before the age of 15, were you ever sexually molested or assaulted?” Feeling listened to was rated from the response to the question, “When you are talking with your family and friends, do you feel you are being listened to most of the time, some of the time, or hardly ever?” Violent victimization over the past 6 months was rated by using the response to the question, “In the past 6 months, were you a victim of any violent crime such as assault, rape, mugging, or robbery?”
Positive and negative symptoms of schizophrenia were measured with subscales of the Positive and Negative Syndrome Scale (PANSS) (
19). Depressive symptoms were measured by using a participant’s mean item score on the Calgary Depression Scale for Schizophrenia (
20). Substance use was measured first with clinicians’ ratings of whether criteria were met for a diagnosis of abuse or dependence and second with clinicians’ ratings of the severity of current use on the 5-point Dartmouth scale (
21). This scale focuses on persistent and recurrent social, occupational, psychological, and physical problems stemming from substance use.
Years in treatment refers to treatment with antipsychotic medication. Medication adherence was rated for the first month of treatment, applying a 4-point scale. Supervised accommodation was indicated by self-report data indicating that a participant lived in a supervised apartment, a hospital, or a nursing home. Adaptive function was measured with two instruments: the Quality of Life Scale (
22), which focuses on the deficits associated with chronic schizophrenia, and the Instrumental Activities of Daily Living Scale (
23), which assesses various functions, including personal care and housekeeping. Satisfaction with life was rated with a 7-point scale from the response to the question, “How do you feel about your life in general?” (
24).
Statistical Analyses
We examined data on 1,435 participants for whom both baseline and follow-up information on violence was available. The statistical approach was selected in part to address attrition in the course of the CATIE study (
14). The analyses used a proportional hazards model of time to first injurious violence, generating bivariable and multivariable hazard ratios associated with the baseline predictors (independent variables). We then conducted the same analyses for participants who did not report engaging in injurious violence at baseline. We censored participants who discontinued their participation at the point where no further follow-up data were available.
Results
Participants’ basic demographic and clinical characteristics and rates of injurious and noninjurious violence over the 18-month follow-up period are summarized in
Table 1; detailed demographic and behavioral characteristics have been published elsewhere (
13,
14). All participants met or had met DSM-IV diagnostic criteria for schizophrenia. Their illnesses were long-standing and relatively unstable. At baseline, the mean time since the first treatment with antipsychotic medication was 16.5 years (SD=10.9). Only 13.1% of participants were engaged in vocational activity, as defined here to include supported employment, and 43.1% lived in supported accommodation.
The participants’ mean age was 40.5 years (SD=11.1); 74.2% were male, 60.4% were Caucasian, and 20.6% were married or cohabiting. The mean number of years in education was 12.1 (SD=2.23), which is consistent with previous reports on this sample showing that 25% had less than a high school education and 39% attended college (
13). Victimization was common. Approximately 20.2% of the sample reported a history of sexual victimization before the age of 15, and at study entry, 2.4% reported being the victim of a crime such as assault, rape, mugging, or robbery in the past 6 months.
Altogether, 37.8% of participants met criteria for substance abuse or dependence in addition to their diagnosis of schizophrenia. At study entry, participants were moderately symptomatic; 16.3% had been admitted to the hospital more than twice in the past 12 months. The mean positive symptom score on the PANSS was 18.4 (SD=5.61) (possible range, 7–49), and the mean negative symptom score was 20.1 (SD=6.40) (possible range, 7–49). The mean item score on the Calgary Depression Scale for Schizophrenia was 1.57 (SD=0.55) (possible range, 1–4).
At study entry, 85 participants (5.9%) reported having inflicted injurious violence in the past 6 months, and 135 (9.4%) reported having engaged only in noninjurious violence. During the 18-month follow-up period, 77 participants (5.4%) reported having engaged in injurious violence, and 119 (8.3%) reported having engaged only in noninjurious violence.
Employing a proportional hazards model of baseline predictors to the time of first injurious violence and using a p value of 0.01 as a threshold for significance because of the large number of variables evaluated, the following baseline measures were associated with future injurious violence in the bivariable analysis (
Table 2): baseline injurious violence (hazard ratio=7.29) and baseline noninjurious violence (hazard ratio=3.94); childhood physical abuse (hazard ratio=1.92), sexual abuse (hazard ratio=2.58), and conduct problems (hazard ratio=1.89); not feeling listened to by one’s family (hazard ratio=1.54) and having been violently victimized in the past 6 months (hazard ratio=5.79); positive symptoms of psychosis (hazard ratio=1.06) and depressive symptoms (hazard ratio=1.77); severity of current drug (hazard ratio=1.84) and alcohol (hazard ratio=1.53) use and current medication nonadherence (hazard ratio=1.46); and having been arrested for a crime in the past 6 months (hazard ratio=1.92).
For all participants, baseline injurious violence (hazard ratio=4.02), recent violent victimization (hazard ratio=3.52), severity of drug use (hazard ratio=2.93), baseline noninjurious violence (hazard ratio=2.72), childhood sexual abuse (hazard ratio=1.85), and medication nonadherence (hazard ratio=1.39) remained significantly associated with future injurious violence in the multivariable analysis (
Table 3).
When the analysis was limited to patients with no history of engaging in injurious violence at baseline, every significant bivariable correlate, with the exception of a diagnosis of substance abuse or dependence, was also a significant predictor in the analysis of all participants (
Table 2). In the multivariable analysis (
Table 3), baseline noninjurious violence (hazard ratio=3.02) and only three additional variables—childhood sexual abuse (hazard ratio=2.13), severity of drug use (hazard ratio=1.63), and medication nonadherence (hazard ratio=1.48)—remained significantly associated with injurious violence.
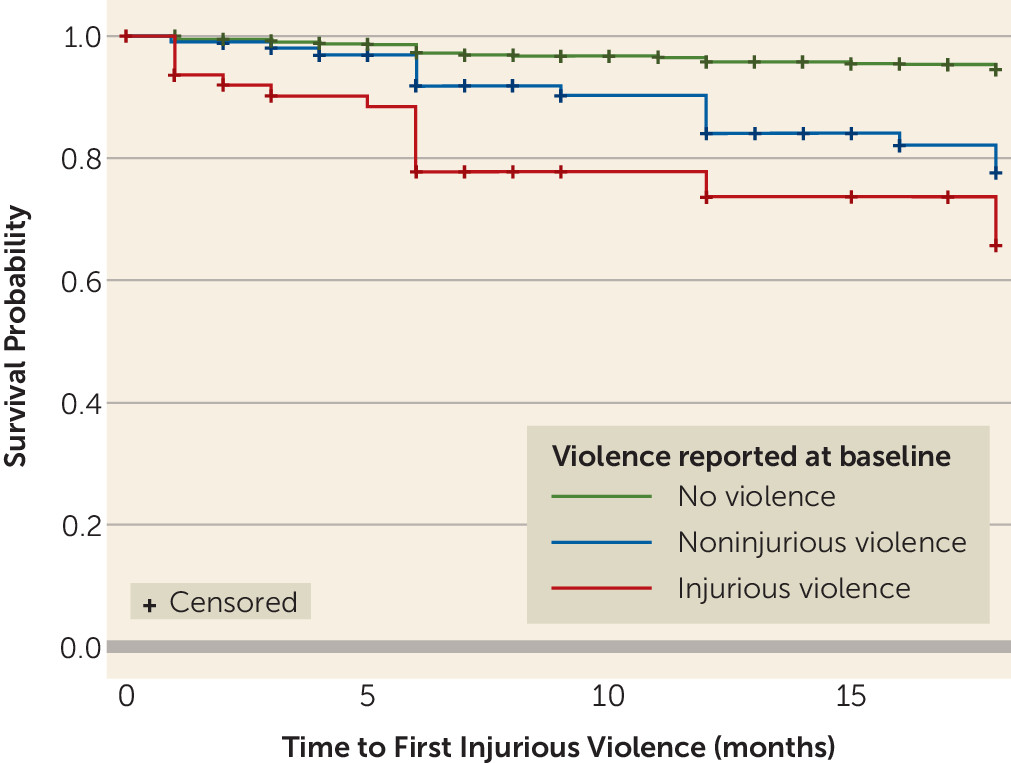
Survival analysis of time to first injurious violence (
Figure 1) confirmed that participants with injurious violence at baseline had by far the highest rates of future injurious violence, followed by individuals with noninjurious violence at baseline. For all groups, violence continued at a constant rate throughout the follow-up period.
Discussion
Previous studies of violence in this sample have either focused on medication effects (
14) or examined all correlates of violence, not just those that preceded a violent act, where a stronger case can be made that the correlate was directly or indirectly causal (
13). This study is therefore the first, to our knowledge, to describe the correlates of subsequent injurious violence among patients being treated for schizophrenia in which the independent variables included recent violence toward others. Independent and dependent variables were rated by trained raters using reliable instruments.
These methodological differences generate results that are significantly different from those generated by other studies. In the multivariable analysis, a history of engaging in injurious violence in the 6 months before baseline evaluation and recent violent victimization were the most powerful predictors of subsequent injurious violence, with hazard ratios >3.5. The few additional significant predictors in the multivariable analysis were severity of drug use, baseline noninjurious violence, childhood sexual abuse, and medication nonadherence.
For participants with no history of engaging in injurious violence at baseline, baseline noninjurious violence was the strongest predictor in the multivariable analysis, followed by childhood sexual abuse, severity of drug use, and medication nonadherence.
Comparison With Other Studies: Rates of Violence
The overall rate of violence in schizophrenia reported here is comparable to that reported elsewhere (
2), but the rate of serious violence is higher. The 6-month prevalence of injurious violence at baseline was 5.9% in our study, compared with a 6-month prevalence of serious violence at baseline of 3.6% in an earlier analysis of the same participants (
13). The most likely explanation lies in the broader definition of the dependent variable used in our study. Previous research on these participants used a definition of serious violence that was limited to positive responses to two items on the MacArthur Community Violence Interview: “Have you used a knife or fired a gun at anyone?” and “Did you physically hurt or injure anyone?”
Rates of violence declined after baseline assessment. The 5.4% rate of injurious violence for the subsequent 18 months, for example, was lower than the rates of injurious violence for the 6 months before study entry. Three factors are likely to have contributed. First, patients were enrolled in the CATIE study because their treatment was considered suboptimal (
13). If one reason for this was recent violence, one would expect a decline in the rate as a result of regression to the mean. Second, treatment during the trial was associated with reduced symptoms on multiple measures (
18) and may have reduced violence. Third, 54% of participants had stopped providing data by month 18 (
25). Nonadherence to treatment is a correlate of violence in psychosis (
15). Participants who engaged in violence may have been more likely to drop out of the study.
Comparison With Other Studies: Correlates of Violence
Simultaneous large effects, in multivariable longitudinal analysis, of baseline injurious violence and recent victimization have not been shown previously in patients with schizophrenia. Previous studies suggest a shared relationship, as antecedents of violent behavior, between experiencing and perpetrating harm (
15). Victimization ceases to be a correlate of violence when baseline injurious violence is removed from the analysis. Further research is required to establish whether people with schizophrenia who both experience and perpetrate injurious violence do so during the same incidents. The remaining findings in the present multivariable analysis are less new. Both childhood sexual abuse and substance abuse have been replicated risk factors for violence (
4).
The 85 participants who described recent injurious violence at baseline comprised only 5.9% of the study sample but 23% of all participants with injurious violence at follow-up. We anticipated that individuals who acted violently only during the follow-up period would differ from the study sample as a whole in terms of the antecedent predictors of violence. Contrary to our expectations, removing the hazard ratio associated with injurious violence for the whole sample was not associated with compensatory increases in the hazard ratios for other risk factors (and the hazard ratio for severity of drug use decreased). The corollary would seem to be that predicting injurious violence will be even more difficult for the group without violence at baseline, because the most helpful hazard ratio for the purposes of prediction is lacking.
Of the significant associations we observed in the bivariable analysis, childhood conduct problems have previously been linked to general criminality or less serious violence in this study sample (
14) as well as in other samples, albeit inconsistently (
26,
27). Depression, too, has previously been linked to violence in this (
14) and other samples (
2). Antidepressants now appear to be of limited efficacy in treating depression in schizophrenia (
28). Alternative forms of treatment, in addition to helping improve patients’ mood, may reduce rates of violence.
Previous longitudinal studies found negative symptoms of schizophrenia to be negatively correlated with violence (
14). We found no association between negative symptoms and injurious violence in bivariable or multivariable analysis. Previous cross-sectional research has also linked positive symptoms to violence (
13), but again, we found no correlation. Cross-sectional methods allow the possibility that symptoms follow, rather than precede, violence, and the absence of a significant association using a prospective method suggests that symptoms such as delusions are sometimes a consequence, rather than a cause, of violence. One possibility is that such symptoms reflect clinical deterioration under the stress of police and legal involvement.
Implications for Risk Assessment and Management
The hazard ratios associated with baseline violence and recent victimization represent large effects by conventional criteria (
29) and are larger than those reported for psychosis as a whole (
15). The association with treatment adherence, while smaller in hazard ratio terms, persists in multivariable analysis and speaks to the important contribution of maintaining a therapeutic alliance in the management of violence risk.
Neither of these points, however, should distract from the overall picture of violence in schizophrenia. Nineteen out of every 20 participants in this unstable sample described no violence of any kind during the follow-up period. Even among the 85 individuals with baseline injurious violence, most did not report any violence during follow-up. While these results have implications for our understanding of the causes of violence in schizophrenia, they do not suggest that violence risk could be more successfully managed by identifying individuals who will act violently and by admitting them to the hospital. These results do not challenge previous suggestions that if this approach were to be attempted, false positive rates, false negative rates, or both would be unacceptably high (
30,
31).
Limitations
There are several limitations to this study. First, we relied on self-reported data to identify violent acts. Although self-report, used prospectively, is a more sensitive measure of violence than official reports and is similar in sensitivity to using multiple sources of information simultaneously (
32), information from collateral sources might have added validity to the dependent variable. Second, the maximum period of follow-up was 18 months. Clinicians are frequently concerned with shorter-term risk. Although not shown empirically, it is possible that the same risk factors act differently at different times and that our findings would have been somewhat different had we restricted follow-up to, say, 6 months. Larger numbers would be required to explore this possibility.
Third, although the dependent variable, violence, was measured throughout the follow-up period, the independent variables were measured only at baseline. Some of these variables would likely have changed during the follow-up period. Some people would have found independent accommodation and some would have found work. Clinical changes, and in particular reductions in posttraumatic stress disorder symptoms and substance use, have been shown to be associated with reductions in violence in other patient groups (
33,
34). We did not investigate the correlates of these changes in this sample.
Finally, our 6 monthly follow-up, while shorter than those used in many studies of mental disorder and violence, may have been too long to detect some effects. The absence of an association between positive symptoms, including delusions, and engaging in injurious violence over the ensuing 6 months, for example, is an important finding for the purposes of assessing risk. It could still be the case, however, that in some circumstances delusions cause violence and that the effect is too transitory to be detected using this design. Correlations between delusions and violence that are found only in cross-sectional studies could be the result of mental state changes that follow violence, as suggested here, but could also be caused by short-term effects.