Numerous studies indicate that transgender individuals—that is, individuals who experience incongruity between their sex assigned at birth and their current gender identity—are at particular risk of psychological distress and associated impairment (e.g., suicidality) (
1–
3). This elevated risk is hypothesized to stem at least in part from transgender individuals’ elevated exposure to stigma-related stress, also known as minority stress (
4,
5), and it can also result from the stress associated with a lack of gender affirmation (i.e., the accurate recognition and validation of one’s gender identity) (
6). ICD-11 (
7) specifies that individuals experiencing persistent discordance between their experienced gender and their assigned sex meet diagnostic criteria for gender incongruence.
To alleviate the stress of persistent discordance between experienced gender and assigned sex, an increasing number of transgender individuals who experience gender incongruence seek gender-affirming medical interventions, including hormone replacement therapy and gender-affirming surgeries (
8). The World Professional Association for Transgender Health’s
Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People recommends consideration of these interventions for affirming transgender individuals’ gender and alleviating gender-related stress (
9).
Despite professional recommendations to consider gender-affirming medical interventions for transgender individuals who experience gender incongruence, the effect of such interventions on long-term mental health is largely unknown. Available evidence stems mainly from small samples utilizing cross-sectional designs and self-reported treatment exposures and mental health outcomes (
2,
10,
11). A meta-analysis that aggregated data across nearly two dozen small-sample studies (
10), mostly relying on cross-sectional designs, found positive associations between self-reports of receiving both hormone therapy and gender-affirming surgery and mental health. Several more recent uncontrolled studies of the effects of hormone replacement therapy on transgender individuals’ mental health have found that transgender individuals’ mental health improved for up to 24 months after initiating hormone therapy (
11,
12).
The limitations of previous research in terms of nonrepresentative sampling, self-reported measurement, and limited follow-up periods can be overcome with national health registry data sets that include clinician-derived assessment of gender incongruence and complete records of psychiatric and gender-affirming treatment and utilization data in an entire population. In the one known study to use a population-based design to investigate psychiatric morbidity among transgender individuals (N=324), individuals who had legally changed their gender and had a diagnosis of gender incongruence associated with an inpatient hospital visit in Sweden between 1973 and 2003 were at higher risk of suicide attempts, suicide-related mortality, and psychiatric hospitalization compared with age- and reassigned-gender-matched controls (
13). The study did not report the prevalence of mood and anxiety disorder treatment among those receiving gender-affirming treatment compared with the total population or as a function of length of time since receiving gender-affirming treatment. Furthermore, the proportion of individuals receiving gender-affirming treatments in Sweden has increased nearly exponentially since 2003 (
8,
14). Similar recent increases in referrals for gender-affirming treatments have been reported in other countries around the world (
15–
18).
In this study, we took advantage of the Swedish Total Population Register (
19), linked to the Swedish National Patient Register and the Swedish Prescribed Drug Register, to ascertain the prevalence of mood and anxiety disorder health care visits, antidepressant and anxiolytic prescriptions, and hospitalization after a suicide attempt among the entire Swedish population as a function of gender incongruence diagnosis, gender-affirming hormone and surgery utilization, and length of time since receiving gender-affirming treatments. This data set permitted identification of all individuals in Sweden seeking gender-affirming treatments between January 1, 2005, and December 31, 2015. Although not all transgender individuals seek gender-affirming treatments and not all treatment-seeking transgender individuals meet diagnostic criteria for gender incongruence, findings from this unique data opportunity have timely implications for documenting the mental health of transgender individuals seeking gender-affirmative treatment and ways in which the medical profession can support this increasingly visible population.
Methods
This total population prospective study included all individuals living in Sweden on December 31, 2014, as identified in the Swedish Total Population Register. Using de-identified personal identification numbers (a unique number assigned to all Swedish residents), we linked sociodemographic information with National Patient Register information on health care usage between January 1, 2005, and December 31, 2015, and Prescribed Drug Register information on prescribed and purchased medication between July 1, 2005, and December 31, 2015. The study was approved by the Regional Ethics Committee in Stockholm (no. 2017/1736–31).
Gender Incongruence Diagnosis
Using the Swedish National Patient Register, we classified all individuals in Sweden according to whether they had received a diagnosis of gender incongruence, as defined by the diagnostic system applied in Sweden during the study period (i.e., a diagnosis of either transsexualism [ICD-10 code F64.0] or gender identity disorder [ICD-10 codes F64.8, F64.9]) during an inpatient or specialized outpatient visit between January 1, 2005, and December 31, 2015. The two diagnoses used to define gender incongruence at the time of the study are not fully equivalent but capture largely overlapping populations (
20). In Sweden during the study period, a diagnosis of either transsexualism or gender identity disorder was required for accessing gender-affirming treatment (e.g., gender-affirming hormone treatment, hormone-suppressing or -blocking medication treatment, mastectomy with chest contouring, hair removal, vocal cord surgery, speech therapy, genital surgery) and was given after an approximately yearlong evaluation, following a national consensus program (
14,
21). Adolescents could receive the same gender-affirming treatments as adults but could not receive genital surgery before age 18 (
22).
Outcome Measures
This study’s outcome measures were psychiatric outpatient health care visits, antidepressant and anxiolytic prescriptions, and hospitalization after a suicide attempt between January 1, 2015, and December 31, 2015. Restricting the outcome assessment period to one year, 2015, the most recent available, removes potential confounding by secular trends in treatment utilization and transgender acceptance and visibility. Each psychiatric outpatient visit was coded by the treating physician with a primary diagnosis from ICD-10 (
23) and up to 20 supplementary ICD-10 diagnostic codes. Using these codes, we classified all individuals as having received treatment for any or no mood disorders (codes F30–F39) or anxiety disorders (codes F40–F42). Prescribed medication use was obtained from the Swedish Prescribed Drug Register, which contains information regarding all prescribed and purchased medications nationwide for all individuals. Individuals were categorized into any use or no use of antidepressant and anxiolytic medication according to the Anatomical Therapeutic Chemical (ATC) Classification system (codes N06A and N05B). All inpatient health care visits were similarly coded by the treating physician using ICD-10, indicating a primary cause of hospitalization and up to 30 supplementary causes. Using these codes, we classified all individuals as having been hospitalized after a suicide attempt (versus not) using the ICD-10 codes for intentional self-harm (codes X60–X84).
Covariates
Sociodemographic information was drawn from the Swedish Total Population Register in December 2014 and included current legal gender, age, country of birth, level of education, urbanicity, and household income.
Gender-Affirming Treatment Utilization
For individuals with a gender incongruence diagnosis at any visit, we assessed the type and year of gender-affirming treatment, both hormone treatment and surgery. Information about hormone treatment, including androgen-suppressing and -blocking medication, was obtained from the Swedish Prescribed Drug Register between July 1, 2005, and December 31, 2015. All medications prescribed to individuals who had received a gender incongruence diagnosis were coded as gender-affirming if they were feminizing hormone medication (i.e., estrogens [ATC codes G03C, L02AA], progestogen [G03D]), masculinizing hormone medication (i.e., androgens [G03B]), or androgen-suppression or -blocking medication (i.e., testosterone-5-alpha reductase inhibitors [G04CB], antiandrogens [G03H], gonadotropin-releasing hormone analogues [G03GA, L02AE, H01CA], antigonadotropin-releasing hormones [H01CC], and spironolactone [C03DA01]). For each individual with a gender incongruence diagnosis who received prescriptions for any of these medications, we calculated the number of years since initiation.
Gender-affirming surgery was coded using information about all inpatient surgical procedures received by individuals with a gender incongruence diagnosis in the National Patient Register between January 1, 2005, and December 31, 2015. All surgical procedures associated with a gender incongruence diagnosis performed during this period were coded by type of surgery using the Nordic Medico-Statistical Committee Classification of Surgical Procedures (
16): breast or dermatological chest surgery (codes H and QB), surgery of the reproductive organs (codes K and L), dermatological surgery (code Q), and laryngeal surgery (code DQ).
Statistical Analysis
We first examined sociodemographic differences between individuals with a gender incongruence diagnosis and the rest of the population in Sweden. We then compared the prevalence of any mood and anxiety disorder treatments (i.e., psychiatric outpatient health care visits and prescribed psychiatric medication) between individuals receiving gender-affirming treatments and the rest of the population in Sweden during 2015, using logistic regression. Among individuals with a gender incongruence diagnosis, we then investigated the odds of mood and anxiety disorder treatment and hospitalization following a suicide attempt (occurring in 2015) as a function of years since initiation of hormone or hormone-suppressing treatment and since last gender-affirming surgery. We examined years since last gender-affirming surgery because gender-affirming surgery is often a lengthy process involving several distinct procedures before gender affirmation is attained.
All analyses were conducted using SPSS, version 24 (IBM, Armonk, N.Y.), and adjusted for current legal gender, age, country of birth, level of education, urbanicity, and household income.
Results
Of the total Swedish population on December 31, 2014 (N=9,747,324), 2,679 had received a diagnosis of gender incongruence between January 1, 2005, and December 31, 2015 (
Table 1). Those diagnosed with gender incongruence were significantly younger on average than the rest of the population (t=19.94, p<0.001), and they were more likely to have a current legal female gender than male gender (χ
2=4.54, p=0.03). Individuals with a gender incongruence diagnosis were more likely to have a university education (χ
2=12.77, p<0.001), to have a lower household income (t=30.61, p<0.001), to live in a larger city (χ
2=61.95, p<0.001), and to have been born outside of Europe (χ
2=32.33, p<0.001).
Mood and Anxiety Disorder Treatment Among Individuals Diagnosed With Gender Incongruence
Table 2 compares the prevalence of health care visits and medication treatment for mood and anxiety disorders between individuals diagnosed with gender incongruence and those not. In analyses adjusted for sociodemographic factors, those diagnosed with gender incongruence were about six times as likely to have had a health care visit due to a mood or anxiety disorder in 2015, more than three times as likely to have received prescriptions for antidepressant and anxiolytic medication in 2015, and more than six times as likely to have been hospitalized after a suicide attempt.
Gender-Affirming Treatments Among Individuals Diagnosed With Gender Incongruence
Just over 70% of individuals diagnosed with gender incongruence during the follow-up period (2005–2015) had received prescriptions for hormone treatment, including androgen-suppressing and -blocking medication, during this period. Half of those treated with hormones had initiated their hormone treatment within the past 5 years (
Table 3).
Nearly 40% of those with a diagnosis of gender incongruence had received gender-affirming surgical treatments during the follow-up period.
Table 3 presents the types of surgical treatments and the distribution of individuals by number of years since last gender-affirming surgery. The most common types of surgical procedures were mastectomy with chest contouring, surgery of the reproductive organs, dermatological surgeries, and laryngeal surgery.
Less than a third (29%) of those diagnosed with gender incongruence had received neither hormone treatment nor gender-affirming surgery. Among those who had received gender-affirming surgery, 97% had also been treated with hormones.
Changes in Likelihood of Mood and Anxiety Disorder Treatment After Gender-Affirming Hormone and Surgical Treatment
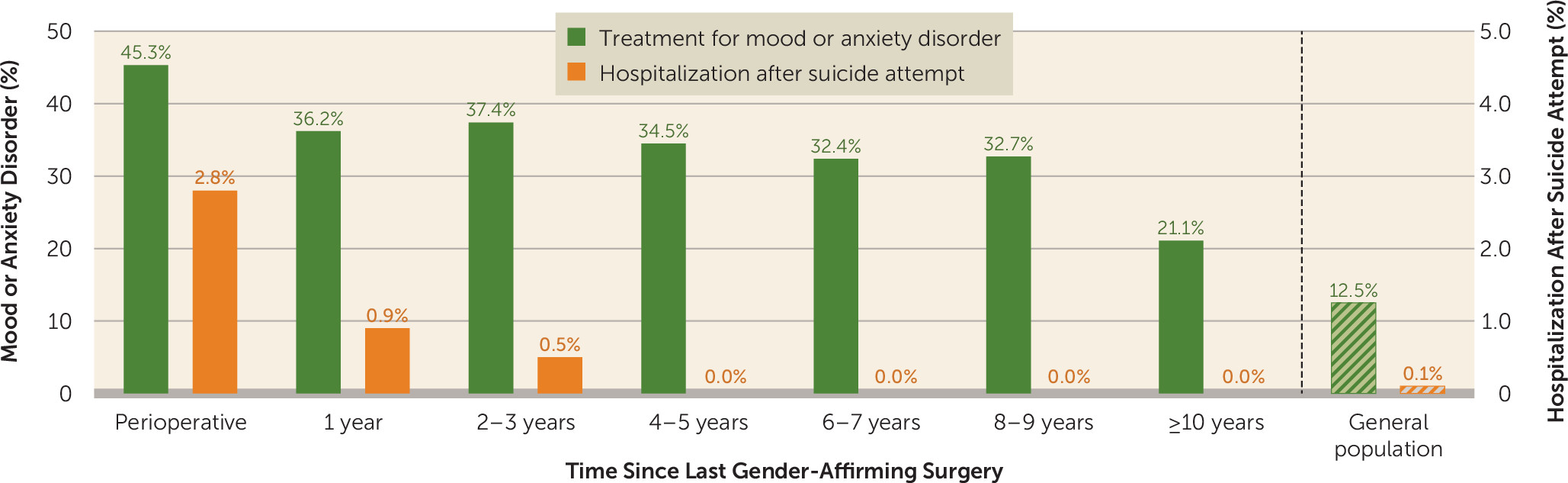
We examined the effect of years since hormone treatment initiation and years since last gender-affirming surgery on likelihood of having received mood or anxiety disorder treatment in 2015 among individuals with a diagnosis of gender incongruence. Among those with a gender incongruence diagnosis receiving hormone treatment, years since initiation of hormone treatment was not significantly related to likelihood of mental health treatment (i.e., psychiatric outpatient health care visits and prescribed psychiatric medication; adjusted odds ratio=1.01, 95% CI=0.98, 1.03). However, among those receiving gender-affirming surgical treatment, the risk of mental health treatment was significantly reduced with increased time since last surgical treatment (adjusted odds ratio=0.92, 95% CI=0.87, 0.97). Specifically, the likelihood of being treated for a mood or anxiety disorder was reduced by 8% for each year since last gender-affirming surgery. The number of individuals with a gender incongruence diagnosis who had been hospitalized after a suicide attempt in 2015 was low (N=22) but was also reduced as a function of time since last surgical treatment. The association between time since gender-affirming hormone and surgical treatments and hospitalization after a suicide attempt did not reach significance (hormone treatment: adjusted odds ratio=1.12, 95% CI=0.97, 1.30; surgical treatment: adjusted odds ratio=0.87, 95% CI=0.61, 1.24).
Figure 1 presents the prevalence of mental health treatment (either health care visits for depression and anxiety, antidepressant and anxiolytic prescriptions, or both) and hospitalization after a suicide attempt in 2015 by years since last gender-affirming surgical treatment.
To assess the potentially interrelated and therefore confounding effect of gender-affirming hormone and surgical treatments on each other, a sensitivity analyses was conducted, entering both years since initiation of hormone treatment and years since last surgical treatment simultaneously into the same model predicting odds of mood and anxiety disorder treatment (i.e., psychiatric outpatient health care visits and prescribed psychiatric medication). The results of this analysis were similar to those presented above, with a nonsignificant effect of time since initiation of hormone treatment (adjusted odds ratio=1.03, 95% CI=0.97, 1.08) and a significant effect of years since last gender-affirming surgical treatment (adjusted odds ratio=0.91, 95% CI=0.86, 0.97).
Discussion
Taking advantage of total population registers containing diagnoses of gender incongruence, gender-related hormone and surgical treatment codes, and mental health treatment utilization, we examined the potential impact of gender-affirming hormone and surgical treatment on later mental health treatment utilization. The results also present the first known population prevalence of mood and anxiety disorder treatment and suicide attempts among transgender individuals compared with the general population. Overall, our results show that transgender individuals, here defined as those with a diagnosis of gender incongruence, are about six times as likely as the general population to have had a health care visit for any mood or anxiety disorder, between three and four times as likely to have received prescriptions for antidepressant or anxiolytic medication, and more than six times as likely to have been hospitalized after a suicide attempt. Time since initiating gender-affirming hormone treatment was not associated with these mental health treatment outcomes, whereas time since receiving gender-affirming surgery was significantly associated with a decrease in mental health treatment.
These findings begin to answer the call for population-based documentation of transgender health (
1) and extend earlier evidence of associations between gender-affirming treatment and improved mental health mostly derived from studies utilizing cross-sectional designs or short follow-up periods, self-reported exposures and outcomes, and small nonprobability samples (
2,
10,
11). In addition to showing that transgender individuals are more likely to utilize mental health treatments than the general population, the results suggest that gender-affirming treatments may reduce this risk. Specifically, the odds of receiving mental health treatment in 2015 were reduced by 8% for every year since receiving gender-affirming surgery over the 10-year follow-up period. Despite this linear decrease, even 10 years after receiving such treatments, the prevalence of mental health treatment utilization continued to exceed that of the general Swedish population (
24), suggesting the need to address factors in addition to gender-affirming treatment availability that may strengthen transgender individuals’ mental health. Such factors may include reductions in structural (e.g., economic inequality), interpersonal (e.g., victimization), and psychosocial (e.g., identity concealment) stressors to which transgender individuals are disproportionately exposed (
4,
24). Ensuring access to transgender-affirming mental health care may also further reduce transgender individuals’ persistent psychiatric risk (
25). Although the prevalence of hospitalization after suicide attempt among those with a gender incongruence diagnosis was too small for statistical testing, the numbers who were treated after a suicide attempt decreased as a function of years since last gender-affirming surgery. Among those who received their last gender-affirming surgery more than 3 years ago, no suicide attempts were registered.
Despite the notable methodological strengths of utilizing data from a total population, the results should be interpreted in light of several limitations. First, the criterion used here to define the transgender population does not capture the full spectrum of those who identify as transgender. We specifically lacked information regarding gender assigned at birth, legal gender change, and gender identity at the time of data collection, preventing subgroup analyses of the transgender population (
26). Recent estimates across five countries suggest that between 0.4% and 1.3% of the population may identify as transgender, including gender-nonconforming individuals who do not seek gender-affirming hormone or surgical treatment (
18,
27–
29). Although the transgender population in the present study is limited to individuals with a diagnosis of gender incongruence, this population is of particular concern to the medical community because of its high likelihood of seeking gender-affirming hormone and surgical treatments. Given the free availability of gender-affirming treatments in Sweden, our approach to ascertaining this particular population is likely highly sensitive. Our approach also did not include a comparison group of individuals who had sought but not yet received gender-affirming treatment. While this population might be able to serve as an important comparison group in future studies, without the ability to distinguish between those who had not received treatment because they are waiting for it and those not seeking it in the first place, the current data structure cannot provide this comparison. Longitudinal designs assessing within-person changes in treatment seeking, treatment receipt, and ultimate mental health outcomes would be essential for tracking mental health before and immediately after treatment. Because our approach could only ascertain suicide attempts among living individuals, longitudinal designs that allow for tracking completed suicide among decedents remains an important future direction.
Second, mental health treatment utilization is an imperfect proxy for mental health itself. Transgender people receiving treatment for gender incongruence are by definition exposed to treatment settings, which may disproportionately expose them to mental health treatment opportunities. Although the Swedish context of universal health care coverage removes financial barriers to treatment seeking, other unmeasured factors, such as general tendency toward treatment seeking or perceived discrimination in treatment settings, may influence the associations examined here. Third, because we derived information about outpatient psychiatric health care visits from national health care databases, we had limited information about the type of mental health treatment patients received, and we could not differentiate among individuals receiving psychotropic medication, psychotherapy, or both. Fourth, this study was conducted in a single high-income national context with legal protections for transgender individuals and universal health coverage, including for gender-affirming treatments. While this context makes the present study possible, it also may constrain the generalizability of findings to low- and middle-income countries and to countries that lack transgender protections or universal health care coverage.
Overall, this study provides timely support for policies that ensure coverage of gender-affirming treatments. Although gender-affirming treatments are recommended as a medical necessity for appropriately selected individuals experiencing gender incongruence and are a covered health benefit in most developed countries, uncertainty exists, such as in the United States, regarding federal protections of transgender employees from transgender-related exclusions in employee benefits (
30). In the context of such uncertainty, some U.S. states deny use of state funds to cover costs for gender-affirming treatments, and the Veterans Health Administration specifically prohibits gender-affirming surgery within Veterans Affairs (VA) facilities or use of VA funding for gender-affirming treatments (
31,
32). To the extent that gender-affirmative medical interventions are interpreted as sterilization, many hospitals can refuse to provide such care, citing religious directives (
33). Debates regarding the provision of gender-affirming health care are global, and in much of the world, such care is unavailable or largely unaffordable (
29). Therefore, in many contexts around the world, lack of coverage for gender-affirming treatments drives the use of non–medically supervised hormones and surgeries, thereby exacerbating physical health risks (
34) and the other epidemics disproportionately borne by the global transgender population, including suicide and HIV infection. The longitudinal association found in the present study between gender-affirming surgery and reduced mental health treatment utilization, combined with the physical and mental health risks of surgery denial, supports policies that provide gender-affirming surgeries to transgender individuals who seek such treatments.