Duration of untreated psychosis (DUP)—the amount of time that elapses between psychosis onset and treatment initiation—predicts illness course in schizophrenia. DUP predicts likelihood and extent of remission (
1), time to remission, response to coordinated specialty care (
2), response to antipsychotics (
3), symptom severity, and psychosocial function (
4). In other domains of illness course, there is a lack of convergent findings (
5), notably in the lack of an association between DUP and cognitive functioning (
6). However, while some studies have not detected an effect of DUP (
7), meta-analyses show that DUP explains 2%−13% of variance in outcome, depending on the sample and duration of the follow-up period (
4,
8). DUP is one of the more potent predictors of course in schizophrenia, with an effect larger than that of premorbid adjustment (
4,
9) and age at onset (
10). Gender may play a larger role (
11), but unlike most other predictors, DUP is modifiable. One aim of early intervention programs has been to identify psychosis in its early stages and minimize DUP (
2,
12,
13).
Why long DUP is associated with a poor illness course remains unclear. It has been hypothesized that untreated psychotic symptoms are toxic, meaning that a long DUP results in irreversible neurological or psychosocial damage (
14–
16). According to the neurological variant of this hypothesis, commonly referred to as neurotoxicity, individuals have similar premorbid functioning, but a long DUP results in more neuronal damage, greater functional decline, and chronic impairment. While long DUP appears to be associated with structural and functional abnormalities (
17–
19), the overall evidence remains inconclusive (
20,
21). Regardless of associations with brain structure or function, untreated psychosis could result in psychosocial toxicity (
16), in which untreated psychosis prevents the individual from navigating developmental hurdles, resulting in chronic impairment.
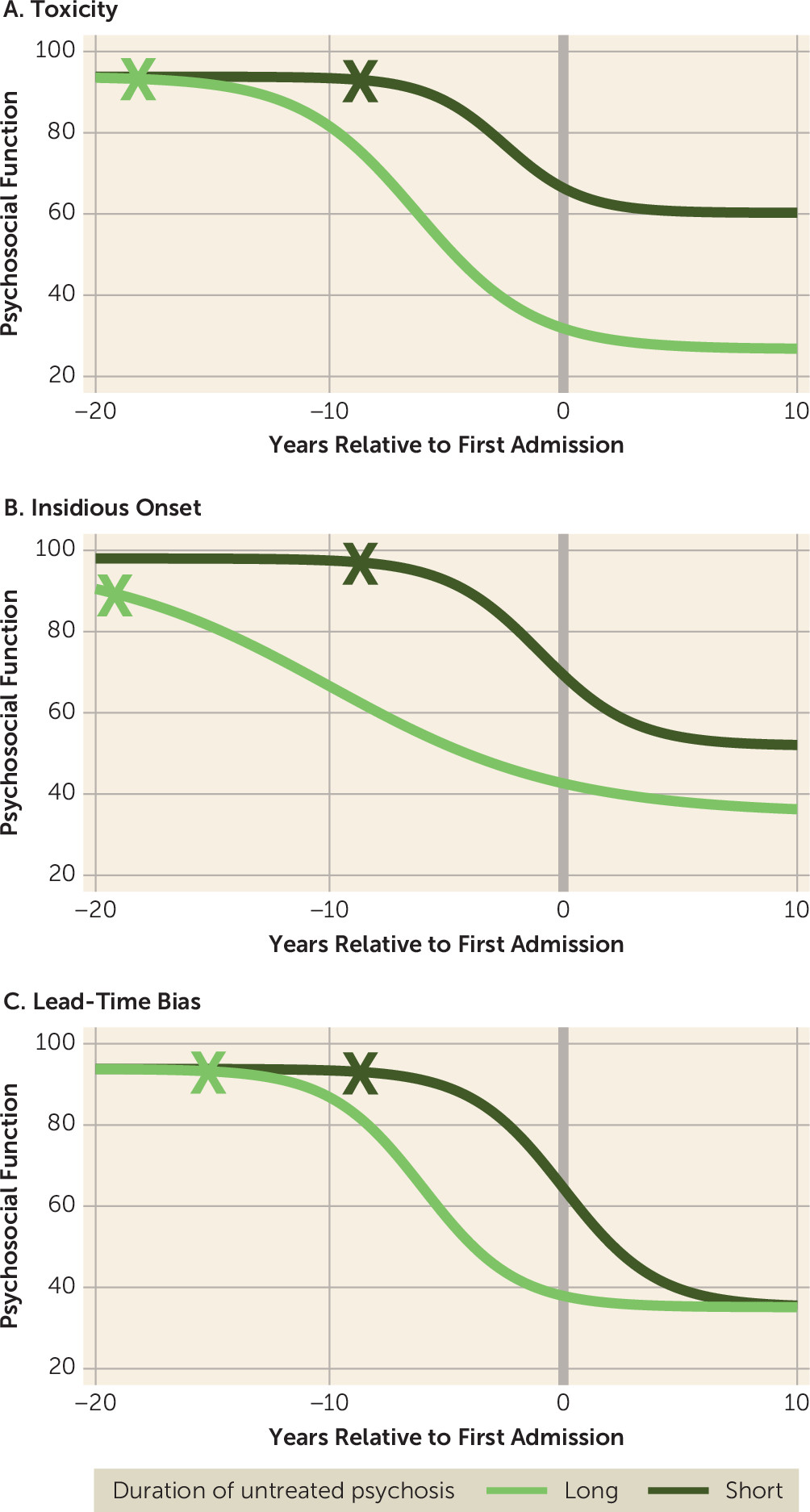
Figure 1A depicts the hypothesis that long DUP is either biologically or psychosocially toxic, or both.
Alternatively, some evidence suggests that long DUP reflects a more severe form of schizophrenia, typified by an early and insidious onset (
22,
23), poor premorbid functioning (
24), and treatment resistance (
3).
Figure 1B illustrates this hypothesis. A patient with long DUP is more impaired throughout the illness course. This hypothesis is consistent with longitudinal research showing that a long DUP is associated with lower odds of recovery after the first psychotic episode and more commonly precedes nonaffective, as opposed to affective, psychosis (
5,
25).
A third explanation is that DUP reflects differences in illness stage—that is, DUP does not predict a worse illness trajectory, but it does indicate that an individual is farther along in illness trajectory. Compared with someone with short DUP, a patient with long DUP may already be in an advanced stage of illness by first admission (
26) and therefore functioning more poorly. If so, comparing short- and long-DUP individuals would introduce lead-time bias, a known artifact of epidemiological studies in which early detection appears to improve outcomes because it shifts the observation window forward.
Figure 1C depicts this alternative. Patients with long and short DUP are on the same trajectory, only shifted relative to entry in the study. According to this hypothesis, if time is measured relative to psychosis onset rather than entry into the study, outcomes will be unrelated to DUP.
These models generate testable predictions. If the toxicity hypothesis holds, DUP should be associated with long-term but not premorbid deficits in psychosocial function. If long DUP indicates a more insidious, persistent form of illness, DUP should be associated with differences in both premorbid and long-term psychosocial function. If lead-time bias explains the observed effect, DUP should be associated with psychosocial function only in the period surrounding first admission, and defining illness course relative to psychosis onset should wipe out the association with DUP. A rigorous test of these predictions requires access to several kinds of data: premorbid psychosocial function, date of psychosis onset, date of first treatment, and long-term psychosocial function after onset. The present study is, to our knowledge, the first to test these alternative explanations.
Methods
Sample and Procedure
Data were drawn from the Suffolk County Mental Health Project, a longitudinal study of first-admission psychosis (
27,
28). Between 1989 and 1995, individuals with first-admission psychosis were recruited from the 12 inpatient facilities in Suffolk County, N.Y. (response rate, 72%). The Stony Brook University Committee on Research Involving Human Subjects and the hospital review boards approved the protocol annually. Written consent was obtained from all study participants or from the parents of minors. Eligibility criteria included residence in Suffolk County, age between 15 and 60, ability to speak English, IQ >70, first admission within the past 6 months, current psychosis, no apparent medical etiology for psychotic symptoms, and capacity to provide informed consent. In-person follow-up interviews were conducted at 6 months, 24 months, 48 months, 10 years, and 20 years after baseline.
At baseline, 628 patients met inclusion criteria. To select those with a reliable schizophrenia diagnosis, the cohort was defined by the last available study diagnosis. Of the 628 participants ascertained at first hospitalization, 287 had a schizophrenia spectrum diagnosis (schizophrenia, schizoaffective, or schizophreniform disorder) at their last available consensus review (
29). Their demographic characteristics are reported in
Table 1. Detailed statistics on the distribution of DUP are reported in Table S1 in the
online supplement.
Measures
Diagnosis.
Research diagnoses were made by the consensus of study psychiatrists at baseline, 6 months, 24 months, 10 years, and 20 years using all available information (the diagnostic process is reported in reference
29), including medical records, interviews with significant others, and the Structured Clinical Interview for DSM-III at first admission and for DSM-IV (SCID) thereafter (
30,
31).
Psychosocial functioning.
Premorbid psychosocial functioning was assessed using an interview based on the Premorbid Adjustment Scale (PAS) (
32,
33), which was administered to participants and significant others at baseline and at month 6. Master’s-level social workers with experience treating patients with chronic mental illness made initial PAS ratings based on school records, the participant’s PAS responses, and parents’ PAS responses, if available. Ratings were confirmed by R.K. The PAS consists of five domains (sociability and withdrawal, peer relationships, scholastic performance, adaptation to school, and social-sexual relationships) rated on a 7-point scale (scores range from 0 to 6, with 0 representing good functioning). Rating periods covered childhood (up to age 11), early adolescence (ages 12–15), and late adolescence (ages 16–18).
After first hospitalization, study psychiatrists made consensus psychosocial functioning ratings using the Global Assessment of Functioning Scale (GAF). GAF ratings combined symptom and functional impairment using all available information. The ratings reflected the best level of functioning over any 1-month period in the past year. Between the PAS (three time points) and the GAF (six time points), 2,137 ratings of psychosocial functioning were available across the nine time points.
To express psychosocial function on the same metric throughout, we transformed PAS scores to the GAF metric. First, PAS scores were reverse transformed so that higher numbers reflected better function, and were rescaled to a 0–1 metric. Next, composite scores were calculated as the mean of the five PAS items. Seventy-seven individuals had their first admission in late adolescence and thus had late-adolescent PAS and baseline GAF ratings for the same time period. This group did not differ from the larger sample in terms of functioning in childhood or early adolescence or by baseline hospitalization (see Table S2 in the online supplement). PAS scores were rescaled to the GAF metric by adding the difference in means (21.5), then multiplying by the ratio of their standard deviations (62.3). Because of illness onset, the number of premorbid ratings decreased from 265 in childhood to 259 in early adolescence to 233 in late adolescence.
Duration of untreated psychosis.
DUP was defined as the interval between the onset of the first psychotic symptom and the first psychiatric hospital admission. The date of onset was determined from symptom timelines obtained during the first admission and 6-month follow-up diagnostic interviews (the SCID), in which interviewers assessed the first date of onset for all threshold hallucinations, delusions, and catatonic symptoms. This information was supplemented by informant interviews that covered prebaseline psychotic symptoms, school records, and medical records. At the 24-month follow-up, psychiatrists used all available information to determine the date of onset of the first clear psychotic symptom. The distribution of DUP was highly skewed, ranging from zero days to 24 years (mean days, 726, SD=94.89; median days, 346, interquartile range [IQR]=200–945). This range is comparable with two meta-analyses on DUP (
4,
8), which reported mean DUPs of 721 days and 427 days.
Many definitions of DUP have been used in the literature (
16). Because some studies of neurotoxicity define the end of the DUP interval as the first treatment with antipsychotic medication, we also calculated DUP according to this operationalization. The median of this score (310 days, IQR=150–671) was somewhat shorter than that reported by Kane and colleagues in treatment programs across 21 states in the United States (median days, 518) (
2). The two DUP scores were strongly correlated (r=0.77) and produced the same pattern of results in subsequent analyses. Table S3 in the
online supplement reports the results of analyses defining DUP relative to first treatment with antipsychotic medication.
Covariates.
Occupational status was quantified as the occupation of the primary income earner of the participant’s family, rated on the Hollingshead index of occupational status, which is a scale from 1 (“large business owner/major professional/executive”) to 8 (“not working”) (based on reference
34). Slightly more than half of participants were of an occupational status of 5, which equated to “skilled laborer” or greater (see
Table 1). Prescription of antipsychotic medication was based on participants’ self-report, corroborated by medical records when available. This is a dichotomous variable that was coded “1” for participants who received prescriptions for antipsychotic medication for greater than 25% of the interval, and “0” for all others. The proportion of participants who received prescriptions for antipsychotic medication at each time point is reported in
Table 1.
Missing Data
DUP was known for all 287 individuals with a schizophrenia spectrum diagnosis. Psychosocial function ratings were available for at least 70% of participants at each time point. Forty-three participants died over the study’s course, accounting for 14% of missing data points. Participants whose psychosocial function ratings were missing at any time point did not differ significantly in gender or occupational status from those for whom ratings were known. Minority participants were more likely to be missing data in childhood (χ2=17.86, df=4, p=0.001) and early adolescence (χ2=13.67, df=4, p=0.008). However, missingness status was not associated with race at any other time point. Participants whose psychosocial function ratings were known were more likely to be receiving antipsychotic medication at 6 months (Fisher’s exact test p=0.02), at 24 months (p<0.001), and at 48 months (p<0.001). Analyses used full information maximum likelihood estimation, which includes partial cases. Table S4 in the online supplement reports the number of psychosocial function ratings available at each follow-up, as well as their distributions.
Analyses
For cross-sectional analyses of the association between DUP and psychosocial function, DUP was dichotomized by a median split. All other analyses quantified DUP as a continuous variable.
Because of the nonnormal distribution of DUP, associations between DUP and change in psychosocial function before and after first admission were tested using Kendall rank-order correlations.
Associations between DUP and illness course were first visualized using a LOESS function, a scatterplot smoother. Next, associations were tested using multilevel spline regression models. Multilevel spline models include random-effects estimates of the slope and intercept for each participant, thus modeling individual trajectories. However, these results focus on fixed effects of the multilevel models, which reflect the sample average. Spline models allow for nonlinear trajectories by estimating a point or points along the independent variable—time—at which the average trajectory changes. For a review of this method, see Howe and colleagues (
35). All multilevel spline models were estimated using the GLIMMIX function in SAS (SAS Institute, Cary, N.C.).
Multilevel spline models were built in the following order. First, we modeled mean psychosocial function. Second, we added time as a predictor, measured relative to either psychosis onset or first admission. Third, we added DUP to quantify stable differences in psychosocial function explained by DUP. Fourth, we estimated an interaction between DUP and time to test whether DUP predicted differing trajectories of psychosocial function. For each model, we estimated the point at which psychosocial trajectories changed by placing the inflection point at every consecutive 1-year interval and comparing model fitness via the Bayesian information criterion (reported in Table S5 in the online supplement). Optimal models were selected by comparing fit via the same criterion (reported in Table S6 in the online supplement).
Finally, all analyses were repeated to adjust for gender, occupational status, race, and prescription of an antipsychotic medication. These covariates were added as predictors of both intercepts and slopes.
Results
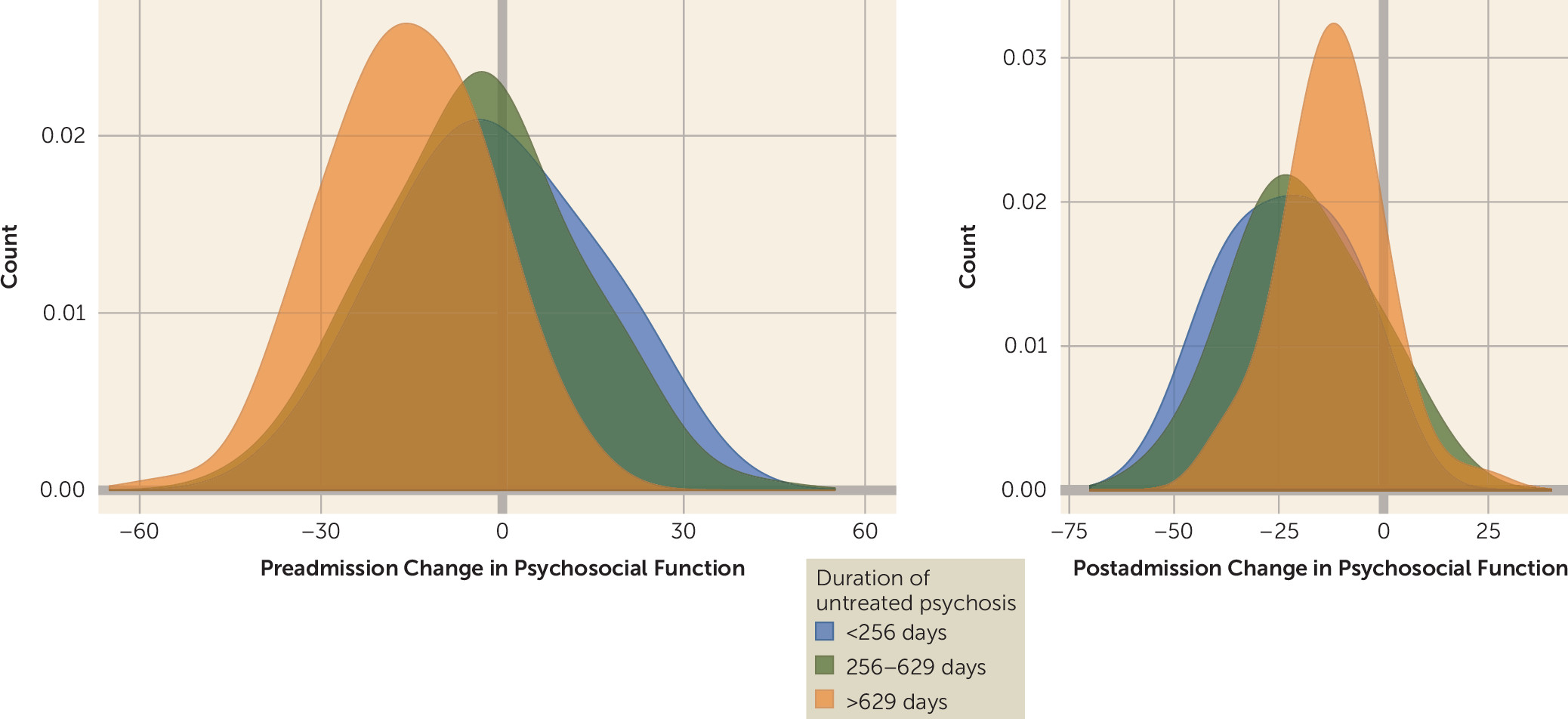
DUP was associated with psychosocial function at first admission (Cohen’s d=0.75, p<0.001), 6 months after first admission (d=0.34, p=0.01), and 24 months after first admission (d=0.38, p=0.004). The GAF was assessed relative to the best month in the past year. As a result, ratings at first admission and at 6-month follow-up may have reflected premorbid function for those with short DUP. Note, however, that group differences at 24 months do not show such overlap and remain significant. Associations outside this window were not significant; that is, DUP was not associated with differences in either premorbid or long-term psychosocial function. Bivariate correlations indicated that a longer DUP was associated with greater declines in psychosocial function between childhood and first admission (tau=−0.26, p<0.001). However, in the follow-up period, the opposite pattern emerged. Shorter DUP was associated with larger postonset declines in psychosocial function (tau=0.24, p=0.001).
Figure 2 depicts the distribution of pre- and postadmission changes in psychosocial function broken down by tertiles of DUP.
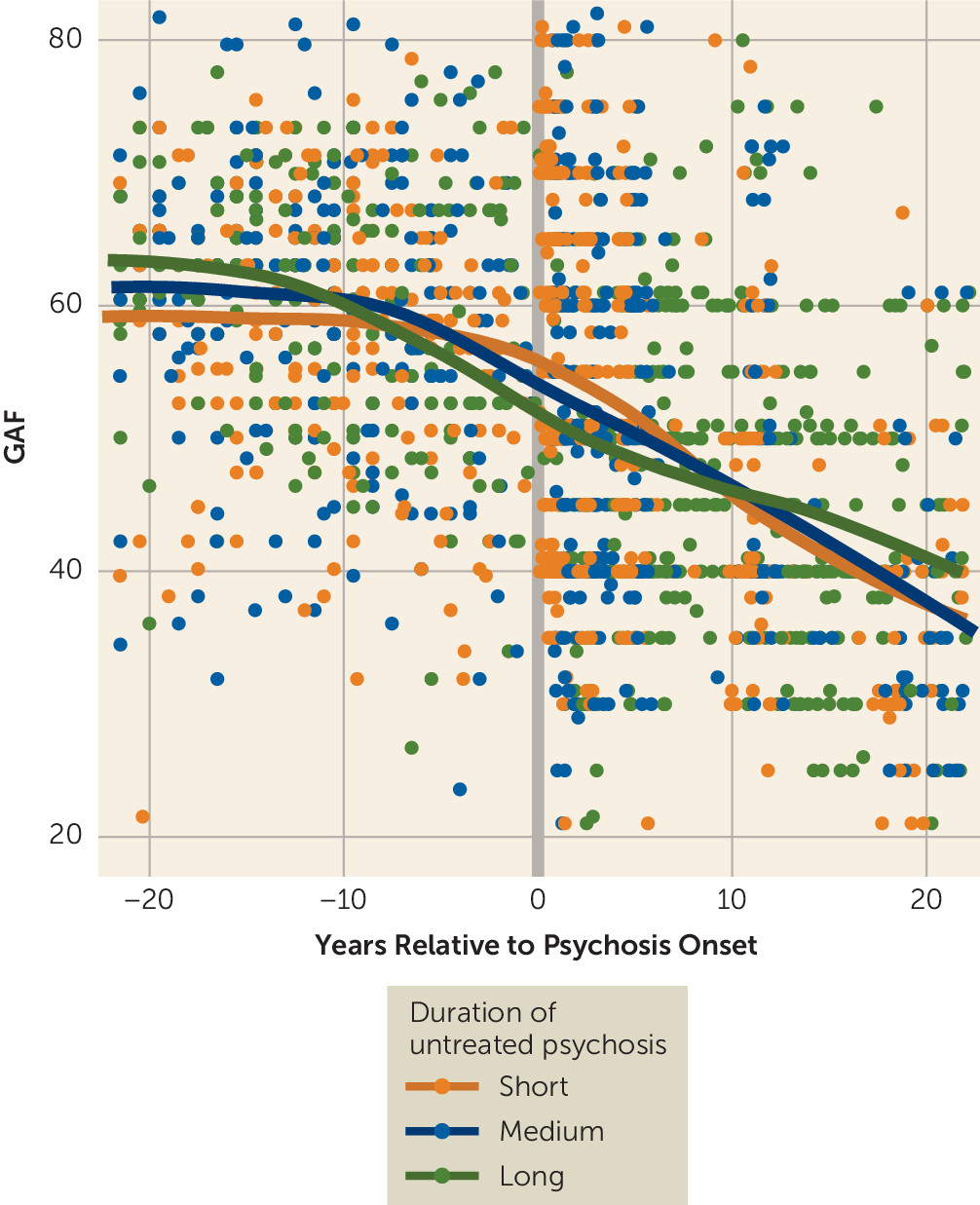
Figure 3 depicts psychosocial function relative to first psychotic symptom.
Table 2 reports fixed-effects estimates of the multilevel spline models based on these two conceptualizations. When psychosocial function was analyzed relative to first admission, DUP was associated with illness course across the lifespan (B=−0.04, 95% CI=−0.06, −0.03, p<0.001). When psychosocial function was analyzed relative to onset of the first psychotic symptom, DUP was no longer a significant predictor (B=0.00, 95% CI=−0.01, 0.02, p=0.79). We also estimated the interaction between included DUP and time and found that this worsened fit, indicating that DUP did not predict the rate of functional decline (see Table S6 in the
online supplement). Figure S1 in the
online supplement depicts the model-implied illness course for individuals with a long or short DUP, plotted relative to psychosis onset. The model-implied trajectories are very similar, and the difference between the two lines is not statistically significant.
In post hoc analyses, we also tested the effects of gender, race, and occupational status as predictors of illness trajectories. These models had worse fit to the data than models with simple mean effects of these covariates, and they were not significant predictors of illness course.
Discussion
In this study, we tested three different hypotheses regarding the link between DUP and illness course. The toxicity hypothesis suggests that untreated psychosis causes irreversible neuronal or psychosocial damage (
14,
19), leading to long-term differences in illness course. Alternatively, a long DUP has been hypothesized to reflect, rather than cause, a more insidious, persistent psychotic disorder (
22,
36,
37). Here we describe a third hypothesis, which is that the effect of DUP is an artifact of lead-time bias. Long-DUP patients are ahead of short-DUP patients in illness progression at any given study time point, causing spurious differences between groups even though they are on the same trajectory.
In a sample of 287 individuals recruited during their first admission for psychosis and ultimately diagnosed with schizophrenia or schizoaffective disorder, and for whom symptom severity and psychosocial function were characterized at 2,137 points from childhood to 20 years postadmission, both long- and short-DUP groups experienced declines. Long-DUP patients experienced most of these declines prior to first admission. Short-DUP patients were not spared, but rather experienced declines after first admission. In this way, lead-time bias creates the illusion of a treatment effect attributable to early intervention. Indeed, DUP no longer predicted trajectories when individuals were compared in terms of time relative to psychosis onset.
These findings suggest a potential for biased inferences in studies of first-episode psychosis. Studies that assess outcomes for a short period after first admission may identify protective effects of early diagnosis or treatment that actually reflect differences in illness stage rather than changes in illness course. However, these results should not be interpreted as evidence that early intervention is ineffective or that schizophrenia results in an inevitable decline. Rather, our results point to a need to control for lead-time bias to assess the effect of early interventions. For instance, in this cohort, the association between DUP and psychosocial function at first admission (d=0.75) was greater than estimates of antipsychotic efficacy, which are large (
38). Such confounding effects significantly reduce statistical power to detect real treatment effects.
Comprehensive pharmacological and psychosocial treatment has been shown to be effective in remediating symptoms and improving quality of life in schizophrenia (
2,
39). However, without sustained intervention, a majority of patients relapse (
40,
41). This epidemiological cohort has received intermittent and inconsistent care that relied primarily on antipsychotic medications, as was typical of the era, which may explain the lack of change in trajectory after first admission (
42–
44). Although early intervention alone may not halt the disease process, comprehensive and sustained care improves the quality of life for those with schizophrenia.
Limitations
In our analyses, both the date of onset and premorbid function were estimated based on information collected between the first admission and 6 months later. Depending on the length of DUP and age at first admission, this process could require collecting information about events that occurred years ago. We minimized error from retrospective assessment by supplementing self-report interviews with interviews with significant others and with historical data from both school and medical records (
45). The analysis is also limited by the use of different measures of premorbid and postadmission psychosocial function, which required converting one metric to another (
46). To our knowledge, however, no single measure could capture psychosocial function early in development as well as symptoms and functioning in adulthood.
Long periods of time passed between some of the follow-up interviews; however, data were available for time points critical to distinguishing the hypothesized trajectories. In addition, the long-term nature of the study allowed for reappraisal of diagnoses based on longitudinal data. This increases diagnostic validity, reducing the risk of excluding patients with schizophrenia whose initial presentation reflected that of another psychotic disorder with a better prognosis. There are other outcomes that may be associated with DUP, such as symptom severity or need for treatment, which were not addressed here because of the lack of preadmission data. In addition, we note that psychosocial function is an indirect measure of neurotoxicity, unlike direct evidence from neuroimaging. Further research should investigate trajectories of these outcomes.
As a first-admission study, this sample does not include people with schizophrenia who were never hospitalized. However, the range of DUP values is broadly in line with other first-episode studies (
4) and is shorter than that of a large and diverse sample drawn from clinical settings across the United States (
2), suggesting that our sample is not biased toward advanced cases. In addition, the wide age range of the sample and the range of observed DUP values increase statistical power to detect an effect, relative to analyses of intervention studies aimed at minimizing DUP. As with any single study, these findings require replication.
The interpretation of this and other studies of DUP is qualified by the many ways in which DUP can be defined. We compared multiple definitions of DUP, none of which changed the results. However, there are alternative definitions—the interval start could be defined as the first psychiatric symptom of any kind (
16), and the endpoint as the date of first effective treatment (
47) or first contact with a mental health care provider (
48)—that depend on data not available in this cohort.
Conclusions
An inverse association between DUP and illness course is often found in schizophrenia research. However, the association appears to be explained by lead-time bias, in which a short DUP is associated with better outcomes because DUP is confounded with illness stage. That is, those with a short DUP are in an earlier stage and therefore appear to have better outcomes than those with a long DUP, who are in a later stage. When lead time was accounted for by analyzing disease course relative to psychosis onset, DUP no longer predicted outcomes in our cohort. These findings argue against the toxicity of untreated psychosis as well as the hypothesis that a long DUP signals a more insidious, severe psychotic disorder. To avoid confounding by lead-time bias, studies of first-episode schizophrenia should estimate the course of illness and treatment response relative to time since psychosis onset. Treatments more potent than those available to this cohort may be able to alter illness trajectory and make early intervention beneficial.
Acknowledgments
The authors gratefully acknowledge the support of the participants and mental health community of Suffolk County, N.Y., for contributing their time and energy to this project, and they thank Janet Lavelle, Jonathan Sandler, and the interviewers for their careful assessments, as well as the psychiatrists who derived the consensus diagnoses.