Social determinants, which are social and environmental conditions experienced across the lifespan (
1), produce health inequalities along a society’s social gradient in a way that disproportionately burdens the most marginalized and disadvantaged (
2). In their theoretical model of social determinants, Compton and Shim (
3) describe how policy and social norms create pervasive inequities in social and environmental conditions across the U.S. population—conditions that, both directly and in concert with biological risk, affect onset, severity, and remission of psychopathology (
2 –
4). These social policies and norms influence access to important resources (e.g., education, health care, social capital) and exposure to environmental toxins and to stressors, such as childhood trauma, neighborhood deprivation, and discrimination (
3). Within the U.S. context, one of the predominant organizing frameworks of these social policies and norms is structural racism (
5,
6)—a socially constructed taxonomic stratification of power based on proximity to Whiteness, with individuals of African descent being the most distal category (
7). Classic theoretical models, including Clark and colleagues’ biopsychosocial model of racism (
8) and Harrell’s multidimensional model of racism-related stress (
9), delineate the multiple pathways through which racism creates an accumulation of psychological and physiological stress responses that negatively affect health over time. Drawing on this framework, Link and Phelan applied their theoretical model of fundamental causes to describe how racism is a fundamental cause of health inequity in the United States (
10,
11). In short, structural racism has an enduring association with health outcomes because it is maintained through multiple pathways by limiting access to flexible resources, such as those connected to neighborhood segregation and individual freedom to control life circumstances (
10). Together, both theoretical models (
3,
10) provide a framework for understanding how structural racism serves as a complex cause of mental health outcomes through social and environmental intermediary pathways connected to biological risk. Yet the study of such social determinants of psychosis has received limited investment in American psychiatry (
12). More attention is often placed on understanding the biological and individual factors that lead to mental illness (
3) despite increasing theoretical emphasis on the importance of the confluence of biological and social factors (
13 –
16).
European studies have consistently found higher psychosis incidence and prevalence among people with African and Caribbean heritage compared with majority White populations (
17), highlighting the important etiological role of the social environment (e.g., social inequality, adversity, and discrimination [
18 –
21]) in psychosis risk (
14). In one of the first empirical studies on psychosis incidence in a minoritized population, Ødegård (
22) found in 1932 that Norwegian immigrants to the United States were twice as likely to be diagnosed with schizophrenia compared with U.S.-born individuals and those born and living in Norway. While racially similar to the contemporaneous dominant caste of American society (i.e., of European ancestry), the Norwegian immigrants were still othered and marginalized within the social hierarchy of that time for being immigrants. This study inspired a line of fruitful research examining associations between ethnic minority status and psychosis in primarily European countries. The United States, by contrast, has lagged behind Europe in examining the link between minority status and psychosis incidence. Our contemporary understanding of psychosis incidence in minoritized U.S. racial groups has been complicated by key factors, including the lack of a centralized health register to obtain an accurate denominator for incidence calculation; methodological issues with sample selection in epidemiological studies (e.g., differential access to health care based on race and socioeconomic status [
23]); and misdiagnosis based on perceived racial group (
24). While several U.S. studies have demonstrated that Black people and sometimes Latino people are overrepresented in the patient population with psychotic disorders (
25 –
29), these findings have been complicated by studies demonstrating that clinicians tend to misinterpret and misattribute symptomatic phenomenology presented by Black people, resulting in the overdiagnosis of schizophrenia and underdiagnosis of affective disorders (
30 –
35). The strongest evidence of a racial disparity in psychosis comes from a Kaiser Permanente California birth cohort study (
36) that demonstrated a threefold elevated risk of schizophrenia spectrum diagnoses for Black members compared with White members; however, after adjustment for several socioeconomic status indicators, this risk was reduced to 1.92, with a confidence interval that narrowly included zero. Additionally, evidence from nationally representative epidemiological studies (
37 –
39) shows higher 12-month prevalence estimates of psychotic symptoms among Black (e.g., 15.3%) and Latino (e.g., 13.6%) Americans compared with White Americans (e.g., 9.7%) (
40). To date, the United States has not adopted a representative, population-based approach sufficiently powered for the study of clinical psychosis incidence that simultaneously adjusts for race-based misdiagnosis and related socioeconomic disadvantage. Such investment is critical to have stable, reliable estimates of any racial disparity in psychosis risk. The lack of clarity on this issue has stymied efforts to elucidate the relationship between racial and ethnic minoritization and psychosis in the United States.
Even though psychosis incidence and prevalence across racial groups in the United States remains inconclusive, the central role that structural racism plays in shaping the distribution of risk factors for psychosis across the U.S. population is less equivocal. This social taxonomy in the United States has roots in a racial trauma history that gave rise to a pervasive system of structural racism that persists today (
41). The genocide of First Nations people, the theft of their land, and the enslavement of over 3.9 million Africans and their American-born descendants (
42) to build White American wealth and capital are historical traumas embedded in the foundation of the United States and its legacy of oppression, segregation, and economic injustices (e.g., Jim Crow laws, mass incarceration) (
43). The repercussion of this legacy is evident in sharp inequities along racial lines (
44). A striking example of this inequity exists in New Jersey, where the racial differences in wealth are extreme, with the median net worth for White families at $309,396 compared with just $7,020 and $5,900, respectively, for Latino and Black families (
45). This inequity necessarily translates into very different lived experiences on average in education, health care, and neighborhood exposures—inequities widened further because important services in the United States (e.g., schools) are funded through property taxes.
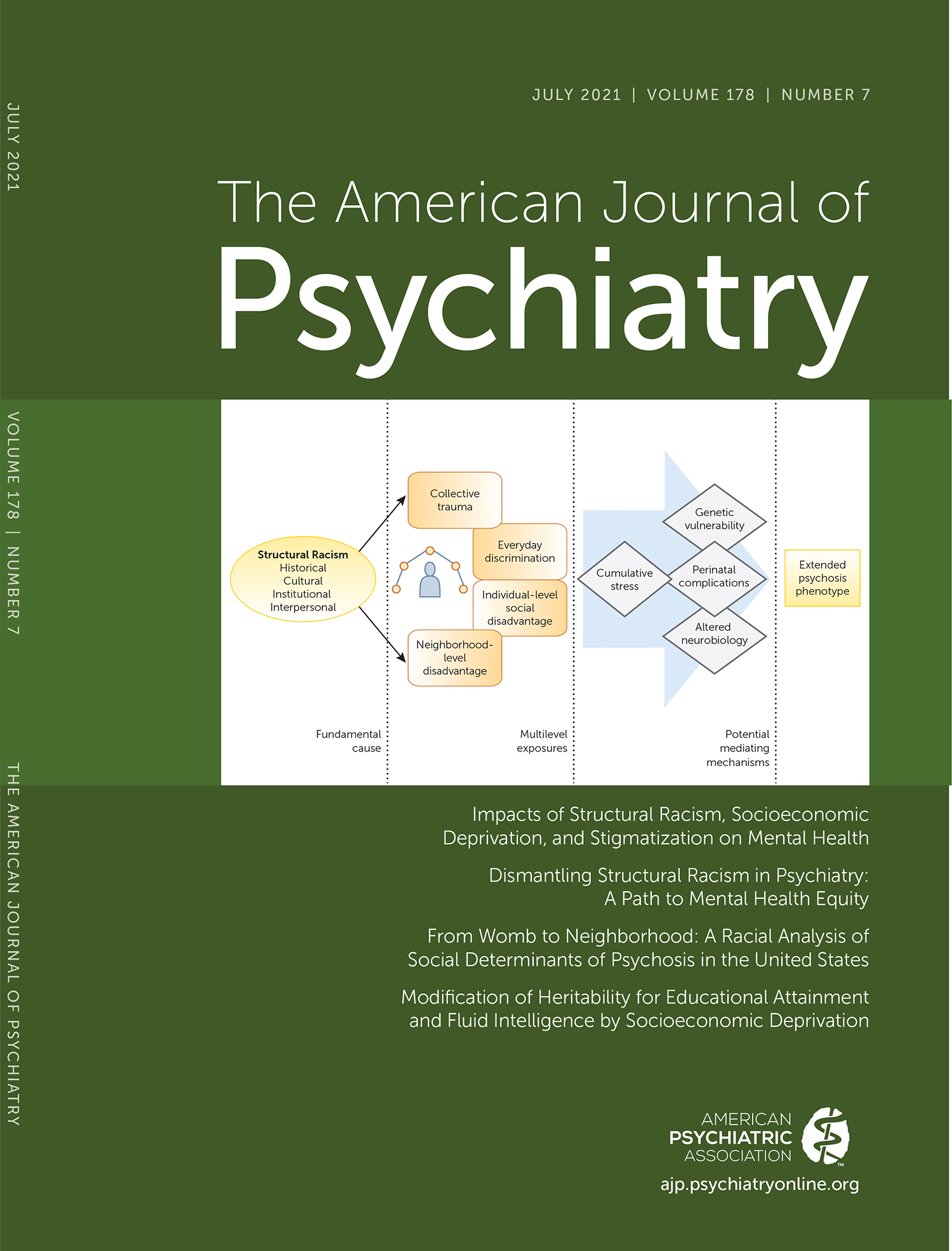
This narrative review seeks to provide the first consolidated integration of U.S.-based work on social determinants of psychosis in three key areas, with a specific focus on race and ethnicity. Being of a particular race in and of itself is not the determinant; the systematic racism that constructs the social milieu makes it relevant. Figure
1 presents a hypothesized model of how a lineage of structural racism shapes psychosis risk through social determinants at multiple levels, including those of the neighborhood and the individual. Specifically, this review focuses on risk factors within U.S. neighborhoods, trauma experienced at both collective and individual levels, and complications experienced during perinatal periods. These areas were chosen in part because of their consistent link to psychosis and how they are shaped by structural racism, although we acknowledge that they are not exclusively linked to psychosis. Studies reviewed highlight the U.S. context’s uniqueness and provide suggestions for further inquiry. Our aim is not to exhaustively review the evidence on all social determinants of psychosis, but to highlight those that seem particularly relevant for the U.S. context. We offer the model in Figure
1 as an overall framework worthy of future empirical inquiry, outlining the interconnected social mechanisms of disadvantage identified in previous European studies (
46) and underlying increased stress and other biological consequences linked with psychosis outcomes in the United States. We include studies across the psychosis continuum, from psychotic experiences in non-treatment-seeking community samples (e.g., the Collaborative Psychiatric Epidemiology Surveys) (
47) to psychosis risk syndrome in clinical high-risk population studies (e.g., the North American Prodrome Longitudinal Study) (
48) to psychotic disorders such as schizophrenia in clinical settings (
30). We also include selected studies that connect these social determinants to possible underlying biological mechanisms, implicating stress hormones (
16,
49,
50), neural activity and connectivity (
51,
52), and epigenetic mechanisms (
53).
THE NEIGHBORHOOD
Neighborhood-level factors cover a broad range of social, economic, and political conditions, including urbanicity, ethnic density, perceived neighborhood disorder (e.g., vandalism and other signals of loss of social control), residential stability, and access to resources, opportunities, and services. Among other mental health concerns, given the link between stress and psychosis (
54), adverse neighborhood conditions are associated with an increased prevalence and severity of the extended psychosis phenotype (
55).
U.S. neighborhoods have evolved to systematically and generationally perpetuate disadvantage (
41) for racially minoritized communities (
56) through both formal and informal generational segregation and discrimination (
57,
58). These forces maintain systemic inequity in community-wide access to resources, services, wealth, and opportunities (
59) comprising access to healthy foods, safe water, clean air, parks, affordable childcare, health care, education, employment opportunities, and safe housing (
60). All of these neighborhood factors confer disadvantage that is associated with cumulative stress (
61) (see Figure
1) and therefore conceivably linked to heightened risk for psychosis (
54).
In an early study, Faris and Dunham (
62) showed that urbanicity—residing in a more population-dense area—was related to higher schizophrenia rates, a finding that applied to both Black and White people. Hollingshead and Redlich (
63) continued this work by examining the relation between social class and mental health disorders, finding disproportionate rates of psychotic disorders among individuals of the lowest socioeconomic status, including many people of color.
Narita et al. (
64) found that higher neighborhood disruption (e.g., fear of being “pushed out” of one’s neighborhood or a perceived decline in local social networks) was associated with significantly greater odds of endorsing a psychotic experience in a large U.S. community sample. In a related study, Anglin et al. (
65) examined perceived neighborhood ethnic density in a large sample of young adults in an urban setting. Respondents who grew up in neighborhoods predominantly populated by a different ethnic or racial minoritized group endorsed a higher number of psychotic experiences than those who grew up in White, mixed, or racially concordant neighborhoods. These findings suggest that growing up with the experience of stressful racial dynamics in an urban community may lead to increased risk for psychosis spectrum experiences. Additionally, Ku et al. (
66) reported that neighborhood-level residential instability, as measured by the percentage of people who lived in multiple homes within 1 year, predicted earlier psychosis onset, a proxy for more severe illness course.
Future research in the United States could probe for a more refined understanding of the mechanisms that underlie the links between neighborhood-level factors and psychosis risk. For instance, lack of green space (
67) and exposure to environmental toxins (
68) correlate with psychosis in European studies. Additionally, the use of objective measures of neighborhood disorder and disruption could complement existing assessment strategies that focus on subjective accounts, providing an opportunity to better understand the relation between objective and subjective evaluation of neighborhoods, and better steer intervention strategies. Objective measures may include the use of geocoding and the mapping of addresses, which can be compared with publicly available information about a neighborhood, such as average socioeconomic status, crime, and local resources.
TRAUMA IN A U.S. CONTEXT
Acute or chronic traumatic events and major life stressors have an impact on psychosocial and biological stress responses, which may contribute to the pathogenesis of psychosis (
54,
69 –
71). In the United States, studies have focused primarily on the impact of adverse childhood experiences (e.g., abuse, neglect, incarcerated family members), showing that at least 61% of individuals in the U.S. population endorse at least one event, with racial and ethnic minoritized individuals having higher adverse childhood experience exposure rates (
69). Findings in the general population appear to differ by trauma type, with White Americans reporting an overall higher traumatic event incidence (
72), but minoritized racial groups reporting a higher incidence of childhood maltreatment and exposure to violence (
72). U.S.-based research has identified various traumatic events as potential contributors to psychosis risk, including adverse childhood experiences, such as emotional or physical neglect (
73 –
75), psychological or physical bullying (
76 –
78), developmental challenges associated with foster care (
79), and parental separation or death (
80,
81). Perceived discrimination has also been associated with psychosis (
76,
82,
83).
Trauma and adverse childhood experiences are common among individuals with schizophrenia, with 86% of individuals with schizophrenia surveyed in one study reporting at least one adverse childhood experience (
81). Those at clinical high risk for psychosis also report having had at least one traumatic experience (∼85%−97%) (
80,
84), with many individuals endorsing more than one traumatic experience (
81,
84). In the U.S. National Comorbidity Survey, experiencing one trauma type was not associated with psychosis outcomes, but experiencing more than one was, indicating a possible compounding effect (
85). More frequent victimization, trauma, or stressors is associated with increased psychotic symptom frequency or severity in a dose-response pattern (
73,
85 –
87). This is relevant as revictimization is high after an initial trauma (
88).
Across the psychosis continuum, trauma and adversity rates, including for physical abuse (
80), sexual abuse (
81), domestic violence (
81), separation from a parent (i.e., divorce, raised by nonbiological caregivers) (
89), and parental death (
81), are significantly higher for marginalized racial groups compared with White people. Socioenvironmental adversity, often found in more disadvantaged racially minoritized communities, may intersect with collective historical racial trauma to increase exposure to chronic stress and traumatic events.
Police victimization and gun violence are examples of significant social health crises disproportionately affecting racially minoritized communities in the United States (
90,
91), as Black, First Nation, and Latino men are killed by police at higher rates compared with White men (
90). Police violence in particular may be more impactful on mental health because it is enacted by people who are state sanctioned to enact violence and there is little legal recourse for such violence (
92). Black men, specifically, have a 1 in 1,000 chance of being a victim of lethal force by police over their lifetime, in contrast to 39 in 100,000 for their White counterparts (
93). In addition, Black and Latino individuals have a disproportionately higher rate of exposure to gun violence fatalities (
94). Death by police violence and homicide by firearm are leading causes of death of young Black men (
93,
95,
96).
This creates a unique type of collective trauma in the United States, where communities have been intimately or vicariously affected by the trauma of police victimization and gun violence. In a diverse sample from four large U.S. urban centers, individuals who self-reported different types of police victimization (e.g., physical [with or without a weapon], sexual, psychological, neglect) were more likely to report psychotic experiences (
97). Likewise, greater exposure to gun violence fatalities, regardless of police involvement, was positively associated with psychotic experiences (
94). Given that other similarly educated countries, such as England and Japan, report zero to seven police killings per year, compared with the average of 1,100 incidents per year in the United States (
97), police victimization and gun violence should receive more attention as stress- and trauma-related social determinants of psychosis risk in the United States.
RACIAL DISPARITIES DURING PRE- AND PERINATAL PERIODS
A variety of obstetric complications have been associated with increased risk for psychotic disorders in U.S. samples (
98). Various infections (
99), increases in maternal inflammation (
100,
101), maternal stress (
102,
103), hypoxia-associated obstetric complications (i.e., decreased oxygen to the fetus [
104]), decreased fetal growth [
105,
106]), lower maternal hemoglobin levels (
107), and alterations in various nutrients (
108) during pregnancy have been linked to increased prevalence of psychotic disorders in the United States (
109). All of these prospective results have been based on birth cohorts that enrolled pregnant women during the 1950s and 1960s and followed them and their offspring, collecting thousands of variables, including prenatal blood samples (
110,
111). Nevertheless, not only do these studies suffer from cohort effects due to political climates and demographic characteristics that are not generalizable to contemporary samples, but also none of these studies adequately incorporated known racial and ethnic disparities in birth complications commonly found in the United States into their explanatory models.
The latter point is of paramount importance, given that Black women in the United States are at substantially increased risk for many obstetric complications, spanning preterm delivery, reduced fetal growth, and increased infection rates (
112,
113). Importantly, findings indicate that access to prenatal care and a variety of sociodemographic factors (e.g., income) do not explain racial disparities in birth outcomes (
114). Moreover, Black women with higher socioeconomic status have an increased risk of obstetric complications compared with non-Hispanic White women with lower socioeconomic status (
114). Neighborhood- and individual-level factors appear to affect the disparity in these outcomes. A recent study revealed that exposure to environmental contaminants (e.g., air pollution, heat exposure) is linked to higher rates of preterm birth and low birth weight differentially in Black mothers compared with other mothers in the United States (
115), possibly as a result of an interaction between prenatal stress and contaminants (
116). Additionally, psychological distress related to perceived neighborhood crime levels and breakdown of order and social control have also been linked to preterm birth in Black mothers (
117). Studies also have found that Black women experience a higher number of stressors during pregnancy, although these stressful life events on their own do not appear to account for racial disparities in obstetric complications when considering events that do not include discrimination (
118). Other findings suggest that perceived discrimination significantly predicted lower birth weight among Black women, but not in other racial or ethnic groups (
119). In fact, both objective measures of neighborhood environment and perceived racial discrimination have been associated with increased psychological distress in pregnant Black women (
117).
Findings also indicate that Black women are more likely to have lower cortisol levels during the second trimester of pregnancy compared with other racial and ethnic groups (
120). Lower second-trimester cortisol levels are consistent with what has been observed among women diagnosed with posttraumatic stress disorder and has been interpreted as potentially related to a lifetime of exposure to increased stress due to repeated discriminatory experiences (
120). Not only is cortisol essential for fetal growth and development, but findings indicate that lower cortisol levels in later stages of pregnancy are associated with decreased fetal growth among those who develop schizophrenia (
105,
121 –
123). Black women may also be more sensitive to the effects of stress hormones during pregnancy, with some findings suggesting that smaller increases in stress hormones produce poor birth outcomes, such as preterm delivery, among these pregnancies (
124). In addition, Black women show higher levels of other stress biomarkers as compared with White women of the same socioeconomic status in mid to late pregnancy, including particular inflammatory markers (e.g., C-reactive protein) and adrenocorticotropic hormone (
125,
126). Furthermore, Black women have shown a more robust inflammatory response to a laboratory stressor than White women in mid-pregnancy, and elevated inflammatory cytokines were related to experiences of perceived discrimination (
98). In their review of racism and perinatal effects, Conradt et al. (
127) argue that discriminatory experiences in pregnant women of color may increase allostatic load, wearing down the body’s regulatory systems, causing biological and epigenetic changes in the infant as well as differences in birth outcomes. Cumulatively, these findings highlight a complex picture, with both decreased and increased maternal cortisol levels and other stress biomarkers, potentially leading to poor birth outcomes and subsequent risk for psychotic disorders in adulthood.
Finally, there is evidence that many Latina women have lower birth complication rates if they are recent immigrants to the United States (
128); however, the longer Latina women stay in the United States, the more similar the obstetric complication rates become to those for Black women (
129,
130). These findings may be due in part to cumulative (and potentially intergenerational) exposure to discrimination during the acculturation process (
131 –
133). Studies have also identified a relationship between greater acculturation and blunted maternal cortisol response (
134) in addition to elevated concentrations of the inflammatory cytokine interleukin-6 (
135), which may be biological mechanisms through which acculturation has an impact on adverse birth outcomes. Overall, these findings suggest that racial and ethnic disparities in the rates of obstetric complications in the United States could contribute to a developmental trajectory toward psychosis and findings of higher schizophrenia rates among Black individuals, immigrant populations, and potentially other less studied groups that experience high discrimination rates (e.g., because of religion, sexuality, and other racial and ethnic identities).
DISCRIMINATION AND POSSIBLE BIOLOGICAL MECHANISMS LINKED TO PSYCHOSIS
Figure
1 illustrates structural racism as a fundamental cause of the extended psychosis phenotype through group-level processes occurring at the neighborhood level that are connected to processes occurring at the individual level (e.g., discrimination). Neighborhood-level factors (e.g., exposure to environmental contaminants, concentrations of crime) likely interact with the psychological ones to enhance chronic stress across generations, especially given how neighborhoods in the United States are structured to preserve advantages or disadvantages over time. Experiences of discrimination underlie the chronic stress experienced by many racial and ethnic minoritized individuals—stress that has been linked to physiological and neurobiological mechanisms, including psychophysiological stress responses shaped by threat appraisals and immune responses (
136). Such racial discrimination has been associated with paranoia in a dose-response pattern in nonclinical populations (psychotic experiences in Hispanic/Latino, Asian American, and Black American individuals) (
82,
137,
138) and clinical populations (
48,
76).
Our review of obstetric complications suggests that discrimination among Black and Latina mothers may contribute to these complications because of heightened responses to stress (e.g., inflammatory responses)—responses in offspring that are also caused by obstetric complications (
103). Other longitudinal work on possible biological mechanisms linking discrimination with psychosis risk indicates that such experiences can contribute to chronic activation of stress systems, leading to long-term changes in neural circuitry responsible for regulating emotional learning and the pairing of threat cues to neutral stimuli (
139). One study (
139) found that for racial and ethnic minoritized people, prior negative life experiences, such as discrimination, explained racial differences in threat-related neural and psychophysiological activity. Other work (
52) highlighted how discriminatory experiences may affect underlying neural systems in similar ways to other stressful experiences. Clark et al. (
52) found that higher levels of social discrimination in racial and ethnic minoritized populations were correlated with increased spontaneous amygdala activity and increased functional connectivity with other brain regions, particularly the thalamus. This neural activation pattern is similar to processing of other stressful experiences. Given the history of oppression, discrimination, and systemic racism in the United States, understanding the biological consequences of the unique trauma and stressors of minoritized communities will expand our understanding of risk for psychosis more generally.
Recently, Gur et al. (
140) conducted a longitudinal study exploring how environmental determinants, such as traumatic-stressful events and low socioeconomic status, affect neurodevelopment and brain function. They found that traumatic, stressful events and low socioeconomic status throughout adolescent development caused brain development to be completed earlier in addition to an overall reduction in volume. Other recent developmental work highlights the possible epigenetic effects of discrimination in African Americans. Carter et al. (
141), using gene expression data from the Family and Community Health Study, found that high exposure to discrimination during early adolescence was associated with depression in adulthood and accelerated cellular-level aging. The role of epigenetic mechanisms provides a promising avenue for future study and should be explored further in relation to psychosis etiology.
RECOMMENDATIONS
To truly adopt an antiracist framework, it is necessary to walk in the opposite direction on the path that seeks to maintain the status quo (
142). The evidence reviewed suggests that a greater appreciation of how racism shapes social determinants of psychosis would support such a framework in North American psychiatry. As a fundamental cause of mental health inequities, structural racism and the social policies and norms it shapes (e.g., preservation of neighborhood disadvantage) must be dismantled to have a complete solution. Simultaneously adjusting health care policy and how we approach early intervention for psychosis among Black and other racially minoritized groups is also necessary. As an example, health care policies could be reimagined to provide psychological intervention and protection to circumvent the detrimental impact of racial discrimination and stress on Black mothers. Many generalized stress interventions have been tested (
143,
144), but to our knowledge, there are no evidence-based interventions specifically designed to tackle race-based discrimination stress in racially minoritized pregnant mothers.
Altogether, the current evidence suggests the need to identify, address, and tackle the social determinants deeply ingrained in U.S. society, in tandem with empowering the most marginalized communities. This has the potential to lead to mental health benefits not yet attained, as there is evidence of a large unmet health care need among young people with psychosis, especially within racially minoritized communities in the United States (
145). We recommend that the field of psychiatry devote considerably more effort to addressing structural racism and social determinants of psychosis in funding priorities, training, and intervention development.
Funding Priorities and Training
In light of the morbidity and stigma associated with psychosis and schizophrenia specifically, a strong federally funded research program designed to provide reliable psychosis incidence estimates across racial and ethnic groups in the United States that systematically account for misdiagnosis is urgently needed. Relatedly, funding intervention development efforts that include multilevel targets, including those at the neighborhood level, such as those connected to collective racial trauma, may better capture an important area of risk that our review suggests contributes to psychosis outcomes. Definitive causal evidence is lacking because the critical studies have not yet been carried out, but the available evidence points to a social system of contributory causes for psychosis in the United States that may require multilevel interventions. Such interventions require equitable community partnerships that target the health of the community and include the perspective of institutions and organizations within communities (
146). As an example, Hankerson et al. (
147) are using community-partnered participatory research principles to develop and implement a depression intervention that incorporates the neighborhood-level perspective of African American churches in the local community. More funding for these approaches is needed, as they provide an opportunity to include community-level targets in interventions that would not otherwise be revealed. (See Castillo et al. [
146], for other detailed examples of community-level interventions.)
In terms of training, a better integration of the work on racial trauma (
148) in mental health training and practice would improve the ability to adequately assess for context indicators and to intervene in racially minoritized populations. The DSM-5 Cultural Formulation Interview (
149), which includes a specific section on factors within the social environment, could be used as a tool to better integrate such experiences in patient assessments. This interview broadly assesses the role of culture and context on illness presentation and the diagnostic process (
150). Incorporating a cultural formulation in the diagnosis of psychosis has been shown to facilitate reasoning and decision making about symptoms and behaviors presented by Black immigrants in Canada, leading to enhanced diagnostic clarity (
151). More training regarding how to use cultural formulations to integrate information about collective racial trauma in the social environment would support efforts to optimize and personalize treatments for racially minoritized persons with psychosis. Relatedly, a training system that requires mental health care professionals and leaders to increase their focus on structural competencies (
152) is needed. This proficiency in structural competency includes understanding how inequities in social and economic conditions shape clinical presentations, practitioner-patient interactions, and the course and efficacy of treatment once symptoms emerge across all stages of illness.
Intervention Development
Optimizing and personalizing interventions for people with psychosis are major federal funding and public health priorities (
153). Yet, there is generally a lack of empirically supported treatments to support those who have experienced racial discrimination despite its apparent role in mental illness etiology, including for psychosis. For Black and other culturally minoritized groups, treatment optimization and personalization could be enhanced if these social determinants connected to racism were adequately incorporated into early intervention and treatment models. As an example, Weisman de Mamani et al. (
154) developed a culturally informed manualized treatment for schizophrenia that focuses on family collectivism and enhancing adaptive spiritual beliefs and practices. This treatment helped reduce psychiatric symptom severity and improve quality of life, especially for Hispanic patients with schizophrenia.
There are no early intervention or treatment programs for psychosis, to our knowledge, that directly target the pernicious aspects of racism that affect Black and other culturally minoritized groups. Treatment paradigms for psychosis that focus solely on individual psychotherapy without incorporating the role of social context may be missing a significant part of the etiological variance. Multilevel (community and individual) and intergenerational approaches to the early intervention and treatment of psychosis should be considered and tested in studies using mixed methods. Neblett (
155) described the value of using qualitative approaches, such as Photovoice (
156), to study how racism affects Black youth in the local community. Photovoice is a community-based participatory research approach in which participants have the opportunity to photograph issues and themes that are of importance to the community, and through these photos, a better understanding of these issues emerges as well as a dialogue with previously marginalized or neglected voices (
157). Participatory methods similar to Photovoice can reveal novel ways to develop treatments that incorporate tackling racism in the community because it prioritizes the voice and perspective of a segment of the population that is underrepresented among researchers and clinicians (
158,
159). There is enhanced probability to reveal something innovative and constructive.
CONCLUSIONS
Our review of the U.S.-based literature on social determinants reveals a pattern of racial disparities in established risk factors for psychosis. That racism has historically structured U.S. societal systems means that the neighborhood and social context may hold a significant portion of the relative contribution of risk for psychosis. This may occur through individual-level discrimination as well as through collective trauma at the community level (e.g., police and gun violence). The evidence that these multilevel exposures may enhance chronic stress activation across generations through perinatal complications in mothers is considerable. Furthermore, evidence regarding the neurodevelopmental and neurobiological effects of discrimination, especially regarding long-term changes in neural circuits responsible for pairing threat cues to neutral stimuli, make it a critical target for further research and intervention development. Social and environmental stressors connected to structural racism (e.g., neighborhood disadvantage, collective trauma, discrimination) that are disproportionately experienced by Black and Indigenous people of color could contribute to psychosis risk in these populations. While our review revealed that much of the work in this area has focused on Black and Latino populations, these social determinants are likely also relevant for Indigenous and Asian-descended populations; more research is needed in these populations.
The disproportionate number of marginalized and disadvantaged Black people represented among individuals with psychosis in U.S. clinical settings may reflect how these traumas, discrimination, and neighborhood violence are influencing the ability to receive adequate treatment and avoid traumatic pathways to and through care. Indeed, perceived neighborhood disorder in childhood and adolescence significantly predicted delays in identification and receipt of mental health services for people with a diagnosis of psychosis (
66). Other marginalized groups, encompassing those in poor rural areas, the lesbian, gay, bisexual, transgender, queer, and intersex community (especially transgender people of color), and those with disabilities also suffer disproportional social determinants of health. Building a critical consciousness about the ways behaviors and symptoms are connected to the contexts in which we live, including in our training programs, among providers, and in our patients, can enhance practice effectiveness. More research studies that use both qualitative and quantitative methods will be necessary to fully understand the interplay between adversity, minority status, and other dynamic factors within U.S. communities and how the unique experiences of these marginalized groups influence psychotic experiences, illness development, access to care, and ability to recover.