Psilocybin: From Psychiatric Pariah to Perceived Panacea
Abstract
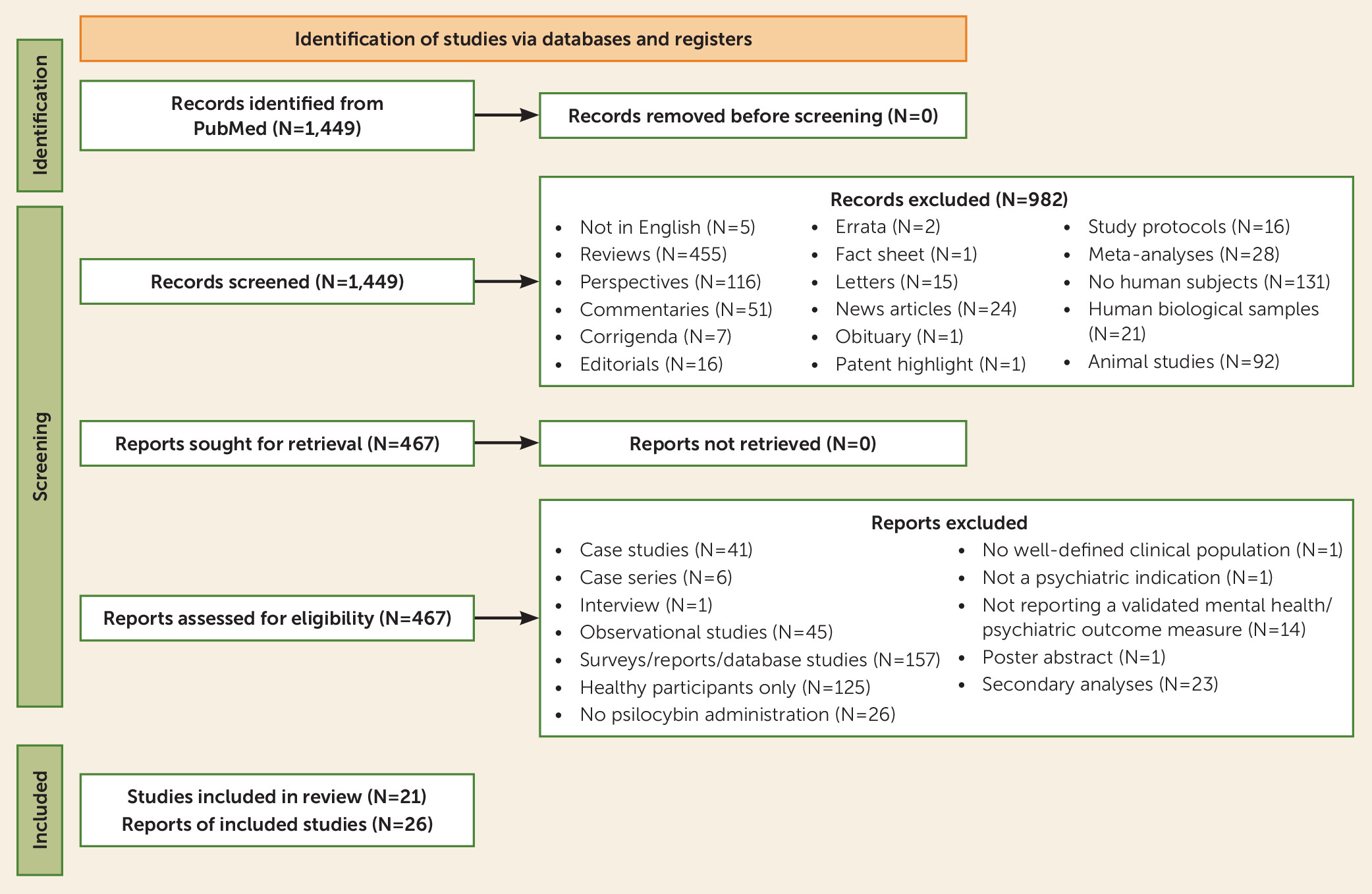
Objective:
Methods:
Results:
Conclusions:
Methods
Results
| Indication | Publication | Design | Dosing Sessions | Psilocybin Doses | Comparator | Psychological Support | N Randomized or Enrolled | Duration of Follow-Up | N Completed Study | Blinding Assessment and Success | Summary of Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Obsessive-compulsive disorder | Moreno et al., 2006 (34) | Open-label trial | 4 dosing sessions, 1 week apart | Very low (0.025 mg/kg), low (0.1 mg/kg), medium (0.2 mg/kg), high (0.3 mg/kg) | None | Prep: screening and day before; dosing: music and eyeshades; after: debrief at unspecified point | N=9 (7 male, 2 female); ages 26–62 | 24 hours after each dose | N=6 received all four doses | N/A | Main effect of time on Y-BOCS scores; all scores decreased from baseline to post-ingestion assessment; reduction in Y-BOCS scores ranged from 23% to 100% |
| Anxiety or depression due to cancer | Grob et al., 2011 (22) | Within-subject, double-blind, placebo-controlled crossover RCT | 2 dosing sessions, a few weeks apart | 0.2 mg/kg | 250 mg niacin | Prep: unspecified number of sessions; dosing: music and eyeshades; after: debrief at end of session | N=12 (1 male, 11 female); ages 36–58 | 6 months | N=8 at 6 mo., N=11 at 4 mo., N=12 at 3 mo | Not formally assessed, but drug order noted to be apparent to both participants and investigators | 30% reduction in BDI at 1 month (p=0.05); became statistically significant at 6-month follow-up (p=0.03); trait anxiety showed decrease during follow-up (p’s <0.03) |
| Tobacco dependence | Johnson et al., 2014 (20); Johnson et al., 2017 (42) | Open-label trial | 3 dosing sessions, 2–6 weeks apart; began with moderate dose, proceeded to high doses in 2nd and 3rd dosing sessions if participant could tolerate | Moderate (20 mg/70 kg), high (30 mg/70 kg) | None | Prep: 4 weekly CBT sessions with 2–3 therapists; dosing: music and eyeshades, guided imagery at end of first dosing; after: weekly support visits between dosing sessions | N=15 (10 male, 5 female) | 6 months | N=12 completed all dosing sessions | N/A | 12 of 15 participants were nicotine abstinent at 6-month follow-up; 11 of the 12 reported quitting on the target quit date and were verified as abstinent by urine and breath testing at all subsequent assessments during intervention period |
| Alcohol dependence | Bogenschutz et al., 2015 (19) | Open-label trial | 2 dosing sessions, 4 weeks apart; began with moderate dose, proceeded to high dose in 2nd session if participant could tolerate and did not have complete mystical experience with lower dose | Moderate (21 mg/70 kg), high (28 mg/70 kg) | None | 7 MET sessions, three preparation sessions, and two integration sessions; prep: 4 sessions with two or three therapists; dosing: music and eyeshades; after: 4 sessions between 1st and 2nd dose, and 4 after 2nd dose | N=10 (6 male, 4 female); ages 25–62 | 36 weeks | N=10 had one dose, N=7 had two doses, N=9 completed follow-up measures | N/A | Percent drinking days and percent heavy drinking days decreased during weeks 5–12 (after psilocybin) relative to baseline and relative to weeks 1–4 (MET/preparation sessions prior to psilocybin) |
| Anxiety or depression due to cancer | Griffiths et al., 2016 (23) | Within-subject, double-blind, placebo-controlled crossover RCT | 2 dosing sessions, ∼5 weeks between | 22 or 30 mg/70 kg | 1 mg or 3 mg/70 kg psilocybin | Prep: 2 or more sessions (mean of ∼3 for ∼8 hours total); dosing: music and eyeshades; after: 2+ sessions between 1st and 2nd dosing session (mean of ∼3 for ∼3 hours) and 2+ sessions between 2nd dose and 6-month follow-up (mean of ∼2.5 for ∼2.4 hours) | N=56 (26 male, 25 female); mean age, ∼56 years | 6 months | N=51 had one dose, N=49 had two doses, N=46 completed 6-mo. follow-up | Not assessed in participants, but session monitors could consistently distinguish between doses | Response rates on HAM-D and HAM-A were 75%–83% after dosing session 2; remission rates were 42%–68%; at 6-month follow-up, response rates were 77%–83%, and remission rates were 50%–71% |
| Anxiety or depression due to cancer | Ross et al., 2016 (24); Agin-Liebes et al., 2020 (25) | Within-subject, double-blind, placebo-controlled crossover RCT | 2 dosing sessions, ∼7 weeks between | 21 mg/70 kg | 250 mg niacin | Prep: three 2-hour sessions with therapist dyad over 2–4 weeks; dosing: music and eyeshades; after: three 2-hour sessions with dyad starting day after dosing | N=31 (11 male, 18 female); ages 22–75, mean age, ∼56 years | 3–4 years | N=29 had one dose, N=26 had two doses, N=23 completed 6-mo. follow-up, N=16 completed long-term follow-up (3–4 yrs.) | Not assessed in participants, but session monitors could consistently distinguish between drugs | Larger reductions in anxiety and depressive symptoms prior to crossover point for psilocybin versus niacin (all p’s <0.05); typically manifested the day following the dosing session and were sustained up to 7 weeks post-dosing; large effect sizes across all measures and time points (0.8 < d < 1.69); at long-term follow-up, response rates were 57%–79% across measures |
| Treatment-resistant MDD | Carhart-Harris et al., 2016 (12); Carhart-Harris et al., 2018 (17) | Open-label trial | 2 dosing sessions, 7 days apart; low dose in first dosing session, treatment dose in second | Low dose (10 mg), treatment dose (25 mg) | None | Prep: 4 hours on a single visit with two psychiatrists; dosing: music and eyeshades; after: phone call 1 day after low dose; in-person therapy 1 day and 1 week after second treatment dose | N=12 in 2016 paper (6 male, 6 female); N=20 in 2018 paper (14 male, 6 female); ages 30–64 | 6 months | N=12 completed in 2016 paper; N=19 completed all measures | N/A | Mean self-reported intensity of psilocybin effects was 0.51 for the 10-mg dose and 0.75 for the 25-mg dose; psilocybin was well tolerated with no serious or severe adverse events; QIDS-SR reduced at all time points; maximal effect 2 weeks after high dose |
| MDD | Davis et al., 2021 (13); Gukasyan et al., 2022 (41) | Double-blind, waiting-list-controlled parallel-arm RCT | 2 dosing sessions, 1–3 weeks apart | Moderately high (20 mg/70 kg), high (30 mg/70 kg) | Waiting list | Two facilitators; prep: 8 hours over 2 weeks (2 sessions, about 1 week apart); dosing: music and eyeshades; after: 1 session (∼2 hours) 3 days after first dosing; a second session (∼2 hours) 3 days after second dosing session | N=27; N=15 to immediate treatment, N=12 to waiting list (16 female, 11 male); mean age, 39.8 years | 1 year | N=26 received one dose, N=24 received two doses, N=24 completed all measures | N/A | Reduction in HAM-D score for immediate treatment versus waiting list; large effect sizes at 5 and 8 weeks; across both arms, 17 responders at weeks 5 and 8; across both arms, 14 remitters at week 5 and 13 at week 8; rapid reduction in QIDS-SR scores starting 1 day after first dosing session; benefits largely maintained at 3, 6, and 12 months |
| Demoralization in long-term AIDS survivors | Anderson et al., 2020 (39) | Open-label trial | 1 dosing session | 21 mg/70 kg for cohort 1, 25.2 mg/70 kg for cohorts 2 and 3 | None | Two therapists; prep: one 90-min. individual session, 2 weeks of twice-weekly 90-min. group therapy sessions; dosing: music and eyeshades; after: 2-hour individual therapy with at least one therapist the following day, then additional twice-weekly 90-min. group therapy sessions for 2–3 weeks | N=18, 3 cohorts of 6 participants each (all male); ages 50–66 | 3 months | N=18 received one dose, N=17 completed treatment, N=18 completed follow-up assessments | N/A | Rates of recruitment and retention high (95%); intervention well-tolerated; reduction in Demoralization Scale–II score from baseline to end of treatment and at 3-month follow-up; similar improvements in other outcomes except STAI |
| MDD | Carhart-Harris et al., 2021 (14) | Double-blind, placebo-controlled parallel-arm RCT | 2 dosing sessions, 3 weeks apart | 2 active doses (25 mg) plus daily placebo | 2 inactive doses of psilocybin (1 mg) plus escitalopram 10–20 mg/day | Two facilitators; prep: 1 session lasting ∼3 hours prior to first dose, and another lasting ∼1 hour prior to second dose; dosing: music and eyeshades; after: 3 debriefing sessions after each dose, starting 1 week after each dose and occurring over 3 weeks | N=59; N=30 to 25 mg psilocybin + daily placebo, N=29 to 1 mg psilocybin + 10–20 mg daily escitalopram (20 female, 39 male); mean age, 43.3 years in psilocybin arm, 39.1 years in escitalopram arm | 6 weeks | N=24 completed escitalopram protocol, N=27 completed psilocybin protocol | Not assessed | QIDS-SR change from baseline to 6 weeks did not differ between psilocybin and escitalopram arms; all secondary outcomes favored psilocybin, but statistical significance not inferred |
| Alcohol dependence | Bogenschutz et al., 2022 (21) | Double-blind, placebo-controlled, parallel-arm multi-site RCT | 2 dosing sessions, 4 weeks apart; began with moderate dose, proceeded to high dose in 2nd session if participant could tolerate it and agreed to increase; second dose was 40 mg/70 kg if participant did not have complete mystical experience with lower dose; otherwise it was 30 mg/70 kg | Moderate 1st dose (25 mg/70 kg), high 2nd dose (30 mg/70 kg or 40 mg/70 kg) | Diphenhydramine, 50 mg (1st dose), 100 mg (2nd dose) | META (motivational enhancement and taking action); prep: 4 sessions with 2 therapists; dosing: music and eyeshades; after: 4 sessions between first and second dose, and four after second dose | N=95; N=49 to psilocybin arm, N=46 to diphenhydramine arm (42 female, 53 male); mean age, 46 years | 36 weeks | N=93 received one dose, N=78 received two doses, N=88 completed 8-mo. follow-up assessment | 93.6% of participants guessed correctly after 1st dose, 94.7% of participants guessed correctly after 2nd dose; therapists guessed correctly 92.4% of the time after 1st dose and 97.4% of the time after 2nd dose | Percent heavy drinking days lower in psilocybin versus diphenhydramine group; psilocybin group more likely to report no heavy drinking days and reduction in WHO risk level |
| Treatment-resistant MDD | Goodwin et al., 2022 (27) | Double-blind parallel-arm RCT | 1 dosing session | 25 mg or 10 mg | 1 mg | Lead and assistant therapist for each patient; prep: 3 sessions, with final session 1 day before dosing; dosing: music and eyeshades; after: 2 sessions, one the day after dosing with both therapists, and a second 1 week later with the lead therapist | N=233; N=79 to 25 mg, N=75 to 10 mg, N=79 to 1 mg (121 female, 112 male); mean age, 39.8 years | 12 weeks | N=233 received dose, N=210 completed full protocol | Not assessed | Difference on MADRS between 25-mg and 1-mg arms at primary endpoint, with 25 mg being superior to 1 mg; no difference on MADRS between 10-mg and 1-mg arms at primary endpoint; other statistical tests not conducted due to hierarchical testing procedure |
| Treatment-resistant MDD (all participants maintained on SSRI monotherapy) | Goodwin et al., 2023 (28) | Open-label trial | 1 dosing session | 25 mg | None | Prep: 3 sessions, with final session 1 day before dosing; dosing: music and eyeshades; after: 2 sessions, one the day after dosing, and a second a week later | N=19 (13 female, 6 male); mean age, 42.2 years | 3 weeks | N=19 of 24 enrolled participants underwent dosing | N/A | Mean change in MADRS from baseline to week 3, −14.9 (statistically significant); response on MADRS (>50% reduction from baseline) observed in 8 participants (42.1%) at week 3; responders were also all remitters (MADRS score <10) at week 3 |
| MDD | von Rotz et al., 2023 (26) | Double-blind parallel-arm RCT | 1 dosing session | 0.215 mg/kg (considered a moderate dose) | Inactive placebo | A single therapist; prep: 2 hour-long sessions, with final session 1 day before dosing; dosing: music (no mention of eyeshades); after: 3 hour-long sessions, the first the day after dosing, the second 1 week later, and the third 2 weeks later | N=52; N=26 to psilocybin arm, N=26 to placebo arm (33 female, 19 male); mean age, 37.6 years in psilocybin arm, 35.9 years in placebo arm | 14 days | N=52 received dose; N=49 completed study | Not assessed | Significant difference for change in MADRS and BDI between arms; average between-arm differences were −13 on MADRS and −10.5 on BDI for psilocybin versus placebo; 58% response rate on MADRS and 54% on BDI in psilocybin arm; 54% remission rate on MADRS and 46% on BDI in psilocybin arm; mean differences between arms on outcomes largest 2 days after dosing |
| Depression due to cancer | Lewis et al., 2023 (30) | Open-label trial | 1 dosing session | 25 mg | None | Group psychotherapy format, 1:1 provider to therapist ratio; each cohort involved 4 patients, 4 therapists, 1 lead therapist, and 1 study coordinator (10 in total); prep: three 120-min. group preparation sessions over a 1-week period; dosing: 6–8 hours in a group administration setting with private “bays” for each participant, music provided over speakers; integration: three 120-min. sessions over the 2 weeks following dosing | N=12 (8 female, 4 male); ages 30–71, mean age, 48.2 years | 26 weeks | N=12 completed treatment | N/A | Primary HAM-D outcome decreased from baseline to 2-week follow-up primary endpoint and the 26-week long-term endpoint; clinically substantial change in 8 participants (reductions of 7–12 points), and clinically significant change in 3 participants (4–6 points) |
| Anorexia nervosa | Peck et al., 2023 (35) | Open-label trial | 1 dosing session | 25 mg | None | Prep: two sessions within 10 days of dosing day with a single lead therapist; dosing: two psychologists present; music and eyeshades; integration: two integration sessions, 1 day and 1 week after dosing | N=10 | 3 months | N=10 received 25 mg psilocybin | N/A | No serious adverse events observed; no clinically significant changes in vital signs or ECG; 2 participants developed hypoglycemia, which resolved within 24 hours; no increases in suicidal ideation and no suicidal behaviors reported at post-dosing follow-up; EDE subscale of weight concerns decreased at 1 month and 3-month follow-up; EDE subscale of shape concerns decreased at 1 month but not 3 months; EDE eating concerns and dietary restraint subscale changes not significant at 1 or 3 months |
| MDD | Raison et al., 2023 (18) | Double-blind parallel-arm RCT | 1 dosing session | 25 mg | 100 mg niacin | Prep: 6–8 hours over multiple days with 2 facilitators, with at least 1 session in-person; dosing: music and eyeshades, 7–10 hours in length, two facilitators present; integration: 3 sessions, 1 the day following dosing, 1 a week later, and another 2 weeks after dosing | N=104; N=51 to psilocybin arm, N=53 to niacin arm (52 male, 52 female); mean age, 40.4 years in psilocybin arm, 41.8 years in niacin arm | 6 weeks | N=104 randomized, N=103 received assigned dose, N=92 completed all assessments | Not assessed | Greater reductions on primary outcome (MADRS) from baseline to day 43 and from baseline to day 8 for psilocybin versus niacin; more participants receiving psilocybin versus niacin displayed sustained depressive symptom response; mean change in disability score (SDS) from baseline to day 43 greater in the psilocybin versus niacin group; results of per protocol analysis largely similar, except difference in sustained remission became significantly different between psilocybin and niacin arms |
| Body dysmorphic disorder | Schneier et al., 2023 (36) | Open-label trial | 1 dosing session | 25 mg | None | Prep: 4 weekly preparatory sessions with two psychotherapists; dosing: 7–8 hours with both therapists; music and eyeshades; integration: 2 sessions, 1 day and 1 week after dosing | N=12 (4 male, 8 female) | 12 weeks | N=12 received dose and completed study, N=1 started an antidepressant at week 4 | N/A | Significant decrease on BDD-YBOCS from baseline to 12 weeks; 7 participants were responders at week 12, and 4 were sustained remitters |
| Depression due to cancer | Agrawal et al., 2023 (32); Shnayder et al., 2023 (31) | Open-label trial | 1 dosing session | 25 mg | None | Mixed individual/group psychotherapy format in cohorts of 3–4 patients; preparation: 2-hour individual therapy session with a single therapist, followed by 75-min. group therapy and 45-min. individual therapy the day before dosing; dosing: individual dosing; music and eyeshades; integration: 75-min. group therapy session and 45-min. individual therapy session the day after dosing, followed by the same format 1 week later | N=30 (21 female, 9 male); ages 30–78, mean age, 56.1 years | 8 weeks | N=30 completed study | N/A | Reduction in MADRS scores from baseline to 8 weeks; sustained response in 24 patients, with 15 patients demonstrating remission on MADRS; improvements on all three factors of NIH-HEALS beginning the day after dosing and lasting for 8 weeks |
| MDD | Sloshower et al., 2023 (29) | Within-subject, fixed-order, placebo-controlled trial | 2 dosing sessions, 4 weeks apart; placebo dose always preceded psilocybin dose | 21 mg/70 kg | Inactive placebo | Individual therapy; participants each assigned a study therapist and psychiatrist; prep: 2-hr session the day before each dosing session; dosing: therapist and psychiatrist present for 6 hours; music and eyeshades; integration: two 1-hour sessions 1 day and 1 week after each dosing session | N=22 (13 female, 6 male), ages 20–61, mean age, 42.79 years | 16 weeks | N=19 completed one dosing session, N=15 completed both dosing sessions | After placebo, 15 of 19 (78.9%) correctly guessed placebo; after psilocybin, 12 of 15 (80%) correctly guessed the drug and dose | Significant effect of time, but no significant time-by-drug interaction, on primary outcome (HAM-D) as well as secondary outcomes (HAM-A and QIDS-SR) |
| AUD | Heinzerling et al., 2023 (33) | Pilot open-label trial of two doses of 25 mg psilocybin with a randomized setting manipulation (visual healing, a nature-themed video, vs. standard dosing setting) | 2 dosing sessions, 4 weeks apart | 25 mg (visual healing vs. standard dosing setting randomized at first dosing session) | No drug comparator | Individual therapy; participants each assigned a study therapist and physician; prep: two sessions, 1 week apart; second session ended with either visual healing or body scan meditation; dosing: reclining on couch and either watching visual healing versus eyeshades/music (randomized in first session; participant choice in second session); integration: 3 sessions after each dose, the first the day after dosing, the other two once weekly | N=20 (12 female, 8 male); mean age, 46.9 years in visual healing, 51.0 years in standard dosing setting | 14 weeks | N=20 completed first dosing session, N=19 completed both dosing sessions and full study | N/A | After first dosing session, 1 participant relapsed into alcohol use and required inpatient treatment; a majority of participants agreed or strongly agreed that visual healing helped them feel relaxed and prepared for the psychedelic session and to feel more connected to nature; alcohol use decreased on average for all participants, with no significant differences between visual healing versus standard dosing procedure groups; peak increase in blood pressure following psilocybin dosing was significantly less (both systolic and diastolic) for those randomized to visual healing versus standard dosing procedures |
Evidence of Efficacy
Dosing Considerations
Duration of Benefits
Factors Affecting Internal Validity
Factors Affecting Generalizability
Adverse Events and Risk-Benefit Profile
Psychological Treatment Components
Predictors of Therapeutic Response
Discussion
Mechanism(s) of Change
Recommendations
Establish Optimal Dosing
Assess Treatment Expectancy and Improve Blinding
Increase Sample Size and Diversity for Enhanced Generalizability
Investigate Moderators and Mediators of Therapeutic Response
Utilize Additional Comparators to Dismantle Effects
Investigate Effects of Concomitant Medications
Assess and Control for Prior Psychedelic Use
Conduct Comparative Efficacy Trials
Provide Accurate Education to Interested Patients
Conclusions
Footnote
Supplementary Material
- View/Download
- 461.75 KB
- Download
- 494.54 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).