This issue features a timely and important article by Gustafson et al. (
1), noteworthy for the meaningful questions it addresses, the practical design, the comprehensive analyses, and the candid presentation of the findings.
The findings are very important from both clinical and public health perspectives. In summary, this large randomized controlled trial evaluated the acceptability and effectiveness (opioid abstinence) of a smartphone-based patient support app (A-CHESS) among three groups of opioid-dependent patients receiving buprenorphine, methadone, or naltrexone. Half of the patients in each medication group received normal medication adjustments and traditional counseling, and the A-CHESS group received essentially the same routine care plus the phone app. Acceptability was quite high across all medication groups and throughout the 2-year duration of the trial. Past-month opioid abstinence (verified by urine screens and structured verbal report) was measured at treatment entry and every 4 months thereafter for 2 years. While the primary outcome analyses showed no significant added effect of the A-CHESS app on the abstinence criterion, participants in the A-CHESS group did show significantly greater counseling attendance during treatment and decreased emergency department and urgent care use. Among the most interesting findings was that patients in the methadone and buprenorphine groups (there were too few for analysis in the naltrexone group) who reported low levels of withdrawal and craving did show very significant abstinence-enhancing benefits from the A-CHESS app. While these findings are admittedly complicated, I drew three conclusions from this work that I think have particular relevance to this still developing area of practical clinical research.
Medications Are Very Effective in the Treatment of Opioid Use Disorder
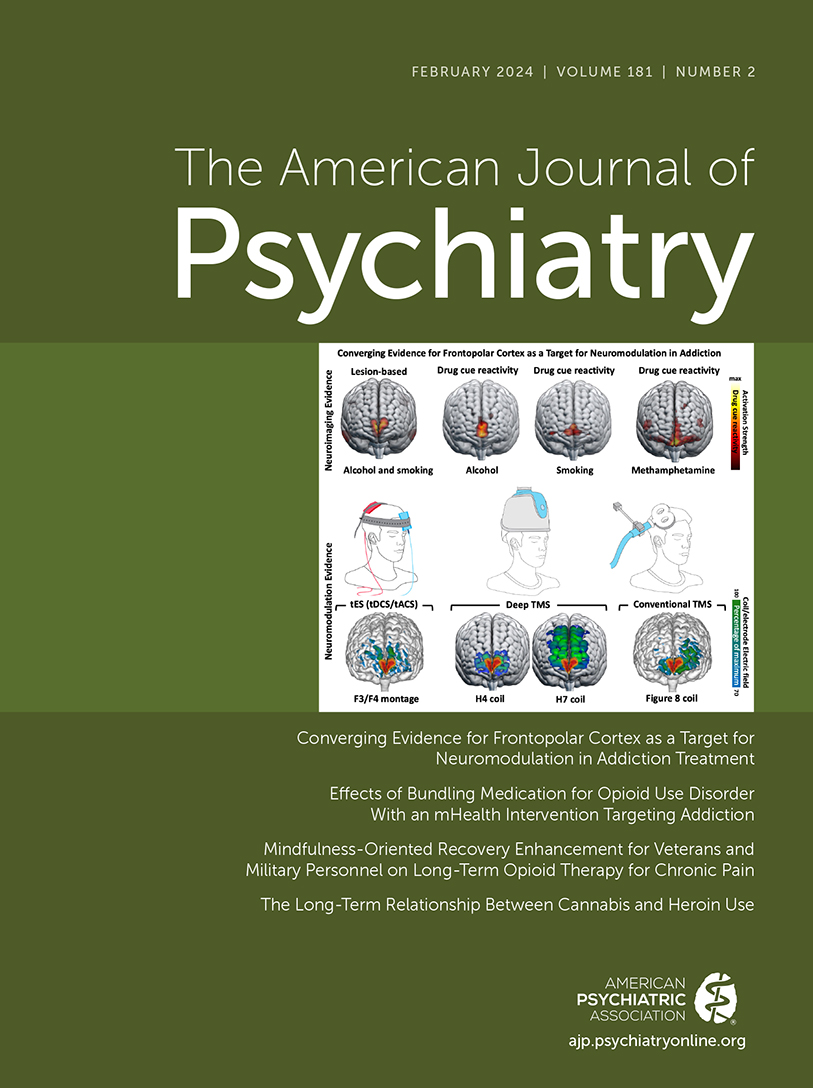
Unfortunately, even after decades of research and clinical work with literally millions of patients with opioid use disorder (OUD), this statement still requires emphasis. Although not the central point of the article, the data from Figures 2 and 3 illustrate dramatic, clinically significant, and enduring improvements in rates of opioid abstinence: 80%–90% by 6 months and sustained through 2 years. Given the deadly nature of OUD and the broad public skepticism that “nothing works,” these findings alone have great public health significance. Moreover, the outcome criterion selected by the authors (abstinence) was a particularly stringent choice. My suspicion is that improvements in “frequency of use in past 30 days” might have shown even stronger results.
Despite these remarkable findings, all three of the tested medications (especially naltrexone) are still a tough sell to many clinicians, patients, and policy makers, usually because of one overarching question: “How long do they have to remain on the medication?” For decades, clinicians have given the same accurate but unsatisfying homily: “We that find patients who remain on the medication longer do better.” I think Figures 2 and 3 in the Gustafson et al. article provide a far more engaging and constructive answer: patients who wish to stop their dependence on opioids and enjoy a healthy medication-free life should first do so while medicated and in treatment. The data from this and many other studies show that abstinence and other important parts of recovery are very likely to be achieved while taking any of the maintenance medications studied here. Put conversely, patients who can’t achieve these goals with clinical care and medication are not likely to improve their chances by stopping treatment. I consider this “medication-assisted recovery” to be a necessary first step toward traditional recovery.
Smartphone-Based Apps Can Now Engage Patients and Add Value to Addiction Treatments
I have been involved in one way or another with development and testing of at least 30 “evidence-based” support apps in the treatment of addiction. None worked—very few of the patients were willing to use any of the apps, even if paid to do so. So I was very heartened by the present findings that 91% of participants used A-CHESS in the first month, 73% at 6 months, and 59% at 1 year. My first thought was that the A-CHESS app was merely used by patients to report outcomes—for which they were reimbursed. Not at all. Study participants used A-CHESS 32% of days in the first year and 18% of days in the second year. In comparison, that’s about how often I use each of my banking, PubMed, and travel assistance apps. These encouraging data suggest that these investigators have begun to crack the important puzzle of how to make social support services engaging—in my view, a fundamental precursor to assessing effectiveness. Yes, it is true that A-CHESS patients were reimbursed for using the app to report monthly status data, but so what? I think the kind of modest incentives used in the study were potentially well worth it if they are part of a clinical package that has such public health potential.
There Are Still Many Things We Do Not Understand About the Recovery Process
My friend and colleague William White, who writes extensively about recovery, has long argued that thanks to NIH, we have a well-developed and ever-advancing “science of addiction.” But he laments that comparatively little effort has been put toward a “science of recovery.” I raise this issue because many of the investigators’ a priori hypotheses regarding mediators and moderators of outcome in this study failed to be supported. Still other statistically significant findings are very difficult (at least for me) to understand. I am not trying to second-guess the investigators’ hypotheses. Rather, I am pointing out how complex the course of recovery can be and how little we understand it.
For example, like the investigators, I too thought the A-CHESS app would have particular benefits for those who had greater depression, loneliness, and poor social support. But that was not the case. Understanding why those sensible ideas did not pan out is the next important step in this line of research. Is it because those patients with poor medication adherence and rapid relapse were too affected to engage with the app? Is it possible that those support elements within the app were just not as engaging or potent for their intended target symptoms? At least by finding that the target population seems to like and use the app, it will next be important to evaluate and augment the potency and effectiveness of the individual components within that app.
Even more puzzling to me is the remarkable finding that the app was most effective in cases where there were few or no withdrawal symptoms. I actually thought the opposite—that the app might provide special assistance and control in helping patients deal with those symptoms. One possibility is tautological: patients with more withdrawal were most likely to be using and thus not abstinent. My after-the-fact clinical speculation is that the app may be most—or perhaps only—effective once withdrawal and craving are effectively managed with a properly dosed medication. In other words, “job one” for any or all of these medications is sustained control of withdrawal and craving. If even partly true, it may be that the app is best administered only after a significant period of physiological stabilization.
So I found the Gustafson et al. study valuable simply for the two main contributions: definitively establishing the clinical value of medications in treating OUD, and the creation and refinement of what may be the first truly engaging smartphone-based app for use in OUD treatment and recovery. But the study has also taken the first steps toward a better understanding of what specific services and supports properly medicated and stabilized OUD patients want and need, and how to deliver those services remotely to enhance recovery. I look forward to what comes next in this important line of research.