Access to reliable contraceptive methods may have health-related, personal, and societal effects that go beyond family planning and prevention of unwanted or unintended pregnancies. The United Nations and World Health Organization have long considered family planning contraceptive counseling as a human right, an essential step toward gender equality and women’s bodily autonomy (
1). Effective contraception has been clearly linked to more educational and socioeconomic opportunities for young women; it increases their chances to pursue their educational goals, which could result in fewer financial stressors and improved quality of life (
2). Moreover, by drastically reducing the occurrence of unintended pregnancies, women could more freely enjoy their sexual experiences, which would have a positive impact on their overall well-being (
3).
Approximately 900 million women worldwide utilize one or more contraceptive methods, with preferred methods varying significantly by country or region (
4). While barrier contraceptive methods (particularly male condoms) remain widely used, hormone-based contraception is adopted by more than 40% of women of reproductive age. Oral contraceptive pills are used by over 20% of women in 27 countries worldwide, with the highest prevalence seen in European countries. Long-acting hormonal strategies such as implants, depot injections, and intrauterine devices (IUDs) eliminate the need for daily medication use and may be a more convenient option for many individuals. The number of women using long-acting strategies such as implants and IUDs has increased significantly over the past few decades, with estimates that 159 million women have IUDs and 23 million have implants, representing 17% and 2% of reproductive-age women, respectively. Curiously, there are significant differences between the adoption of IUDs as the preferred method among women who are married or living together with a partner (20%) versus those who are not married or not in a union (only 6%).
There are several formulations (e.g., estrogens and/or progestins) and numerous routes of administration (e.g., oral, transdermal, injectables, implants, IUDs) to be considered when choosing a hormone-based contraceptive method. Oral contraceptives must be taken daily and consist essentially of combined oral contraceptives or progestin-only contraceptives. Combined oral contraceptives usually contain ethinylestradiol, a synthetic preparation that is analogous to the endogenous estradiol, along with one of the various forms of progestins that mimic the endogenous progesterone—for example, norethisterone, levonorgestrel, or drospirenone. Because of the various progestins used, combined oral contraceptives may have distinct androgenic, estrogenic, and antiandrogenic properties, which may not only affect their tolerability but also determine their potential applications in various medical conditions. Progestin-only contraceptives are often taken continuously and may contain different forms of progestins that are analogous to endogenous progesterone, such as norethindrone and levonorgestrel (
5). It is important to note that the distinct molecular structures of progestins will lead to distinct pharmacodynamic and pharmacokinetic properties and contribute to different tolerability profiles.
Injectables consist primarily of medroxyprogesterone acetate, with subcutaneous or intramuscular administration; they last for 3 months but often lead to side effects that limit their acceptability. Vaginal rings release combinations of estrogen and progestin into the systemic circulation, through the vaginal epithelium, and usually have good tolerability and adherence. IUDs were first introduced to the market as copper T-shaped devices, designed to minimize device expulsion from the uterus; they were often associated with a high incidence of menorrhagia, which adversely affects long-term adherence. Currently, IUDs are hormonal preparations that may last for 3–6 years. They are made of a polyethylene T-frame and contain a cylindrical drug reservoir (
6).
The administration of any hormone-based treatment or contraceptive method should take into consideration that some women may be particularly sensitive to the development of psychological symptoms—particularly mood changes and anxiety—when exposed to exogenous hormone preparations. Preclinical, clinical, and epidemiological data also support the notion of “windows of vulnerability” for the emergence of mood and anxiety symptoms across the reproductive life cycle that could be triggered by exposure to endogenous hormone fluctuations, including symptoms of depression and anxiety during postpartum periods, premenstrually, and across the menopause transition (
7,
8).
In some cases, tailored hormone-based interventions have proven to be effective in reducing this vulnerability by mitigating the negative impacts of changes in the endogenous hormone milieu or by simply eliminating these changes (
9). Combined contraceptives are, for example, recommended for the management of premenstrual dysphoric disorder (
10,
11), with some positive results also in reducing premenstrual breakthroughs of depression (i.e., premenstrual exacerbation of depressive symptoms) (
12).
Studies examining the potential effects of contraceptive preparations on mental health have shown mixed results. A recent systematic review (
13) examined the effects of contraceptive methods, including oral contraceptives, long-acting methods (e.g., intrauterine devices, implants), and condoms, on the mental health status of women across 21 randomized controlled trials and 20 cohort studies. The review included women during reproductive years (ages 14–49), with a small percentage of postmenopausal women included in the analyses. In nine studies of women with a previous history of mental disorders, the use of oral contraceptives showed a slight protective effect against the occurrence of depression. In contrast, three studies that included women without previous mental health issues revealed no protective effect against depression with the use of oral contraceptives compared to nonusers. Overall, the risk ratio for depression was slightly higher (1.13, 95% CI=1.04–1.24) among all hormonal contraceptive users versus nonusers; within the hormone-based subgroup, risk for depression was higher among users of implants, progesterone pills, patches/rings, and hormonal IUDs.
In another recent systematic review and meta-analysis (
14), the relationship between oral contraceptive use and symptoms of mental disorders was investigated in a subset of studies (N=15), with no reports of significant associations. The authors further examined potential differences based on age at onset of oral contraceptive use. In four studies, the use of oral contraceptives in adolescence and early adulthood was associated with the development of depressive symptoms or other symptoms of mental disorders—although no careful psychiatric history had been obtained prior to onset of oral contraceptive use. One of the studies, however, found a slightly protective effect of oral contraceptives, that is, a reduced risk for depressive symptoms with longer duration of oral contraceptive use—up to 5 years of usage (
15). We had observed a similar protective effect against depression associated with longer exposure to oral contraceptives when we examined a large cohort of premenopausal women (ages 42–52 at study entry) (
16). In that study, longer use of oral contraceptives during premenopausal years was associated with a decreased risk for depressive symptoms during the menopause transition.
Altogether, there is some evidence to support modest protective effects of hormone-based contraceptives when used by women with previous mental disorders, and/or by women with history of dysphoric mood symptoms associated with menstrual cycle changes. Age seems to be a modifying factor for the effects of oral contraceptives, with a decreasing risk for depressive symptoms observed among older oral contraceptive users; conversely, there could be a heightened vulnerability to developing depressive symptoms among younger oral contraceptive users (adolescents, young adults). Lastly, emerging evidence suggests a higher risk for depressive symptoms with the adoption of certain hormone preparations or routes compared to other methods—particularly with the use of implants, progestogen-only pills, and hormonal IUDs.
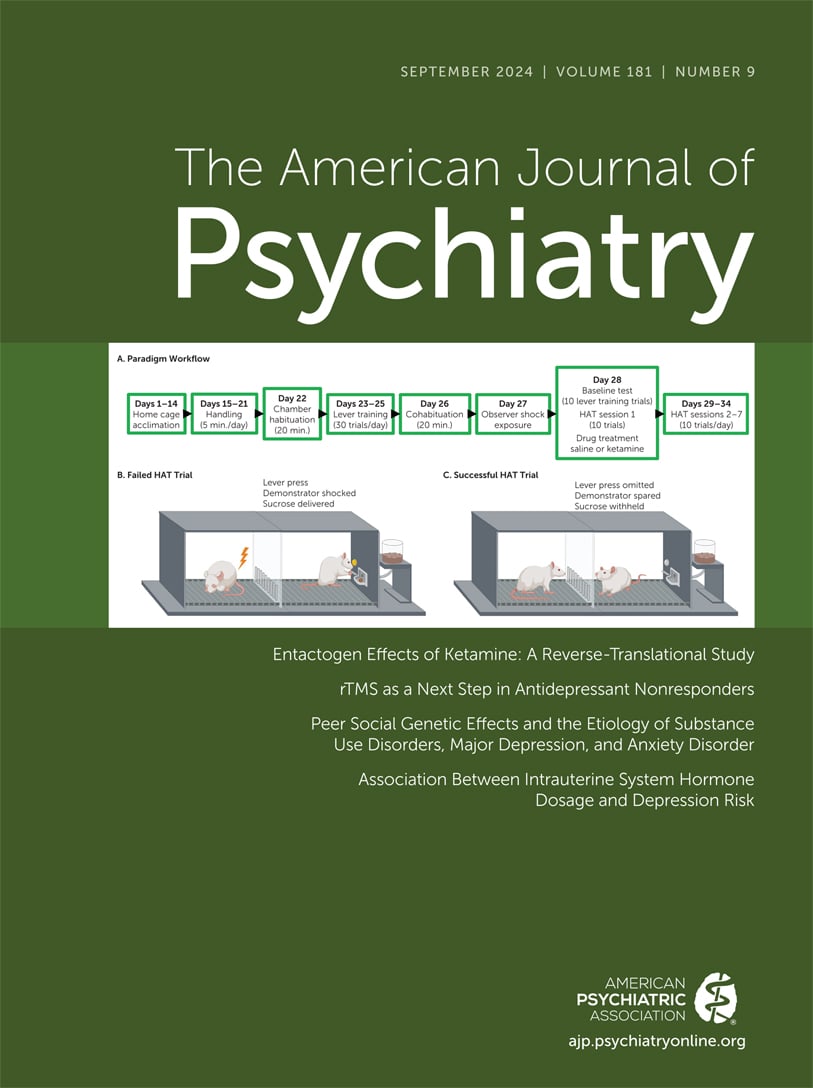
In this issue of the
Journal, a study reported by Larsen et al. (
17) aimed to fill a gap in our understanding of the association between hormonal IUDs or intrauterine systems (IUSs) and the occurrence of depression. More specifically, the authors wanted to explore the effects of levonorgestrel-releasing intrauterine systems (LNG-IUSs) among first-time users and further differentiate these effects based on dosing: low, medium, and high dosages (14 μg/day, 17.5μg/day, and 21 μg/day, respectively). Building on previous evidence that suggested an increased occurrence of depression among women using progestin-only contraceptives and levonorgestrel-releasing IUDs, the authors hypothesized that the risk for depression with LNG-IUS use would increase in a dose-dependent fashion. They utilized data from a Danish registry of almost 150,000 first-time LNG-IUS users. The population of interest consisted of individuals who had never been diagnosed with depression or received prescriptions for psychotropic medications before. The outcome of interest was the incidence of depression within 12 months of initiating the use of an LNG-IUS, with depression being defined as incident use of antidepressants or a diagnosis of depression by a psychiatric service (inpatient or outpatient).
The study had several strengths, as the investigators were quite diligent in reducing potential confounders, such as prior use of psychotropic medications or formal psychiatric diagnosis. Also, they considered other conditions that are known for skewing use of IUSs as the preferred contraceptive method, including history of menorrhagia, leiomyoma, polycystic ovary syndrome, dysmenorrhea, and endometriosis. As part of their sensitivity analyses, the authors investigated those who were nulliparous and first-time users under age 30; by doing so, they aimed to mitigate the potentially confounding effects of high-dose LNG-IUSs being more often prescribed for women age 30 and older for non-contraceptive reasons, such as the management of irregular bleeding and for endometrial protection for those receiving estrogen-based menopause treatments.
Larsen et al. found an increased incidence of depression within 12 months of LNG-IUS use, with a progressively higher risk associated with dosage. Low-dose, medium-dose, and high-dose users had adjusted absolute risks of 1.21% (95% CI=1.06–1.36), 1.46% (95% CI=1.33–1.59), and 1.84% (95% CI=1.72–1.96), respectively; the absolute risk was small based on the number of diagnoses of depression in these three groups (279, 633, and 1,346, respectively). The authors argue that their findings, although modest in absolute numbers, reinforce the notion that progestin usage through IUSs (levonorgestrel) could be contributing to the emergence of depression, and that such susceptibility could be dose dependent.
To place these results in context, the annual incidence rate of medically treated depression in a Danish Registry sample of >2 million individuals (ages 15–44) was estimated to be 10.1 per 1,000 person-years (95% CI=10.0–10.2), which is equivalent to a mean annual incidence rate of 1.0%. The incidence was higher among females—12.8 per 1,000 person-years (95% CI=12.6–13.0), or an annual incidence rate of roughly 1.3% (
18). Recent studies also suggest that the occurrence of depression in the general Danish population could be significantly underestimated if based solely on register-based measures, which tend to identify only the most severe cases (
19). Thus, one could argue that the incidence of depression captured by Larsen et al. among first-time users of LNG-IUSs is only marginally higher when compared to the overall Danish population, perhaps with the exception of the incidence among users of the high-dose LNG-IUSs, which may be more significant.
It is also unclear whether the study included individuals who initiated LNG-IUSs after previous (unfavorable) reactions to oral contraceptives. Some could have experienced, for example, dysphoric states, anxiety, low mood, or irritability while on other oral formulations. If so, a poor tolerability to hormone formulations (in general) and the occurrence of mood symptoms triggered by other hormone preparations could have contributed to the decision to switch these individuals to an LNG-IUS. Hence, the incidence of depression within the first year that was attributed to LNG-IUS use could be partially explained by prior susceptibility and/or lingering mood effects caused by other hormone preparations.
There are some potential explanations for the small increase of incident depression with levonorgestrel in particular, including preclinical evidence of the effects of levonorgestrel on brain γ-aminobutyric acid receptor plasticity and anxiety-like behavior in rats (
20). A previous study (
21) had also suggested that levonorgestrel, when administered at dosages of 20 μg/day, could potentiate physiological responses to stress, enhancing a centrally mediated potentiation of hypothalamic-pituitary-adrenal axis reactivity, and a peripheral downregulation of adrenal cortex reactivity. The authors of that study speculated that these mechanisms could partially explain the predisposition of LNG-IUD users to develop stress, depressive symptoms, or anxiety.
Better awareness is needed regarding the potential emergence of mood symptoms and other psychological changes in response to either fluctuations of endogenous hormones or the administration of exogenous hormone preparations (oral contraceptives, IUDs, menopause hormone therapies). This should be part of the clinical assessment, discussions, and counseling involving general practitioners, gynecologists, and mental health professionals.
Counseling individuals on efficacy, tolerability, and potential risk factors for mood symptoms associated with hormone preparations—including LNG-IUSs—should help in making informed choices. Counseling on individualized risks requires a thorough psychiatric history with a particular focus on reproductive events and indications of a heightened sensitivity to hormone changes or hormone preparations.
A discussion about effectiveness, convenience, benefits, and possible adverse effects of LNG-IUSs should also include the likely timing of onset and duration of these symptoms should they occur (
22). One question that remains unanswered is whether these symptoms are potentially reversible after removal of the IUS, as opposed to their management though different strategies (pharmacological, behavioral) while keeping the IUS in place.
Evidence suggests that changes in mood with hormone-based contraceptive methods are most likely to emerge in the first few weeks or months of use. This is an important point for psychiatrists and other health professionals to keep in mind, particularly those who may not be routinely involved in discussions of contraception or be aware of recent changes in contraceptive methods used by their patients. A recent change in hormone contraceptives (new use, switch, discontinuation) could be a key factor contributing to destabilizing a patient undergoing psychiatric treatment. Recognizing and proactively addressing these complex interactions will lead to more effective, more holistic care for our patients.