Since the days of Ramón y Cajal, neuroscientists have been trying to understand and categorize how neurons are specialized, by form, function, and anatomy. Often, the more information we have, the smaller these individual categories can become. Indeed, years ago at a conference, a colleague was describing a very minute and specific population of neurons surrounding a subnucleus of a small brain region. I (Z.A.M.) remarked to him, “Are you talking about a total of four cells?”, to which he playfully admonished me for not appreciating what is to be gained by closely studying the intricacies of anatomy. I have often reflected on this conversation over the years since—after all, as whole-cell electrophysiologists, we often feel like every individual cell we record from is distinct, special, and unique in a myriad of ways. Anthropomorphizing the cells, we often attribute to them personalities and emotions as we try to coax them into submitting to our instrumentation. Yet still, we need to be able to group our cells into categories to generalize their function (e.g., is a cell glutamatergic/excitatory or GABAergic/inhibitory? Does it signal via a specific modulator?). These categorizations help us understand how that function may be perturbed in pathological states, and how these cellular categories may contribute to certain behavioral output. The advent of “modern neuroscience” tools has allowed for a multitude of ways of categorizing neurons, and those of us who work mostly in rodent models have used this to our advantage, expressing proteins and RNA products in selective populations that allow us to monitor, manipulate, and characterize our favorite cell populations based on their anatomical location and/or projections, and cellular phenotypes. As we are often reminded, however, our goals are not to cure anxiety, autism spectrum, or substance use disorders in rodents; therefore, our experimental design, models, and manipulations must have an eye toward what is known in primates, and especially humans. The latest results from the Schumann and Fox labs, reported in this issue by Kamboj et al. (
1), provide a wealth of new information on distinct amygdalar neuronal populations in the rhesus macaque and age-/stage-matched human subjects.
The amygdala is a critical hub of emotionality, and its dysregulation can contribute to a wide range of disorders, including neuropsychiatric disorders like anxiety, depression, and substance use disorders, as well as neurodevelopmental disorders like autism spectrum disorder (ASD). Efforts to identify effective therapeutics must focus on examining the different amygdalar subnuclei with a translational approach. Preclinical studies (mainly in rodent models) have been heavily focused on understanding how signaling and cellular functions in these cell types contribute to the behavioral outcomes characteristic of these disorders. Cell types are defined by the subnuclei they are located within, the cell class (neuron, microglia, astrocyte, etc.), and typically at least one other defining characteristic, such as developmental origin, neurotransmitter expression, neuropeptide expression, or a unique gene marker. Although the amygdala is generally well conserved across species, it is unclear whether the proportions of diverse cell types within and between subnuclei are conserved as well.
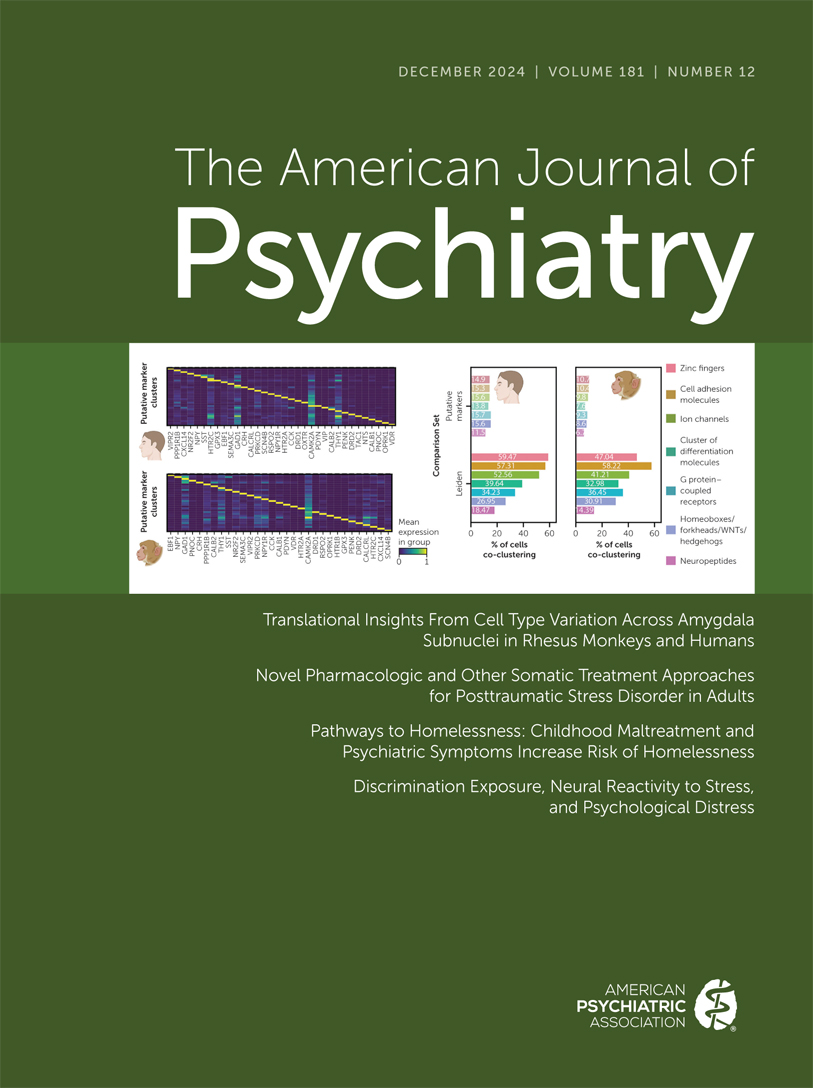
The study by Kamboj et al. utilizes single-nucleus RNA sequencing and a type of network analysis (Leiden clustering analysis) to identify clusters of cells based on a plethora of characteristics simultaneously, including but not limited to genes that differentiate cell class, developmental origin, neurotransmitter expression, and other gene markers. The authors examined the diversity of cell clusters across species and amygdalar subnuclei by performing separate analyses for human ventral lateral amygdala (vLA), human central amygdala (CeA), rhesus vLA, and rhesus CeA. These brain regions are interconnected and have been implicated in a host of functions, including the regulation of motivated behaviors and emotion (
2), where they both appear critical for mediating behaviors related to fear, pain, and reward. This makes understanding how the CeA and vLA develop and function in various human behavioral conditions critical for both diagnosis and potential treatments. Importantly, previous studies in primates and humans did not differentiate between CeA and LA in sequencing or analysis. While these two amygdala regions are close in proximity and communicate with each other, they contain very different groups of cells. Kamboj et al. discovered that the cell cluster composition was significantly different between amygdalar subnuclei in humans and, to a greater extent, in rhesus monkeys. For example, across both species, the authors demonstrated that GABAergic cells in the CeA are more likely to express markers indicating that the cells originated in the lateral ganglionic eminence (LGE). In contrast, GABAergic cells in the vLA are more likely to express genetic markers indicating that the cells originated in the medial ganglionic eminence (MGE). These data are consistent with a study in mice by Waclaw et al. (
3) that showed that putative GABAergic medium spiny neurons in the CeA express genetic markers indicating a developmental lineage specifically from the ventral LGE (
ISL1 and
DLX5/6) and local interneurons within the basolateral amygdala (BLA) are derived from the MGE and/or caudal ganglionic eminence. Different developmental lineages may make these distinct GABAergic populations more or less susceptible to environmental stressors and perturbations, as these ganglionic eminences have different developmental temporal windows (
4).
Kamboj et al. identified a cell cluster of putative intercalated cells (ITCs, a group of inhibitory interneurons that modulate the information flow through the amygdala via feedforward inhibition [
5]) that were derived from the LGE and expressed ITC markers such as
FOXP2,
TSHZ1,
MEIS2, and
PBX3. Moreover, this putative ITC cell cluster expressing
FOXP2 was enriched with a G protein–coupled receptor for neuropeptide FF (
NPFFR2). Similarly, in mice, ITCs surrounding the BLA and CeA originate specifically from the dorsal LGE with gene markers including
DLX5/6,
FOXP2,
MEIS2,
GSX2 (homeobox gene), and
SP8 (zinc-finger transcription factor), as well as significant µ-opioid receptor expression (
3). Importantly, the cell clustering approach used by Kamboj et al. illustrated that the putative ITC cluster that expresses
FOXP2 also expresses genes related to anxiety and depression. In rats, a model of alcohol dependence and withdrawal suppressed GABAergic inhibition from the lateral group of GABAergic ITCs onto BLA principal neurons (
6), suggesting that the putative ITC cell cluster identified by Kamboj et al. could be implicated in the development of alcohol dependence and alcohol withdrawal–induced anxiety as well. Furthermore, the medial groups of GABAergic ITCs are involved in fear conditioning and extinction in mice. Foot shock has been found to increase calcium activity in dorsomedial ITCs, and the amplitude of the calcium responses were positively correlated with the duration of freezing (
7). In contrast, chemogenetic Gi/o manipulation of the ventromedial ITCs impaired fear extinction, while chemogenetic Gq manipulation of ventromedial ITCs promoted fear extinction (
7).
Interestingly, Kamboj et al. found that expression of classic histopathologically defined cell markers did not distinguish between unique cell clusters in their analysis. The authors describe this as a limitation of using such markers (e.g., neuropeptide expression) as cell population identifiers. While the authors’ points are well taken, we encourage readers to not throw out the proverbial baby with the bathwater. While a given histopathological marker may not label a completely unique population, it may contribute to how multiple populations function in concert. This is certainly true when one considers the function of the marker, especially if it has capacity to signal (like a neurotransmitter or neuropeptide released somatodendritically). Still, it is important for preclinical rodent researchers to remember that there is high overlap between many of these markers, especially within the CeA (
8). Moreover, it is important to remember that the expression of these markers (e.g., corticotropin-releasing factor [
9]) may be altered due to the environmental impact of stress, drugs, and so on, and thus these populations, ensembles, and overlapping expression patterns may shift. Indeed, the plasticity of gene expression in these systems may impede the use of these histopathologically defined cell markers for clustering analysis in organisms where there is less environmental control (humans) and smaller numbers of subjects (rhesus and humans) as compared to rodent studies.
The Kamboj et al. study was conducted with cell clusters collected from adolescent males (ages 15–19 years) and male rhesus macaques (ages 3.5–5 years). The lack of female subjects is a major limitation of the study, since neuropsychiatric disorders like posttraumatic stress disorder (PTSD), ASD, and alcohol use disorder (AUD) have distinct sex differences. PTSD is significantly more prevalent in women, whereas ASD and AUD are much more prevalent in men (although rates of disordered alcohol consumption are narrowing between men and women) (
10–
12). Furthermore, these amygdalar cell populations are likely to also show differences in gene expression across the lifespan, and therefore one may expect these clusters to shift and change in adults or in middle-aged and older populations. Nevertheless, the findings of these studies are of high importance, as many neuropsychiatric disorders begin to show onset in late adolescence (
13).
In total, the data presented by Kamboj et al. are an important contribution to understanding the form and function of the primate and human amygdala, and the cell cluster analysis described is certainly an approach that could be applied to countless disorders. The authors provide a robust framework for preclinical researchers to consider existing data in rodent models and to design new and better experiments to understand the contributions of unique populations of neurons within the vLA and CeA. Most importantly, these studies exemplify that translational research needs to flow in multiple directions, and that constantly refining our research approaches between model organisms and humans is the best way forward in discovering targets for new treatments for psychiatric disorders.