Both of these strategies are used in the research described in this review. One component of the review focuses on studies that contrast children from three groups: those with severe nonepisodic irritability, those with classic presentations of bipolar disorder, and those with no mental illness. A second component focuses on the clinical outcomes of nonepisodic irritability. To identify English-language publications on these two topics, comprehensive literature searches were conducted that included all articles on pediatric bipolar disorder or irritability published in major psychiatric journals over the past 20 years. The reference lists of these articles were reviewed to identify other papers on these two topics. Because the publications comparing youths with severe nonepisodic irritability with those with classic presentations of bipolar disorder emerged from the National Institute of Mental Health (NIMH), the source of the present article, this review necessarily focuses on these publications. Nevertheless, relevant papers from other sources also are carefully considered.
Although published data suggest that children with severe nonepisodic irritability do not suffer from bipolar disorder, at least as it is classically defined, some research groups maintain that it is nonetheless reasonable to apply a bipolar diagnosis to children with such a clinical presentation (
4–
7). One important argument for this position is that children with severe nonepisodic irritability manifest severe mood symptoms and are as severely impaired as those with classic bipolar disorder, but without a diagnosis of bipolar disorder their access to the mental health services they need might be limited. I will argue, however, that because data suggest that children with severe nonepisodic irritability do not suffer from bipolar disorder, rather than broadening the definition of bipolar disorder to include them, the issue of access to appropriate treatment may be better addressed through efforts to emphasize the seriousness of chronic irritability as a presenting symptom in children and to support research designed to delineate its pathophysiology and treatment.
Thus, while there is disagreement on whether the bipolar diagnosis should be applied to youths with severe nonepisodic irritability, there is widespread agreement that such irritability and classic bipolar disorder are both common clinical presentations in children and merit significant investment in treatment and research. In DSM-IV, a diagnosis of bipolar disorder in children, as in adults, requires the presence of a well-demarcated period of elevated or irritable mood along with associated symptoms. Research to test whether nonepisodic irritability is a developmental presentation of bipolar disorder began with the description of a syndrome called “severe mood dysregulation.” Longitudinal, family-based, and pathophysiologic studies then followed. This work demonstrates important differences between severe mood dysregulation and bipolar disorder, which in turn carry implications for therapeutics and nosology.
Diagnosing bipolar disorder in youths: the controversy
Data from both inpatient and outpatient settings indicate a recent and marked increase in the rate at which youths have received the diagnosis of bipolar disorder in the United States. Between 1994 and 2003, the percentage of visits for a mental disorder assigned the diagnosis of bipolar disorder increased from 0.42% to 6.67% in youths (
2). Similarly, between 1996 and 2004, the rate of children with a hospital discharge diagnosis of bipolar disorder increased from 1.3 to 7.3 per 10,000, and discharges of adolescents with bipolar disorder increased 400% (
1).
Such trends could result from a true prevalence increase, better case identification, or new conceptualizations of pediatric bipolar disorder. The recent child psychiatry literature contains considerable discussion on the appropriate techniques and criteria for diagnosing bipolar disorder in youths (
4,
7–
14). One particularly pressing question concerns whether youths with severe irritability but without distinct manic episodes exhibit a developmental presentation of mania.
Since well before the DSM era, bipolar disorder has been conceptualized as an illness characterized by discrete episodes of depression and hypomania or mania, with an episode consisting of 1) a distinct change in mood from baseline (i.e., elevated, expansive, or irritable mood in hypomania or mania and dysphoria or anhedonia [or, in children only, irritability] in depression) and 2) accompanying behavioral, physical, and cognitive symptoms (e.g., changes in sleep, appetite, activity, and so on). The accompanying symptoms are considered components of a mood episode only if they begin at approximately the same time as the mood disturbance or if they predate the mood disturbance but worsen concurrently with it. (For a detailed discussion of the clinical assessment of potential manic episodes and severe mood dysregulation in children, see reference
8.)
Within the past 15 years, researchers have suggested that mania presents differently in youths than in adults: in youths it presents not as distinct euphoric or irritable episodes but as persistent, nonepisodic, severe irritability (
4–
7). This marks an important deviation from the classical conceptualization of bipolar disorder and is inconsistent with the DSM-IV criterion A requirement of a “distinct period” of abnormally elevated, expansive, or irritable mood.
To understand the public health implications of this view, it is important to note the overlap between symptoms of mania and those of attention deficit hyperactivity disorder (ADHD) (
15). Distractibility, pressured speech, psychomotor agitation, racing thoughts, and increased goal-directed activity are all diagnostic criteria of mania that also occur in ADHD. Furthermore, while irritability is not a diagnostic criterion for ADHD, temper outbursts and other deficits in self-regulation are often seen in children with ADHD (
16,
17). Also, the prevalence of ADHD in youths (1.9%) is considerably higher than that of episodic DSM-IV bipolar disorder (0.1%) (
18). Therefore, viewing nonepisodic irritability as a developmental presentation of mania could markedly affect prevalence estimates of bipolar disorder; the rediagnosis of even a relatively small percentage of children with ADHD as having bipolar disorder would result in significantly higher rates of bipolar disorder. As discussed later, such rediagnosis could also have significant treatment implications. Therefore, it is important to test systematically the hypothesis that nonepisodic irritability is a form of mania.
Research strategy
In the absence of validated bipolar disorder biomarkers, how does one test whether severe nonepisodic irritability is a developmental presentation of mania? To address this question, my colleagues and I adopted two research strategies. The first involves longitudinal studies: if nonepisodic irritability is a developmental presentation of bipolar disorder, one would expect youths with this phenotype, over time, to develop episodic mania, hypomania, or bipolar disorder not otherwise specified. The second strategy involves cross-sectional studies comparing family history and pathophysiology in youths with the alternative phenotype to 1) youths with clearly episodic bipolar disorder, diagnosed using criteria and techniques parallel to those used in adults; 2) youths with psychopathology other than mood disorders; and 3) youths with no psychopathology. Because research suggests that episodic pediatric bipolar disorder exhibits a course similar to that of adult bipolar disorder (
19–
21), youths with clearly episodic bipolar disorder provide an important standard against which to test proposed alternative phenotypes. If data from youths with episodic bipolar disorder and those with chronic severe irritability resemble each other but are distinct from data from youths with other forms of psychopathology and from healthy youths, a strong argument can be made for the alternative phenotype being a form of bipolar disorder. In the absence of such data, however, this argument cannot be supported. Alternatively, if data differentiate the classic bipolar disorder phenotype from the other three groups, this would suggest that the alternative phenotype is not a form of bipolar disorder.
Notably, questions about the nosologic status of nonepisodic irritability are phrased categorically here. However, it also is important to incorporate a dimensional perspective (
22). As discussed later, data suggest that severe nonepisodic irritability in youths might be on a pathophysiologic continuum with both bipolar disorder and major depressive disorder. Nonetheless, categorical approaches are also important, since the decision to treat with one intervention rather than another is categorical.
Defining severe mood dysregulation
Questions about the appropriate criteria for pediatric bipolar disorder highlight limitations in nosology and research. First, no DSM-IV category captures the symptomatology of children characterized primarily and fundamentally by severely impairing nonepisodic irritability. Indeed, the lack of a DSM-IV category for children affected by such severe mood symptoms may have contributed to the movement toward applying to them the diagnosis of bipolar disorder. This movement in turn could have contributed to rising rates of pediatric bipolar diagnosis.
Other DSM-IV disorders do not accurately capture the phenotype exhibited by severe irritability. While criteria for oppositional defiant disorder include “often loses temper,” “often touchy and easily annoyed by others,” and “often angry and resentful,” nonirritable children can meet criteria for oppositional defiant disorder only on the basis of oppositional behavior. Furthermore, oppositional defiant disorder encompasses a wide range of clinical presentations in terms of severity. While irritability is also a diagnostic criterion for major depressive disorder in youths, this disorder, like bipolar disorder, is defined as episodic.
Second, diagnostic questions about pediatric bipolar disorder also highlight the relative paucity of research on irritability: operationalized definitions, reliable rating scales (although see references 23–25), and normative data are all sparse. In fact, DSM-IV provides no definition of irritability, despite the inclusion of this symptom as a criterion for at least six diagnoses in children (manic episode, oppositional defiant disorder, generalized anxiety disorder, dysthymic disorder, posttraumatic stress disorder, and major depressive episode).
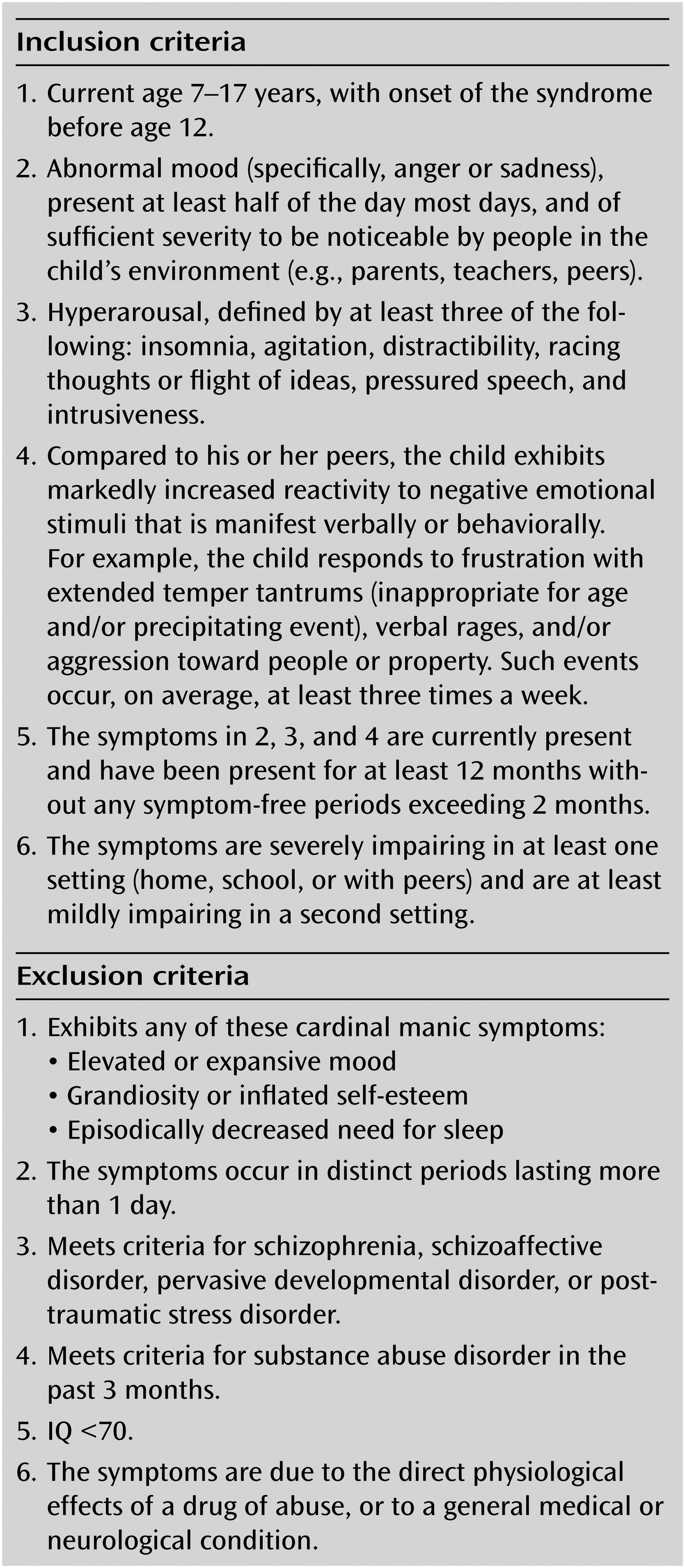
To facilitate research on nonepisodic severe irritability and its relationship to bipolar disorder, my colleagues and I (
14) defined a syndrome termed “severe mood dysregulation” (
Figure 1). The syndrome captures the symptomatology of youths whose nosologic status vis-à-vis bipolar disorder remains in doubt. In designing the criteria for severe mood dysregulation, our approach was descriptive, drawing on available data and expert consultation. We did not claim to define a discrete diagnosis; as with classic bipolar disorder, we expected that children with severe mood dysregulation would meet criteria for other syndromes as well (e.g., oppositional defiant disorder). In defining severe mood dysregulation, we had five goals: 1) to operationalize severe irritability reliably, with a high threshold, far beyond that of any current DSM-IV diagnosis; 2) to identify youths who are as severely impaired as those with bipolar disorder so that any observed differences between severe mood dysregulation and bipolar disorder could not be attributed to differences in severity; 3) to require symptoms common to mania and ADHD, since such symptoms were part of the rationale for assigning the bipolar disorder diagnosis to children with severe chronic irritability; 4) to exclude preschoolers and patients whose symptoms did not begin until adolescence, because irritability may fluctuate during these developmental transitions; and 5) to exclude youths with even brief episodes of mania, such as those meeting criteria for episodic bipolar disorder not otherwise specified (
26).
In severe mood dysregulation, irritability is defined as having two components: 1) temper outbursts that are developmentally inappropriate, frequent, and extreme; and 2) negatively valenced mood (anger or sadness) between outbursts. The latter criterion is required in order to include youths with a persistent mood disorder rather than those who have temper outbursts but normal mood between episodes. In practice, virtually all children with severe mood dysregulation meet criterion 2 by virtue of having persistently angry mood between outbursts. The two-pronged definition of irritability that we employed selects for youths with severe impairment, and other criteria increase the likelihood of accomplishing this goal—symptoms must be severely impairing in at least one of three contexts (home, school, or with peers) and at least mildly impairing in a second. To ensure that significant impairment is present and to operationalize chronicity, the syndrome must be present for at least 1 year with no more than 2 symptom-free months. And, to set clear boundaries with bipolar disorder, youths with psychosis or even brief manic or hypomanic episodes (i.e., ≥1 day) are excluded from the severe mood dysregulation group. While most children with irritability experience fluctuations in the frequency and intensity of their symptoms, this in and of itself does not constitute a manic or hypomanic episode unless the intensification of the irritability is accompanied by the onset or worsening of the DSM-IV criterion B symptoms of mania.
Since 2002, 146 youths with severe mood dysregulation have been studied at NIMH (
Table 1). To make the diagnosis of severe mood dysregulation, we use a module that is appended to the Schedule for Affective Disorders and Schizophrenia–Present and Lifetime Version (K-SADS-PL; module available on request). The module is administered by master’s- or doctoral-level clinicians who are trained to reliability (kappa=0.90), including in the distinction between severe mood dysregulation and bipolar disorder. In the NIMH sample, the mean age at study entry is 11.7 years, but parents report a mean age at onset nearly 7 years earlier. The mean Children’s Global Assessment Scale (CGAS) (
27) score is 45.8 (SD=6.9), compared with a mean score of 46.5 (SD=12.4) for 107 youths with bipolar disorder recruited over the same period, indicating that youths with severe mood dysregulation are as severely impaired as those with bipolar disorder. Approximately 60% of the youths with severe mood dysregulation had a community diagnosis of bipolar disorder at the time of recruitment.
Not surprisingly, 84.9% of the youths in the severe mood dysregulation sample met DSM-IV criteria for lifetime oppositional defiant disorder, while 86.3% met criteria for lifetime ADHD. It is also notable that 58.2% met criteria for a lifetime anxiety disorder and 16.4% for lifetime major depressive disorder, although youths are not included in the severe mood dysregulation sample if their irritability can be attributed solely to a major depressive episode or an anxiety disorder. These data indicate that the severe mood dysregulation syndrome might be conceptualized as a disruptive behavior disorder that includes significant mood and anxiety symptoms.
To more clearly place the severe mood dysregulation phenotype within the context of DSM-IV, post hoc analyses were performed using data from the NIMH Diagnostic Interview Schedule for Children, Version IV (
28), obtained from parents of youths in four community samples (approximately 9,600 youths) and two clinical samples (approximately 2,100 youths). A proxy for the severe mood dysregulation diagnosis required three symptoms of oppositional defiant disorder: temper tantrums, being angry or resentful (each at least “a few days a week”), and being touchy or easily annoyed (nearly every day). In the community samples, 15% of youths with oppositional defiant disorder met criteria for the severe mood dysregulation proxy; in clinical samples, the severe mood dysregulation phenotype accounted for approximately a quarter of the youths with oppositional defiant disorder (P. Fisher, J.B. Turner, unpublished 2010 data).
Longitudinal studies
Longitudinal data provide a particularly important approach to evaluating the validity of classification in pediatric psychopathology. Two pediatric syndromes can be viewed as pathophysiologically similar when they exhibit a similar course and predict similar risks for an adult phenotype, such as classic adult bipolar disorder, where considerable data exist on the validity of the adult phenotype. Thus, in assessing whether severe mood dysregulation is a developmental manifestation of mania, a crucial question is whether youths with the syndrome, when followed through adolescence and into adulthood, develop manic episodes, hypomanic episodes, or bipolar disorder not otherwise specified.
Relevant longitudinal data have been collected in both clinical and community samples. In our clinical research sample, we assessed rates of mood episodes in 84 youths with severe mood dysregulation and 93 youths with DSM-IV bipolar disorder over a median of 28.4 months (
21). Only one patient (1.2%) with severe mood dysregulation, but 58 (62.4%) with bipolar disorder, exhibited at least one new manic, hypomanic, or mixed episode during follow-up (Mann-Whitney U=2,720, z=–3.48, p<0.001). Thus, in this clinical sample, rates of prospectively observed manic episodes were 50 times higher in bipolar disorder than in severe mood dysregulation. Longer studies with larger clinical samples are needed.
Post hoc analyses of large community samples that have been followed for as long as 20 years complement the clinical data. None of these studies was designed to address specific questions regarding the outcome of irritability. Using post hoc proxy criteria for severe mood dysregulation, Brotman et al. (
29) found that compared to youths who never met these criteria, those who met them at a mean age of 10.6 years (SD=1.4) were seven times more likely to meet criteria for a unipolar depressive disorder at a mean age of 18.3 years (SD=2.1) (odds ratio=7.2, 95% confidence interval [CI]=1.3–38.8, p=0.02). The lifetime prevalence of severe mood dysregulation in this sample (N=1,420, ages 9–19 years) was 3.3%, whereas only 0.1% of the sample met criteria for bipolar disorder. Thus, unlike the above-noted clinic-based study, which explicitly recruited children with bipolar disorder, this epidemiologic study had relatively limited power to compare severe mood dysregulation and bipolar disorder, since bipolar disorder is far rarer than severe mood dysregulation in the community.
In another community study, Stringaris et al. (
30) reported on 631 individuals followed from a mean age of 13.8 years (SD=2.6) to a mean age of 33.2 years (SD=2.9), beyond the peak age of risk for bipolar disorder. Chronic irritability in adolescence predicted major depressive disorder at age 33 (odds ratio=1.33, 95% CI=1.00–1.78, p<0.05) as well as generalized anxiety disorder (odds ratio=1.72, 95% CI=1.04–2.87, p<0.05) and dysthymia (odds ratio=1.81, 95% CI=1.06–3.12, p<0.01). The study had a sufficient number of participants with bipolar disorder to examine predictors of the illness (
31), and adolescent irritability was not one of them. Thus, although Brotman et al. (
29) and Stringaris et al. (
30) used different methods, both studies found that adolescent irritability predicted adult unipolar depressive and anxiety disorders.
To a certain extent, these findings are consistent with studies of youths with oppositional defiant disorder. As noted above, oppositional defiant disorder differs from severe mood dysregulation in focusing primarily on oppositionality, not irritability, and in including patients with less severe illness. Studies indicate that the longitudinal predictions of oppositional defiant disorder are protean, including unipolar depressive and anxiety disorders (
32–
35) and, in some instances, bipolar disorder (
33,
34). In particular, data indicate that the irritable, but not the oppositional, dimension of oppositional defiant disorder may be associated specifically with mood and anxiety disorders (
36–
38). The decomposition of oppositional defiant disorder into its component parts, including a continued focus on the specific predictions of irritability, might improve the prognostic power of this common clinical presentation in youths.
Family history/heritability
If severe mood dysregulation is a developmental phenotype of bipolar disorder, one would expect children with severe mood dysregulation to be as likely as those with bipolar disorder to have a parent with bipolar disorder. To test this hypothesis, one small study (
39) compared parental diagnoses (determined by clinicians blind to children’s diagnoses) in samples of youths with severe mood dysregulation or bipolar disorder. The two samples differed in the prevalence of parental bipolar disorder: 33.3% in the pediatric bipolar disorder sample compared with 2.7% in the severe mood dysregulation sample (odds ratio=18.0, 95% CI=1.9–171, p
≤0.01); the latter prevalence is similar to what might be expected in a community sample. Like the longitudinal data, these family-based data suggest that severe mood dysregulation is not a developmental phenotype of bipolar disorder. Limitations of the study included small sample size and ascertainment bias.
While the results of this preliminary family study suggest a differentiation between severe mood dysregulation and bipolar disorder, they do not address the familiality of severe mood dysregulation itself, which was not assessed in parents (
39). In addition, while other studies have examined family members of children with bipolar disorder, none of them contrasted diagnoses in the families of children with classically defined bipolar disorder with diagnoses in the families of children with nonepisodic, severe, chronic irritability (
40,
41). Indeed, no published work has addressed the familiality or heritability of severe mood dysregulation or irritability, but several publications have focused on related constructs. For example, studies indicate that oppositional defiant disorder and aggression are subject to genetic influences (
42–
47). In addition, a phenotype based on scores in the clinical range of the attention, aggression, and anxious/depressed subscales of the Child Behavior Checklist (that is, the Child Behavior Checklist–juvenile bipolar disorder profile) appears to be heritable (
48,
49). Although this profile was originally described as associated with the diagnosis of pediatric bipolar disorder, data are mixed on that point, and some data suggest that the profile might be more akin to severe mood dysregulation than to episodic bipolar disorder (
11,
12,
50–
52). In sum, it appears that irritability, characterized by outbursts and inter-outburst negative mood, may be significantly influenced by genetic factors.
Pathophysiology
In psychiatric nosology, pathophysiology is an important but as yet elusive validator. A major goal of current psychiatric research is to identify biomarkers to guide diagnosis and treatment. Extending this approach, emerging research aims to identify neural mechanisms differentiating not only patients of one phenotype from healthy individuals but also patients of two phenotypes from each other and from healthy individuals (
53). In that vein, the first pathophysiologic studies of severe mood dysregulation were designed to provide “proof of principle” that, using behavioral and biological measures obtained in the laboratory and with functional MRI (fMRI), severe mood dysregulation and bipolar disorder could be differentiated from each other and from healthy individuals. Much like the family studies, studies in this area need to contrast children with classically defined bipolar disorder and children with other phenotypes, such as chronic irritability. As described below, behavioral data from these studies indicate that both youths with severe mood dysregulation and those with bipolar disorder differ from healthy comparison subjects in face emotion labeling ability, degree of subjective distress reported while performing a frustrating task, and performance on response reversal paradigms. In the first two domains, data also indicate that despite similar behavioral deficits in the two patient groups, the mediating neural circuitry differs. These findings are consistent with other work suggesting that neuroimaging techniques may be more sensitive than behavioral paradigms in detecting between-group differences (
53,
54).
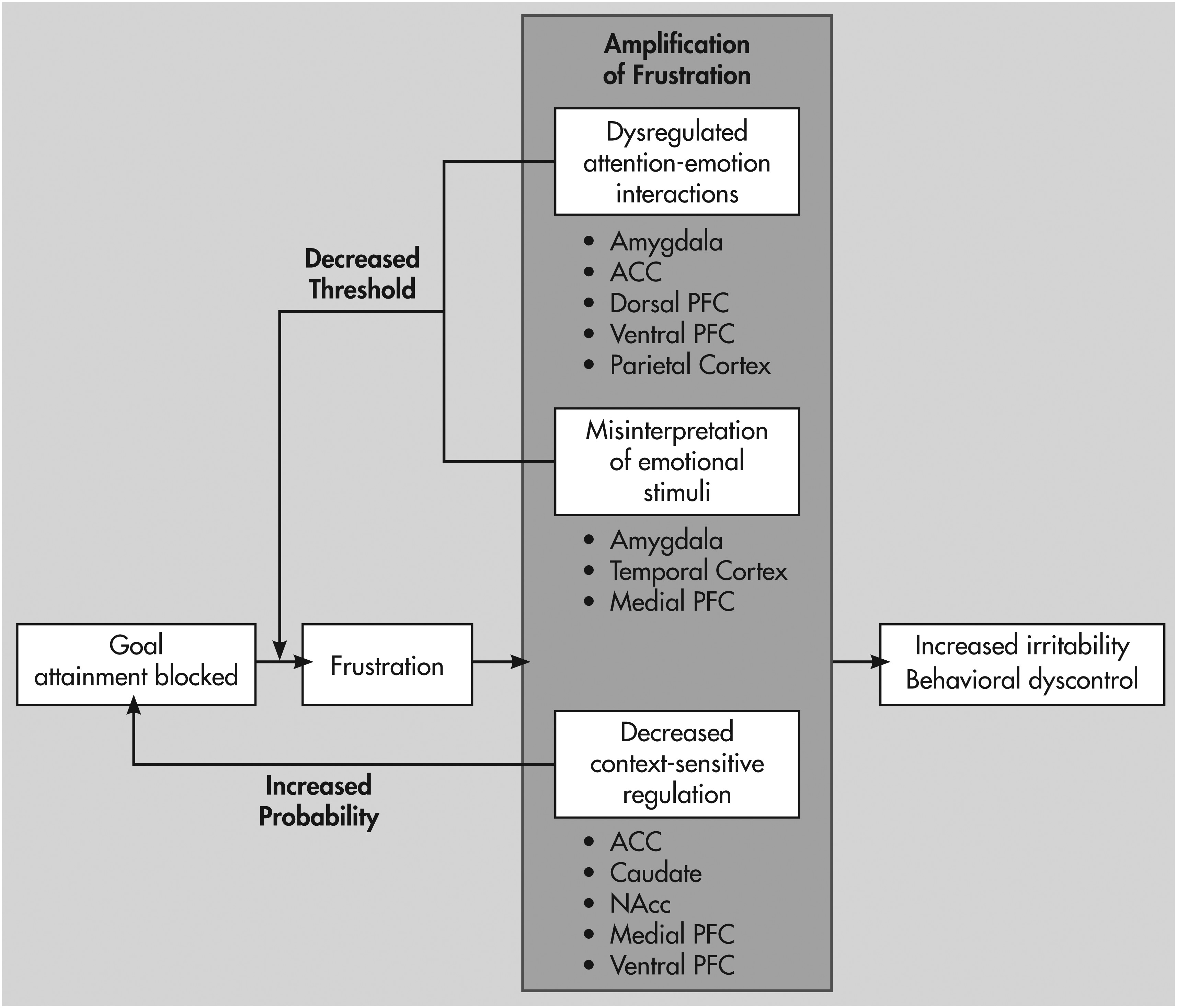
From a systems neuroscience perspective, irritability may result from an inability to engage top-down mechanisms (i.e., selective attention or higher-order mental processes [55]) in order to inhibit maladaptive responses occurring in the setting of frustration, where frustration is conceptualized as the emotional response that occurs when goal attainment is blocked. The face emotion labeling, response reversal, and attentional deficits observed in severe mood dysregulation, combined with recent research on emotion regulation in healthy volunteers and in patients with affective aggression, suggest a testable pathophysiologic model for irritability in youths (
Figure 2).
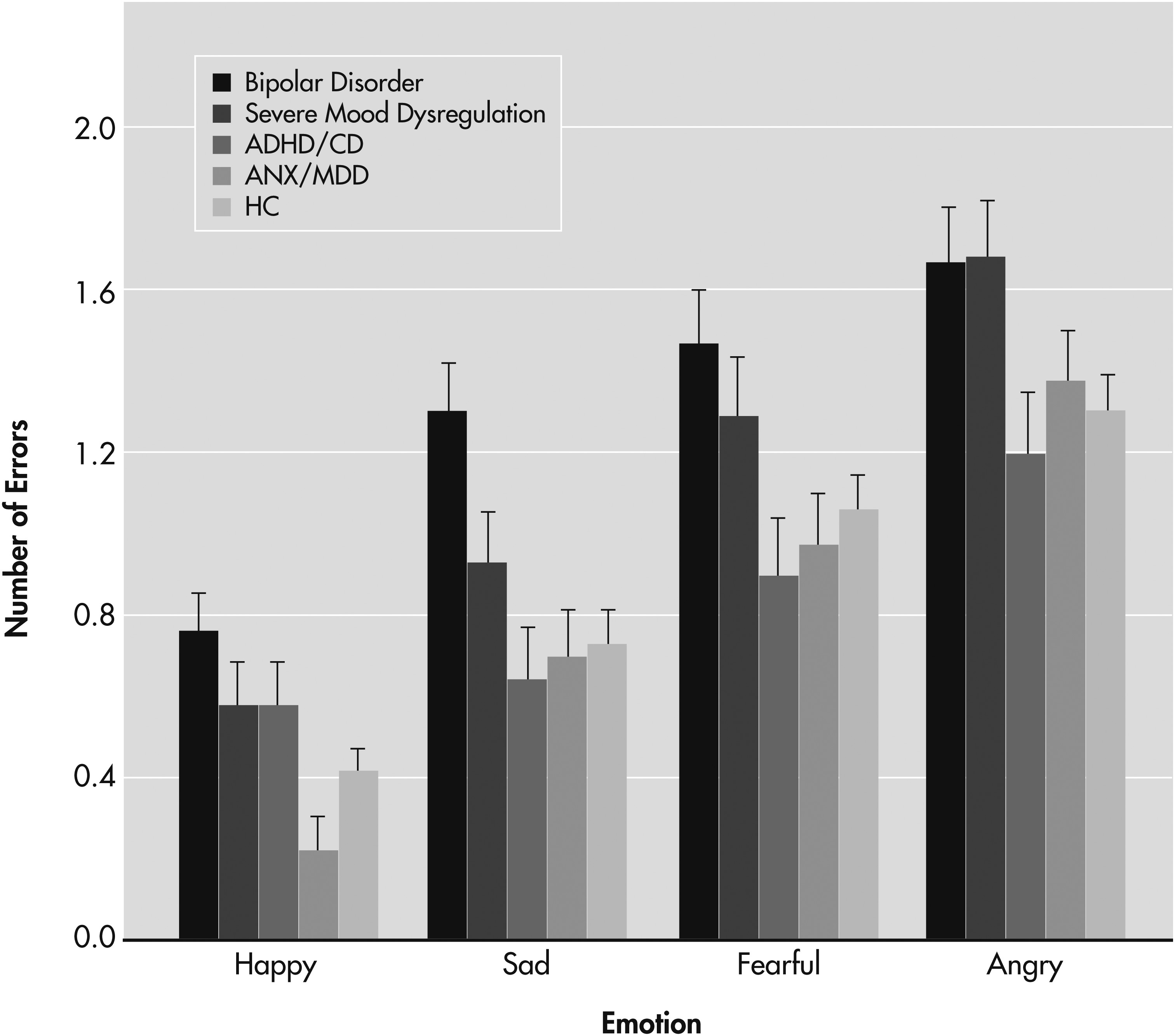
The ability to accurately process social cues, which is a core social-emotional function that facilitates both emotion regulation and social competence (
55), appears to be deficient in both severe mood dysregulation and pediatric bipolar disorder (
56,
57). Deficits in face emotion labeling are not simply nonspecific correlates of childhood psychopathology; Guyer et al. (
56) found deficits relative to healthy comparison subjects in patients with bipolar disorder and severe mood dysregulation but not in youths with ADHD and/or conduct disorder, or in those with anxiety disorders and/or major depressive disorder (
Figure 3). The fact that only the severe mood dysregulation and bipolar disorder groups differed from the healthy comparison group in performance on a face emotion identification task suggests that severe mood dysregulation and bipolar disorder might share some pathophysiologic mechanisms.
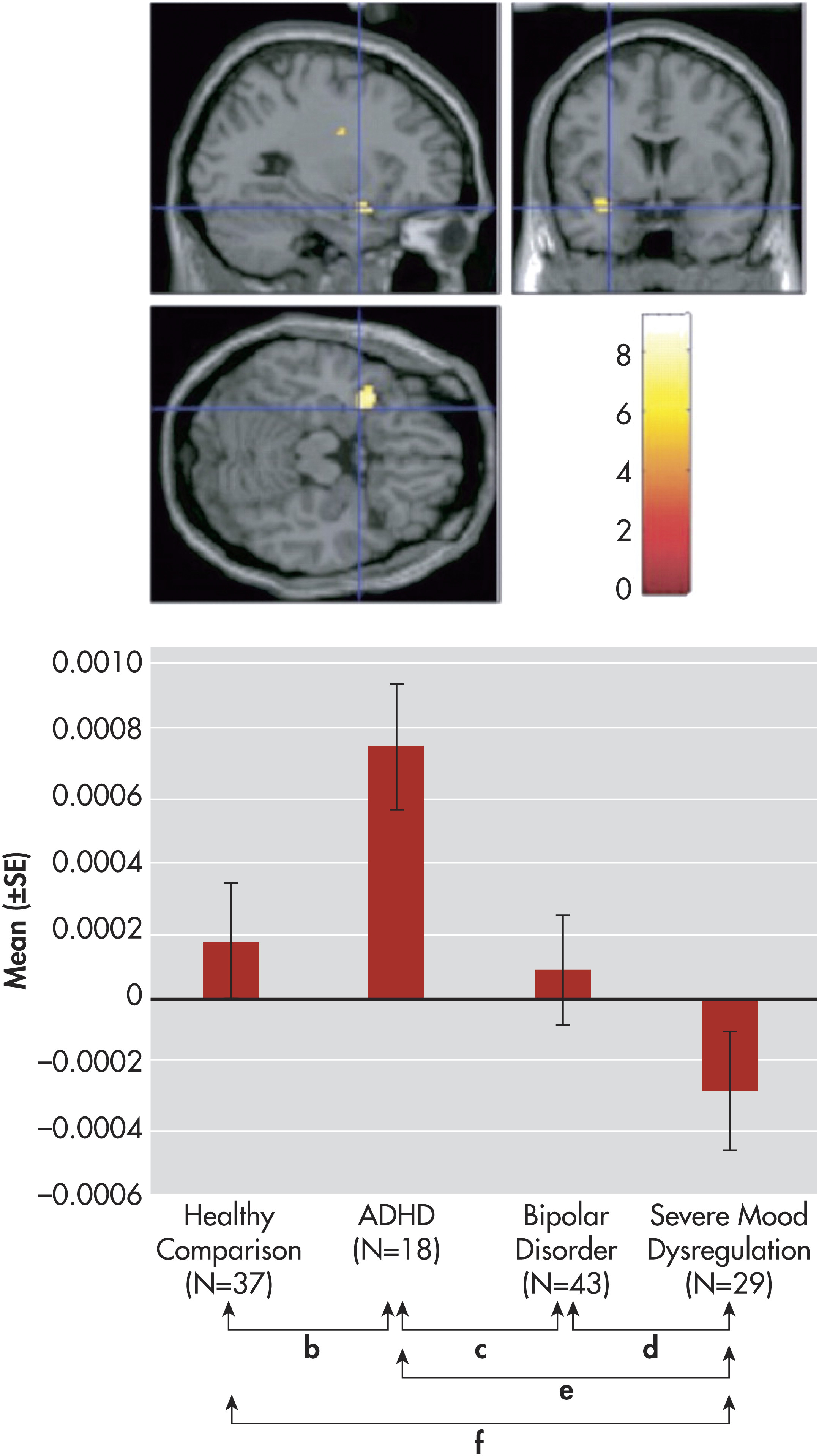
However, examinations of the neural circuitry engaged in each group during face emotion labeling highlight the fact that similar behavioral deficits can result from multiple forms of circuitry dysfunction. fMRI data suggest that despite similar face emotion labeling deficits in severe mood dysregulation and bipolar disorder, neural activity in the amygdala differs between these two groups. Youths with severe mood dysregulation exhibited lower amygdala activity while rating their subjective fear versus nose width of neutral faces, relative to patients with bipolar disorder, nonirritable youths with ADHD, and healthy comparison subjects (
58) (
Figure 4). The finding of decreased amygdala activity in severe mood dysregulation during face emotion processing is similar to one reported earlier in youths with major depressive disorder (
53); the similarity is notable given longitudinal associations between severe mood dysregulation or chronic irritability and depressive disorders (
29,
30).
Another of the core abilities for social-emotional behavior suggested by Ochsner (
55) is “context-sensitive regulation,” or the ability to adapt one’s behavior to changing environmental contingencies. Such regulation can be assessed using response reversal paradigms, in which participants must adapt their responses to changing stimulus-reward associations. As suggested by Blair (
59), an individual with deficiencies in response reversal would be at high risk of encountering frustrating situations and thus of exhibiting irritable or aggressive behavior. In this way, response reversal deficits may play a causal role in the irritability characteristic of severe mood dysregulation. Patients with bipolar disorder and those with severe mood dysregulation both differ from healthy comparison subjects in performance on response reversal paradigms (
60,
61). Ongoing research will test whether the neural circuitry mediating such deficits in severe mood dysregulation and bipolar disorder differs between these patient groups, as it did in the case of face emotion labeling. This fMRI work will use a response reversal paradigm that has already been used in youths with ADHD or psychopathic traits, thus also allowing for comparisons with these patient groups (
62).
While response reversal deficits may increase an individual’s likelihood of encountering frustrating situations, a complementary hypothesis is that the response of irritable individuals to frustrating contexts differs from that of healthy comparison subjects. If the goal is to elucidate mechanisms mediating irritable outbursts in youths, one research strategy involves neuroimaging while participants complete frustrating tasks. A study using a rigged task to elicit frustration found that while youths with severe mood dysregulation and those with bipolar disorder both reported more frustration than did healthy comparison subjects, event-related-potential measures differentiated the two groups. Youths with bipolar disorder had deficient top-down executive attention (i.e., decreased parietal P3 waves) specifically during frustration, while youths with severe mood dysregulation had deficits in bottom-up early attentional processes (i.e., decreased parietal, temporal, and central N1 and P1 waves) during both frustrating and nonfrustrating blocks (
63). Ongoing studies are extending this work using magnetoencephalography and fMRI (
64).
The finding of early attentional deficits in severe mood dysregulation is similar to results reported in youths with ADHD (
65). Indeed, since the criteria for severe mood dysregulation require the presence of three symptoms that overlap between ADHD and the criterion B symptoms for mania, it is not surprising that 86.3% of our severe mooddysregulation sample met criteria for ADHD (
Table 1). The neurobiology of emotional dysfunction in ADHD has received relatively little research attention, although interest is growing (
66–
68). Data indicate differences in amygdala activity in nonirritable youths with ADHD relative to those with severe mood dysregulation, those with bipolar disorder, and healthy comparison subjects during face processing (
58), and considerable research has found high comorbidity between oppositional defiant disorder and ADHD (
33). Thus, emotional dysregulation in ADHD merits significantly more study.
Conversely, few data have been generated to characterize the nature of attentional dysregulation in severe mood dysregulation, particularly in emotional contexts, so that too is an important area for future research. Behavioral and event-related-potential data suggest that youths with severe mood dysregulation, compared to those with bipolar disorder and/or healthy comparison subjects, may have reduced attentional interference from emotional distracters (
63,
68a). However, contradicting these findings are data from youths with severe mood dysregulation who had increased amygdala activation relative to other groups when asked to focus on nose width rather than on the emotional expression of a face, suggesting that youths with severe mood dysregulation may have difficulty focusing away from face emotions (
58). The extent to which emotion-attention interactions are abnormal in youths with severe mood dysregulation, and the precise nature of that abnormality, is important because such interactions may play a central role in emotion regulation (
69,
70).
Of course, irritability occurs in the context of many different clinical presentations (e.g., chronically in severe mood dysregulation; during episodes of mania or depression in bipolar disorder; and in specific contexts in anxious children and individuals with posttraumatic stress disorder), and data suggest that the pathophysiology of irritability, including the specific nature of the attentional control deficits, will vary across clinical presentations. In some clinical states, such as acute mania, bottom-up mechanisms may be particularly important, since increased arousal may be associated with increased irritability (
71). The extent to which the model described in
Figure 2 applies in different clinical phenotypes is therefore an important area for future research. In addition, once the heritability of irritability is established, genetic imaging studies can explore associations between genotype and neural activity in the setting of frustration and other emotional contexts.
Treatment: current literature and research gaps
The distinction between severe mood dysregulation and bipolar disorder may have important treatment implications. If severe mood dysregulation is a pediatric bipolar disorder phenotype, then first-line treatment would include mood stabilizers and atypical antipsychotics, with stimulants and selective serotonin reuptake inhibitors (SSRIs) being relatively contraindicated (
72). On the other hand, if severe mood dysregulation is more similar pathophysiologically to unipolar depressive and anxiety disorders, as well as to ADHD, then stimulants and SSRIs would be recommended. Given the relatively high side effect burden of atypical antipsychotics, coupled with the risks of using antidepressants or stimulants in bipolar disorder, this differentiation is important (
73). Indirect evidence suggests that many youths with severe mood dysregulation are receiving treatment with atypical antipsychotics, particularly risperidone (
74–
77). Possible contributors to this trend are that risperidone has received a Food and Drug Administration indication for irritability (specifically, in autism [78]) and that some controlled studies support its use in aggressive children with disruptive behavior disorders (
79).
The only treatment trial of severe mood dysregulation is a small, negative trial of lithium (
80); earlier studies showed lithium to be effective in treating aggression in the setting of conduct disorder (
81,
82). A recent controlled trial of youths with a phenotype similar to severe mood dysregulation (ADHD and aggression unresponsive to stimulants) found divalproex combined with behavioral therapy to be more effective than stimulant plus placebo and behavior therapy (
83). That study built on previous trials of divalproex in the treatment of irritable or aggressive youths (
84,
85).
A second treatment trial of severe mood dysregulation is under way (
clinicaltrials.gov identifier NCT00794040) to compare a stimulant plus citalopram to a stimulant plus placebo. The study builds on the longitudinal data reviewed above suggesting that severe mood dysregulation is on a pathophysiologic continuum with unipolar depressive and anxiety disorders, as well as data suggesting that both stimulants and SSRIs might be effective in treating irritability and/or aggression. For example, a meta-analysis of stimulant trials in ADHD found effect sizes of 0.69 and 0.84 for stimulants in the treatment of covert and overt aggression, respectively (
86). A number of double-blind controlled trials demonstrate the efficacy of SSRIs in treating irritability associated with premenstrual dysphoric disorder (
87,
88), and one trial found that fluoxetine was more effective than placebo in treating adults with intermittent explosive disorder (
89).
Clinicians or researchers who conceptualize severe, nonepisodic irritability as a phenotype of bipolar disorder are reluctant to treat youths with severe mood dysregulation with stimulants or SSRIs because of concerns about precipitating mania. However, it is important to differentiate activation from mania when assessing adverse events secondary to SSRIs. Activation is common (present in some 10%–20% of youths receiving SSRIs) and generally responds to temporary discontinuation of medication with reinstitution at a lower dosage (
90,
91). Mania in response to SSRIs is uncommon and can be difficult to differentiate from spontaneous cycling (
92,
93); however, there is evidence that children may be at higher risk than adults for antidepressant-induced mania and/or activation (
94,
95).
There are no systematic data regarding the risk of stimulant-induced mania in severe mood dysregulation. However, preliminary data suggest that youths with related phenotypes may respond as well to stimulants as those with uncomplicated ADHD (
96,
97). Considerably more research is needed to determine whether treatment with SSRIs and/or stimulants is effective and safe in treating severe mood dysregulation. A particularly important question is whether children with the severe mood dysregulation phenotype and a parent with bipolar disorder differ from those with severe mood dysregulation but no family history of bipolar disorder in their risk of developing mania, either spontaneously or in response to an activating medication.
In both medication and psychotherapeutic treatment trials, irritability is rarely the major outcome variable. Few scales capture the phenomenology of irritability precisely, and those that do tend to focus on its more extreme behavioral manifestations, such as aggression (for example, see references 78 and 83). While some psychotherapeutic trials focus on overt aggression in adolescents, few trials have examined school-age children with frequent outbursts that are impairing but not always violent (
98,
99). Furthermore, such trials frequently include youths with both proactive and reactive aggression, whereas most youths with severe mood dysregulation exhibit only the latter. Since psychotherapeutic interventions are likely to play an essential role in the treatment of severe mood dysregulation, high-priority areas for research include the development of more fine-grained assessment tools for irritability, as well as interventions aimed at a range of its manifestations. Several interventions designed for children with severe mood disorders, including bipolar disorder, may include relevant components (
100,
101).
Future directions in nosology: DSM-5
One important positive outcome of the controversy about pediatric bipolar disorder is the attention drawn to a relatively large population of severely impaired youths who do not fit well into any one DSM-IV category. In DSM-IV, the severe mood dysregulation phenotype is best captured by oppositional defiant disorder. However, oppositional defiant disorder captures a broad range of severity (whereas youths with severe mood dysregulation are all, by definition, severely impaired) and focuses strongly on oppositional behavior, which may have different treatment implications and longitudinal predictions than irritability (
36,
37).
Thus, in considering how to better serve the clinical needs of youths with the severe mood dysregulation phenotype, the DSM-5 work groups considered creating a specifier for oppositional defiant disorder that focused on the irritable, rather than the headstrong, criteria for the disorder; required impairment in at least two of three settings (at home, at school, and with peers); and set a high threshold for number of outbursts per week. Alternatively, the work groups considered creating a separate diagnosis to encompass the severe mood dysregulation phenotype. The latter strategy was adopted in the draft proposal for DSM-5, which thus includes the diagnosis of temper dysregulation disorder with dysphoria (
102). The criteria for this diagnosis resemble those for severe mood dysregulation, with the major difference being that temper dysregulation disorder with dysphoria does not require “hyperarousal”—that is, the criterion B symptoms for mania and the ADHD criteria (
Figure 1, inclusion criterion 3). In the judgment of the DSM work groups, the presence of such symptoms would best be denoted by assigning the diagnoses of both temper dysregulation disorder with dysphoria and ADHD to patients who meet criteria for both syndromes. However, a disadvantage of this decision is that temper dysregulation disorder with dysphoria itself has not been studied systematically. As with severe mood dysregulation, the criteria for temper dysregulation disorder require pervasive negative-valence mood between outbursts.
The work groups’ decision to propose a separate diagnosis of temper dysregulation disorder with dysphoria rather than an oppositional defiant disorder specifier was based on several considerations. Among the advantages of the new diagnosis are that it would be placed in the mood, rather than the disruptive behavior, section of DSM-5, thus highlighting the fact that irritability is a mood disturbance, frequently accompanied by anxiety, that predicts subsequent mood and anxiety disorders (
29,
30,
36,
37). The goal would be to draw clinicians’ attention to interventions targeting mood and anxiety disorders and to encourage researchers to undertake both pharmacologic and psychotherapeutic clinical trials for this underserved yet severely impaired population. The major argument for a specifier is that it would be more consistent with data indicating that the severe mood dysregulation/temper dysregulation disorder with dysphoria phenotype is on a phenomenological continuum with oppositional defiant disorder. At the time of this writing, DSM-5 has not been finalized, and final decisions will be informed by field trials and further discussion.
Conclusions
At least two important lessons can be drawn from the controversy about the diagnosis of pediatric bipolar disorder. First, available data do not support categorizing children with nonepisodic severe irritability as manic. That is, evidence suggests that youths with nonepisodic irritability 1) are at increased risk for unipolar depressive and anxiety disorders, rather than manic episodes, as they age; 2) do not have high familial rates of bipolar disorder; and 3) differ pathophysiologically from youths with DSM-IV bipolar disorder. Thus, at this time, the available data support reserving the diagnosis of mania for youths who have a distinct change in mood (elevated, expansive, or irritable) accompanied by the onset or worsening of the criterion B symptoms of mania. This conclusion is tempered by the fact that the research requires replication by other groups and in larger samples. Also, it is possible that as the genetics and pathophysiology of both bipolar disorder and severe nonepisodic irritability are discovered, these two clinical phenotypes will be found to share pathogenic mechanisms and thus may ultimately be considered to be on a pathophysiologic spectrum with each other as well as with major depressive disorder. It is also important to note that the longitudinal outcome of children with a family history of bipolar disorder and nonepisodic irritability is unknown.
The second lesson is that irritability is a common, yet relatively understudied, symptom in pediatric psychopathology. Children with DSM-IV bipolar disorder and those with severe mood dysregulation are both severely (and equally) impaired, and data suggest that the severe mood dysregulation phenotype is considerably more common than bipolar disorder (
29). Consequently, there is a pressing need for controlled treatment trials in severe mood dysregulation or related phenotypes. While a few have been conducted (for example, see references 80 and 83), the small number of pharmacologic or psychosocial intervention trials pales in comparison with the clinical need. In particular, an open and important question is whether the first-line treatment for severe mood dysregulation should be the same as for bipolar disorder. Such clinical trials would be facilitated by the further refinement of scales that measure the multiple manifestations of irritability and are sensitive to change. Other important research gaps include the continuity between severe irritability in youth and adult phenotypes, including intermittent explosive disorder (
89); the heritability and genetics of irritability; and the mediating neural circuitry. As noted above, irritability can be conceptualized within the frame-work of affective neuroscience and studied with fMRI and other techniques.
Irritability is a pressing problem for clinical neuroscience and treatment research. Indeed, given the number of affected children and the severity of their impairment, the need could not be greater.