It is estimated that most Americans (81.7%) will be exposed to a trauma during their lifetime (
Sledjeski, Speisman, & Dierker, 2008) and 6.8% will meet criteria for Posttraumatic Stress Disorder (PTSD) at some point in their lives (
Kessler et al., 2005). It has been estimated that anxiety disorders account for one third of all mental health care costs in the United States and PTSD is the most costly anxiety disorder (
Greenberg et al., 1999). Compared to individuals without PTSD or with other disorders, those with PTSD are more likely to have other current or past psychiatric diagnoses, with lifetime psychiatric comorbidity rates on the order of 80% (
Fairbank, Ebert, & Caddell, 2001). Further, PTSD is associated with disruptions in work, social functioning, and physical health (
Alonso et al., 2004;
Galovski & Lyons, 2004;
Smith, Schnurr, & Rosenheck, 2005;
Zatzick et al., 1997).
Fortunately, many studies have documented the efficacy of pharmacotherapy and psychotherapy for posttraumatic stress disorder (PTSD). A meta-analysis of pharmacotherapy for PTSD showed that more patients responded to medication (59.1%) compared to placebo (38.5%) (
Stein, Ipser, & Seedat, 2006). However, the best evidence and treatment guidelines suggest trauma focused psychotherapy is more effective and should be considered a first line treatment for PTSD (
Foa, Keane, Friedman, & Cohen, 2009;
NICE, 2005;
Penava, Otto, Pollack, & Rosenbaum, 1996). Existing meta-analyses of psychotherapy trials have provided estimates of the effect sizes of psychotherapy on trauma-related and other symptoms. For example, Sherman examined whether psychological treatments for PTSD (e.g. CBT, EMDR, and Dynamic therapy; 17 studies) were effective (
Sherman, 1998). The results showed a moderate effect of treatment on improvement in PTSD symptoms (
d = 0.52). However, this study did not examine the relative efficacy of psychological treatments compared to control groups. Also,
Van Etten and Taylor (1998) examined the efficacy of all treatments for PTSD (61 studies including pharmacotherapy, psychotherapy, and control conditions). Overall, psychological and pharmacological treatments outperformed controls. In addition, eye movement desensitization and reprocessing (EMDR) and cognitive behavioral therapy were identified as more effective than other psychological treatments. A meta-analysis by
Bradley, Greene, Russ, Dutra, and Westen (2005) also supported the efficacy of psychotherapy for PTSD with data from 26 controlled trials across multiple treatments.
More recent meta-analyses have focused on the efficacy of specific psychological treatments for PTSD.
Seidler and Wagner (2006) compared seven studies of “trauma-focused” cognitive behavioral therapy (CBT) to EMDR. The results showed that both treatments were effective with no significant differences between treatments. In an analysis of 33 studies,
Bisson and Andrew (2007) demonstrated that “trauma-focused” CBT, EMDR, stress management and group “trauma-focused” CBT were more effective than “non-trauma focused” treatments at reducing PTSD symptoms. In a similar study,
Bisson et al. (2007) analyzed 38 studies on “trauma-focused” CBT, EMDR, stress management, and group CBT. Results indicated that “trauma-focused” CBT and EMDR were more efficacious than waitlist/control on most outcome measures; however, the evidence for EMDR was not as strong. In contrast,
Benish, Imel, and Wampold (2008) found no significant differences among active psychological treatments for PTSD (15 studies); Benish et al. interpreted this lack of treatment differences as evidence that “specific ingredients may not be critical for the treatment of PTSD” (p. 754). However, their meta-analysis did not include comparisons between active treatments and those comprising only nonspecific factors (e.g., therapeutic alliance). Furthermore, the authors stated that “although prolonged exposure has been selected … as a model treatment for dissemination … the meta-analytic findings do not suggest that any particular therapy is superior to another” (p. 755). However, the inclusion of comparisons between very similar, effective treatments (e.g., prolonged exposure vs. prolonged exposure plus cognitive restructuring) would not be expected to reveal differences, and therefore would obscure overall treatment differences.
Previous meta-analyses have also collapsed “trauma-focused” therapies together such that any significant outcome differences among treatments are obscured. Because the procedures of these treatments vary, the ways in which trauma is addressed also differ; thus, the effects of these treatments may differ as well. The present study investigates the efficacy of one specific type of this therapy, prolonged exposure (PE). PE is a manualized treatment package that consists of 9 to 12 90-min sessions. Sessions one and two include information gathering and psychoeducation. The later sessions include repeated imaginal exposure to the index trauma and assignment of in-vivo exposure homework to avoided trauma cues.
PE was chosen as the focus of this analysis for several reasons. First, the American Psychological Association’s Division 12, which addresses empirically-supported psychological treatments, concluded that PE has “strong research support,” making it a “well-established” treatment for PTSD. In addition, several new randomized controlled trials (RCTs) have examined the efficacy of prolonged exposure (
Gilboa-Schechtman et al., unpublished manuscript;
Nacasch et al., under review;
Schnurr et al., 2007). These new RCTs also provide follow-up data that allow for a more thorough evaluation of the maintenance of PE’s effect. Further, PE was chosen for national dissemination by major healthcare administrations due to its efficacy. For example, the Veterans’ Administration Office of Mental Health Services recently funded a “national rollout” to disseminate of PE into VA hospitals as a treatment of choice for veterans suffering from PTSD (
Nemeroff et al., 2006). Likewise, the Substance Abuse and Mental Health Services Administration (SAMHSA) recommended PE as a model treatment for nationwide use (
Nemeroff et al., 2006). Despite the evidence supporting this treatment, no meta-analyses have been conducted to examine the unique contribution of PE. Therefore, the purpose of this meta-analysis is to provide an up-to-date estimate of treatment efficacy for PTSD by combining multiple randomized controlled trials of PE. In addition, this meta-analysis addresses some of the issues raised by
Benish et al. (2008) above by including conditions that control for non-specific factors. Outcome variables were classified into two categories: primary (PTSD symptom severity) and secondary (general subjective distress;
Table 1).
We derived several hypotheses from the existing literature. First, we expected that PE would outperform control conditions on primary outcome measures (Hypothesis 1) and secondary outcome measures (Hypothesis 2) at post-treatment. In addition, we predicted that waitlist controlled trials would produce larger effect sizes than psychological placebo controlled trials at post-treatment (Hypothesis 3). We did not expect PE to outperform other active treatment conditions (e.g. EMDR, CPT; Hypothesis 4). At follow-up, we expected that PE would outperform control conditions on primary outcome measures (Hypothesis 5) and secondary outcome measures (Hypothesis 6). Finally, in follow-up analyses we examined the potential moderating effect of publication year and dose (number of sessions) on effect size. Publication year was included as a potential moderator to examine whether effect sizes are changing over time (due to, e.g., refinements are rendering the treatments more efficacious).
1. Method
1.1. Study Selection
We selected well-controlled randomized trials of PE for PTSD using a comprehensive search strategy. We searched the following databases: PsycINFO (1840 to March 2009), MEDLINE (1966 to March 2009), Scopus (1869 to March 2009), and the Cochrane Central Register of Controlled Trials up to March 2009. The searches included the following terms: “prolonged exposure,” “cognitive behavioral,” “clinical trial,” “random,” “randomly,” “randomize,” “randomise,” “randomized,” or “randomised” alone and in combination with “posttraumatic,” “post-traumatic,” “posttraumatic stress disorder,” “post-traumatic stress disorder,” or “PTSD”. These words were searched as key words, title, abstract, and Medical Subject Headings. Also, we examined citation maps and used the “cited by” search tools. These findings were cross-referenced with references from reviews. In addition, we contacted authors of PE randomized trials for emerging publications. These initial search strategies produced 127 potential articles. Examination of the abstracts identified 23 relevant articles. Inclusion criteria were as follows: (a) participants who met full DSM-III-R, DSM-IV, or DSM-IV-TR criteria for posttraumatic stress disorder; (b) random assignment; (c) adequate control condition (psychological placebo or wait-list control); (d) adult or adolescent participants; and (e) more than one session of PE during the acute phase of treatment. Treatments were classified as PE if they included both imaginal and in vivo exposure. Exposures were classified as in vivo if they involved confronting trauma cues in real life. All included studies used exposure therapy that was based on the manualized treatment developed by
Foa et al. (1991). Exclusion criteria were: (a) single case studies; (b) studies focused on acute stress disorder; and (c) studies with insufficient data, unless study authors were able to provide such data. Of the 23 identified studies, ten were excluded. Four studies had inadequate trials of PE based on the above definition (
Bryant et al., 2003;
Cloitre, Koenen, Cohen, & Han, 2002;
Glynn et al., 1999;
Ironson, Freund, Strauss, & Williams, 2002). Four studies did not have an adequate control condition (
Bryant et al., 2008;
Ironson et al., 2002;
Lee, Gavriel, Drummond, Richards, & Greenwald, 2002;
Paunovic & Öst, 2001); in one study medication was the only treatment provided during the acute phase of treatment (
Rothbaum et al., 2006); and in one study over one third of the participants did not meet full DSM-IV-TR criteria for PTSD (
Difede et al., 2007). Thirteen studies with a total sample size of 658 participants met the final inclusion criteria and were included in the meta-analysis.
1.2. Software
All analyses were completed with Comprehensive Meta-Analysis (
Borenstein & Rothstein, 1999). Comprehensive Meta-Analysis is a program funded by the National Institutes of Health’s SBIR program.
1.3. Procedure
Data on the following variables were collected: treatment conditions, treatment dose (number of sessions and total hours), number of participants, and year of publication. Dependent variables were classified into categories including primary (PTSD/domain-specific subjective distress) and secondary (general subjective distress:
Table 1). In some of the included comparisons, PE was modified and combined with other treatments such as cognitive restructuring (
Foa et al., 1999,
2005;
Marks, Lovell, Noshirvani, Livanou, & Thrasher, 1998;
Power et al., 2002); results will be reported with and without these comparisons included.
Control conditions were classified into three categories: active treatment, psychological placebo or wait-list. Active treatment was defined as those treatments that were purported to contain specific ingredients to alleviate PTSD symptoms. Treatments that were categorized as psychological placebo included: supportive counseling (SC), relaxation (R), Present Centered Therapy (PCT), Time Limited Psychodynamic Therapy (TLDP), and treatment as usual (TAU). Wait-list (WL) was defined as a control condition in which participants did not receive any treatment for PTSD symptoms for a specified amount of time. Six of thirteen studies utilized psychological placebos as the control condition, 5 of the 13 studies had wait-list as the control condition and 2 of the 13 studies included both a psychological placebo condition and a wait-list condition (see
Table 2).
1.4. Study Quality Ratings
The quality of the included studies was then rated using a modified version of Jadad et al.’s quality assessment guidelines (
Jadad et al., 1996). Jadad et al. included three criteria for the quality assessment: 1) random assignment to condition; 2) double-blinding; and 3) description of withdrawals and dropouts. Because this meta-analysis reviews a psychological treatment, the second criterion cannot be applied here because patients cannot remain blind to their treatment condition; therefore we modified this criterion to require that the evaluators were blind to the therapeutic condition (i.e., single blind).
1.5. Effect Size Calculation
Between-group effect sizes for each study were computed using Hedges’s g (
Rosenthal, 1991). Studies with multiple outcomes were categorized as above (see
Table 1) and then combined within each domain. When the necessary data were available, Hedges’s g was calculated directly using the following formula:

where

is the mean of the treatment group,

is the mean of the comparison group, and
SP is the pooled standard deviation. If these data were not provided, Hedges’s g was estimated using conversion equations for significance tests (e.g.,
t,
F) (
Rosenthal, 1991). All effect sizes were corrected for small sample sizes according to
Hedges and Olkin (1985). Therefore, a smaller sample size reduces the estimated effect size helping control for different sample sizes across studies. These controlled effect sizes may then be interpreted conservatively with Cohen’s convention of small (0.2), medium (0.5), and large (0.8) effects (
Cohen, 1988). Hedges’s
g also may be computed directly from Cohen’s
d with the following formula:
. When there were multiple outcomes per domain they were combined according to
Borenstein, Hedges, and Rothstein (2007). The overall mean effect size for all of the studies combined was computed using the following formula:

where
wj is the weight for each study and
gj is the effect size for each study. Effect sizes were calculated with random effects models. The random effects analysis estimates the overall effect size assuming the studies included are only a sample of the entire population of studies and/or when the studies are heterogeneous.
2. Results
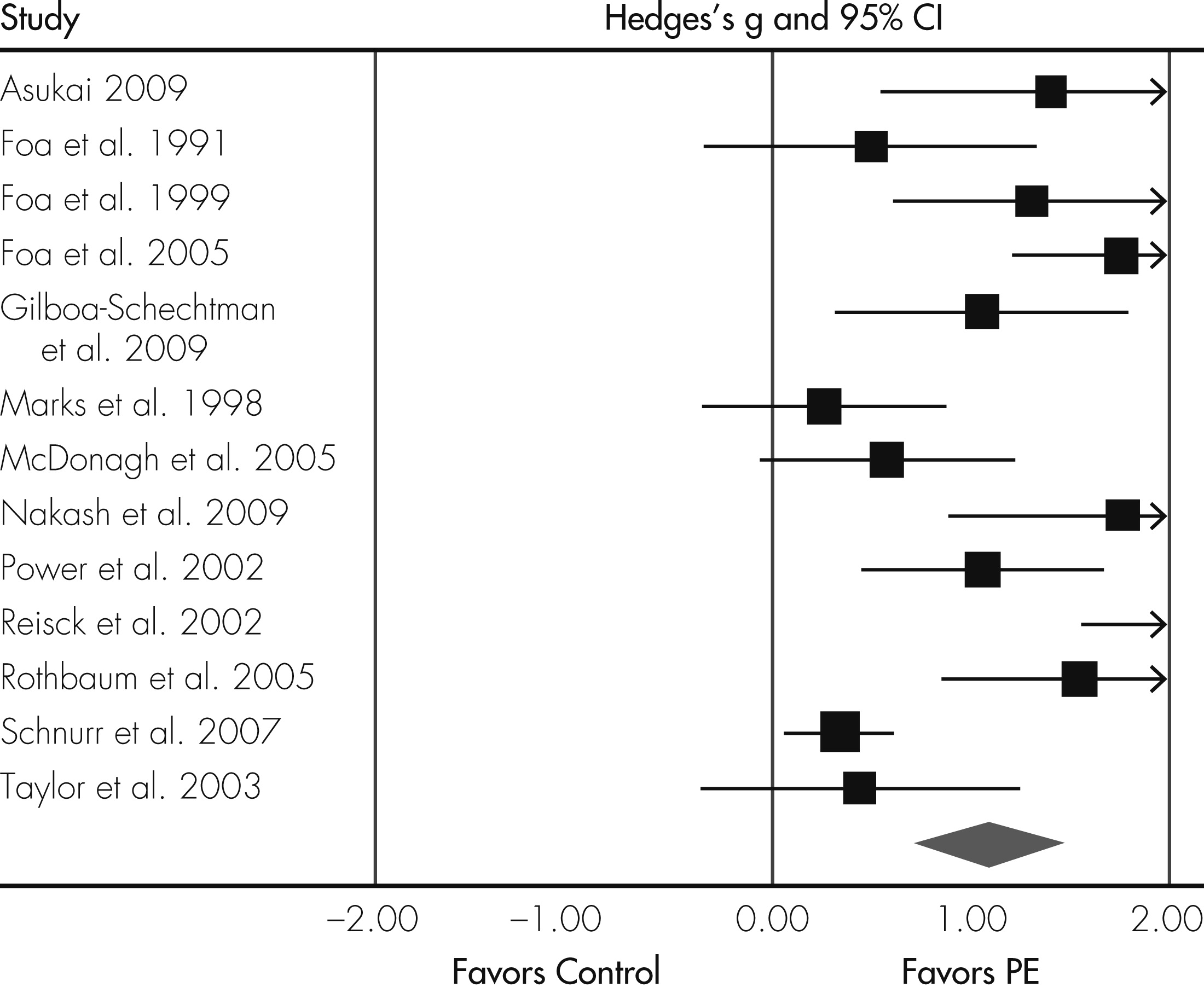
Hypothesis 1.
PE will outperform the control conditions on primary outcome measures at post-treatment.
This analysis included 13 studies with 675 participants. Consistent with prediction, prolonged exposure outperformed control conditions on primary outcome measures at posttreatment showing a large effect size (Hedges’s
g = 1.08 [SE = 0.20, 95% CI: 0.69 to 1.46,
p < 0.001)]). Thus, the average participant receiving prolonged exposure fared better than 86% of the control participants at posttreatment on primary outcome measures (
Fig. 1).
Hypothesis 2.
PE will outperform the control conditions on secondary outcome measures at post-treatment.
This analysis included 13 studies with 666 participants. Consistent with prediction, prolonged exposure outperformed control conditions on secondary outcome measures at posttreatment showing a large effect size (Hedges’s g = 0.77 [SE = 0.12, 95% CI: 0.53 to 1.01, p < 0.001]). Thus, the average participant receiving prolonged exposure fared better than 79% of the control participants at posttreatment on secondary outcome measures.
Hypothesis 3.
PE versus wait-list will produce a larger effect than PE versus psychological placebo at post-treatment on primary outcome measures.
This analysis included 13 studies with 675 participants. Consistent with prediction, the overall effect size of PE compared to wait-list (Hedges’s g = 1.51 [SE = 0.20, 95% CI: 1.12 to 1.90]) was significantly greater than the overall effect size of PE compared to psychological placebo (Hedges’s g = 0.65 [SE = 0.19, 95% CI: 0.29 to 1.01]) at post-treatment (p = .001).
Hypothesis 4.
PE will not significantly outperform other active treatments on primary outcome measures.
This analysis included 6 studies with 262 participants in PE, EMDR, CPT, CT, and SIT. Consistent with prediction, there was not a significant overall difference between PE and active treatment conditions on primary outcome measures at posttreatment (Hedges’s g = −0.07 [SE = 0.18, 95% CI: −0.42 to 0.28, p = .69]).
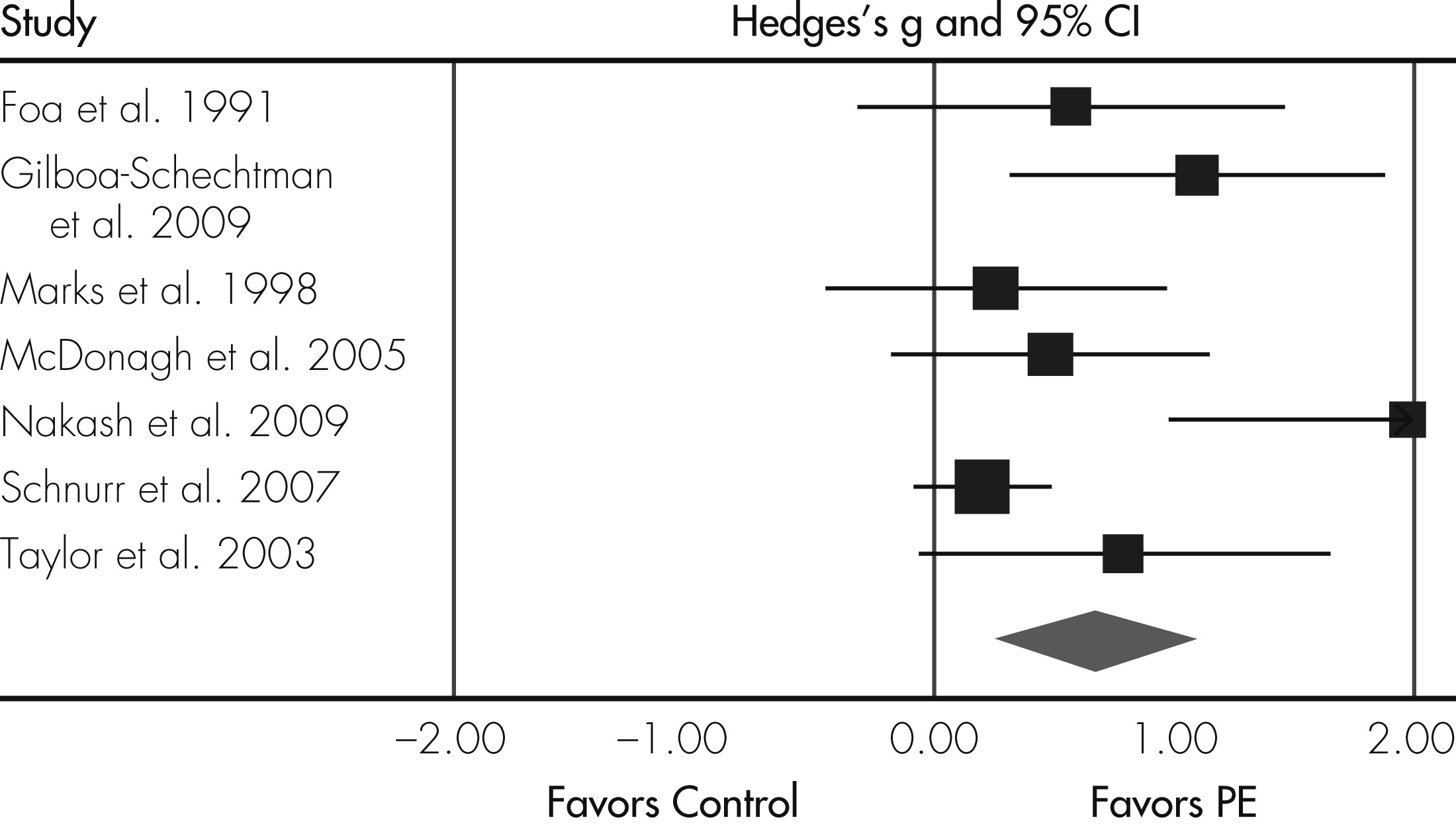
Hypothesis 5.
PE will outperform the control conditions on primary outcome measures at follow-up
This analysis included 7 studies with 348 participants. Follow-up assessments ranged between one and 12 months. Consistent with prediction, PE outperformed control conditions at follow-up on primary outcome measures showing a medium to large effect size (Hedges’s
g = 0.68 [SE = 0.21, 95% CI: 0.27 to 1.10,
p = .001]). Thus, the average participant receiving prolonged exposure fared better than 76% of the control participants at follow-up on primary outcome measures (
Fig. 2).
Hypothesis 6.
PE will outperform the control conditions on secondary outcome measures at follow-up.
This analysis included 7 studies with 368 participants. Consistent with prediction, PE outperformed control conditions at follow-up on secondary outcome measures showing a medium effect size (Hedges’s g = 0.41 [SE = 0.19, 95% CI: 0.03 to 0.78, p = .03)]). Thus, the average participant receiving prolonged exposure fared better than 66% of the control participants at follow-up on secondary outcome measures.
3. Validity of Meta-Analytic Results
3.1. Heterogeneity
A heterogeneity analysis was conducted to test the assumption that the effect sizes were from a homogeneous sample (
Hedges & Olkin, 1985). For this analysis all 13 studies were included with all time points (post-treatment and follow-up) on primary outcome measures. The test was significant, Q(12) = 59.90,
p<0.001, suggesting that the random effects analyses were most appropriate for this study.
3.2. Moderators: Effect Size as a Function of Publication Year, Dose, Type of Trauma, and Time Since Trauma
The following analyses were completed using unrestricted maximum likelihood meta regressions. There was no significant relationship between effect size and time since trauma (β = 0.55, p = 0.61), publication year (β = −0.00, p = 0.86), dose (β = −0.01, p = 0.71), or study quality (β = −0.30, p = 0.07). There was also no significant difference in effect sizes across types of trauma (combat/ terror, childhood sexual abuse, rape, mixed: p = 0.14).
3.3. Publication Bias: “The File Drawer Problem”
Several authors suggest there may be a potential discrepancy between the number of published trials and the total number that are completed (
Bakan, 1967;
McNemar, 1960;
Smart, 1964;
Sterling, 1959). Therefore, any meta-analysis of published studies may be missing non-significant studies and therefore overestimate the overall effect size. Rosenthal and others have called this confound “The File Drawer Problem” (
Rosenthal, 1991). A conservative method of addressing this problem is to assume that the effect sizes of all current or future
unpublished studies are equal to 0 and compute the number of such studies it would require to reduce the overall effect size to a non-significant level (
Rosenthal & Rubin, 1988). This value may be referred to as the “fail-safe
N”.
Rosenthal suggested the following equation to compute a fail-safe

where
K is the number of studies in the meta-analysis and

is the mean
Z obtained from the
K studies (
Rosenthal, 1991). Rosenthal also suggested that findings may be considered robust if the required number of studies (
X) to reduce the overall effect size to a non-significant level exceeded 5 K + 10 which in this study would be 75 (
Rosenthal, 1991). Analyses revealed that it would require more than 446 current or future unpublished studies with an effect size of 0 to bring the overall effect size of the primary analyses within the non-significant range, suggesting that the findings in this meta-analysis are robust.
4. Discussion
4.1. Major Findings
This meta-analysis of 13 (
N = 658) randomized controlled PE trials generally supported the hypotheses. As predicted, PE performed significantly better than control conditions on measures of PTSD both at post-treatment (
g = 1.08) as well as at follow-up (
g = 0.68). Similarly, PE treatment was associated with significantly better outcomes on secondary outcome measures, both at post-treatment (
g = 0.77) and at follow-up (
g = 0.41). These effect sizes compare quite favorably to those of other empirically supported psychotherapies; for example, cognitive therapy for depression has a reported effect size at post-treatment of
d = 0.82 versus wait-list or placebo (
Gloaguen, Cottraux, Cucherat, & Blackburn, 1998). In addition, the large effect sizes associated with PE in the present analyses are in contrast to the relatively smaller effects seen when “psychotherapeutic treatments” were lumped together (
d = 0.52 post-treatment,
d = 0.64 at follow-up) (
Sherman, 1998). The current effect sizes were very robust and clearly not attributable to publication bias, given that it would require more than 400 PE trials with effect size equal to 0 to render the current results nonsignificant (
Rosenthal, 1991). Taken together these results demonstrate that PE is a highly effective treatment for PTSD that confers lasting benefits across a wide range of outcomes.
Consistent with previous meta-analyses, there was no significant difference between PE and other active treatments (CPT, EMDR, CT, and SIT). This meta-analysis cannot answer the question of why these different treatments show similar efficacy. It is possible that these treatments work through separate mechanisms that are equally efficacious. Alternatively, it may be that the application of exposure routinely employed in all of these treatments is responsible for improvement. Future research may help further answer this question. Consistent with our hypothesis, the effect size for PE versus wait-list (
g = 1.06) was significantly greater than the effect size for PE versus psychological placebo (
g = 0.65). This is consistent with previous meta-analyses of psychological approaches (e.g.
Feske & Chambless, 1995). There was significant effect size heterogeneity among the 13 studies included in the meta-analysis, indicating greater variability in effect sizes across studies than would be expected from sampling error alone (
Hedges & Olkin, 1985). There was no significant relationship between effect size and dose (number of sessions). This finding could be due to restricted range (8 to 17 sessions) or flexible dosing (4 studies included flexible dosing). However, when the four studies with a flexible dose were removed we also found no relationship between effect size and dose (
β = − 0.09,
p = 0.61). It is also encouraging to note that effect sizes were not moderated by time since trauma, publication year, study quality, or type of trauma.
Results of the current meta-analysis have meaningful implications for mental health professionals who treat patients with PTSD. A therapist can expect that his/her average PE treated patient will fare better than 86% of patients treated with supportive counseling and similar unstructured talk therapies. The present analyses are also of interest to patients with PTSD who are weighing their treatment options, as well as to policy makers responsible, for example, for setting training priorities.
4.2. Limitations
Several limitations deserve comment. First, the current analyses cannot definitively answer the question of the relative effectiveness of PE compared to other active psychological treatments for PTSD as there were an insufficient number of eligible studies comparing PE with CPT (one study), EMDR (three studies) or SIT (two studies), to obtain a stable estimate of these effect sizes. Nevertheless, we presented this analysis by combining the six comparison treatments. There also are too few dismantling studies to examine the relative efficacy of the individual components of PE (imaginal and in vivo exposure). To our knowledge there is only one study that included an imaginal exposure only condition and met the other inclusion criteria (
Bryant et al., 2003). Although there was only one study, it is interesting to note that the controlled effect size for imaginal exposure only was similar in magnitude to our overall findings (
g = 0.83).
Second, the current analysis did not test the effectiveness of PE compared to pharmacological treatments. However, existing results suggest that the effect of pharmacotherapy for PTSD is significantly less than the effects observed here for PE. For example, a meta-analysis of nine randomized placebo-controlled pharmacotherapy trials found an effect size of 0.41 for PTSD symptoms. Even the medication (the selective serotonin reuptake inhibitor fluoxetine) with the highest effect size at 0.65 was not of the same magnitude as the result found for PE (
Penava et al., 1996).
Third, several of the studies were carried out by the same research group (i.e., Foa et al.). This raises the question of whether findings are similar when this type of treatment is implemented by different groups of researchers. We chose to examine this question empirically. Analysis showed that effect sizes were not significantly different between Foa’s group and other researchers (p = 0.47). Unfortunately data were not available to further determine the effects of gender or chronicity.
Finally, the follow-up analyses included fewer studies (7 vs. 13) and patients (348 vs. 675 for primary outcome measures) than the posttreatment analyses because many of the studies did not include a follow-up assessment. It is crucial to know whether the substantial posttreatment gains are maintained over time, and therefore it is encouraging to see a substantial effect size at follow-up. However, analyses that include fewer patients result in a loss of statistical power and therefore a less reliable estimate of the treatment effect size. Hopefully, future studies will include follow-up assessments such that subsequent meta-analyses can confirm the long-term effectiveness of PE for PTSD.
4.3. Summary and Conclusions
In sum, the results show that PE is highly effective in treating PTSD, and significantly more effective than inactive (waitlist) and active (psychological placebo) control conditions. In fact, the average PE treated patient fared better than 86% of patients in the control conditions. These findings are in marked contrast to the conclusions of
Benish et al. (2008) and suggest that the efficacy of exposure treatments for PTSD cannot be attributed solely to non-specific factors. Consistent with prediction (and with the Benish et al. findings), there was no significant difference between PE and other active treatment conditions (CPT, EMDR, CT, and SIT). PE effectively treats both PTSD-specific distress as well as more general trauma-related distress (e.g., depressed mood), and the benefits are dramatic and enduring. The large effect sizes support the status of PE as the first line treatment-of-choice for PTSD.