Methods
Participants
Individuals were eligible for participation in the study if they had a terminal prognosis with a life expectancy of 6 months or less, according to their treating physician; were receiving palliative care in a hospital or community setting (hospice or home) through an affiliated recruitment site in Canada, USA, and Australia; were aged 18 years or older; were willing to commit to three or four contacts over about 7–10 days; and were able and willing to provide written informed consent. Patients were excluded if they were delirious or otherwise cognitively impaired (based on clinical consensus and post-randomisation Blessed Orientation Memory Concentration test),
8 too ill to complete the requirements of the protocol, or unable to speak and read English.
This trial was coordinated by the Manitoba Palliative Care Research Unit at CancerCare Manitoba, Winnipeg, MB, Canada. Other participating centres were Curtin University, Perth, WB, Australia, and Memorial Sloan Kettering Cancer Center, New York, NY, USA. Approval was obtained from the ethics committees of all participating centres. All participants provided written informed consent.
Randomisation and Masking
After providing consent, all participants were randomly assigned in a 1:1:1 ratio to one of three study groups— dignity therapy, standard palliative care, or client-centred care—and asked to complete baseline psychosocial questionnaires. The study statistician used a computer-generated table of random numbers in blocks of 30 to allocate patients. Allocation concealment was by use of opaque sealed envelopes. The envelopes were sent to each site and opened sequentially by study staff after consent had been obtained from the patient. To avoid any possible response bias or contamination, research staff with whom the participant had no previous contact administered the final psychometric battery of questionnaires. Recordings from the dignity therapy and client-centred care groups were reviewed by the study coordinator to ensure protocol adherence and prevent cross-contamination.
Study Groups
Dignity therapy was provided by a psychologist, psychiatrist, or experienced palliative-care nurse. All therapists took part in a 3-day training workshop, led by the principal investigator (HMC). Continuous supervision of the therapy was provided by the site investigator (HMC, LJK, WB), initially for every case and then varied, until each therapist was fully competent. Group supervision, led by the principal investigator, took place every 6–8 weeks throughout the study, with videoconferencing to connect all three study sites. The principal investigator also reviewed a random sample (about one in six) of transcripts from all study sites to identify any difficulties or therapeutic improvements. Feedback from this review was offered either individually or, when more broadly applicable, within group supervision.
Patients were shown the framework of questions for dignity therapy (panel 1) and asked to consider what they might wish to speak about during their session(s); this initial introduction to, and explanation of, dignity therapy took about 30 min. Within a few days, or as soon as a second meeting could be arranged, the therapist used the question framework to help elicit patients’ recollections, hopes, wishes for loved ones, lessons learned, and things they wanted remembered by those they were about to leave behind. Dignity therapy is flexible enough to accommodate participant’s preferences and choices about content, but the ethos of questioning targets those things that might enhance a sense of meaning, purpose, continued sense of self, and overall sense of dignity. All therapy sessions were audiotaped; these sessions usually took about 60 min. On completion, the audiorecording was transcribed verbatim and the transcript edited, to provide a clear and readable narrative. This transcript or generativity document was returned to the patient within about 4 working days from their previous session, read to them in its entirety to ensure that no errors of omission or commission needed to be addressed (this final session usually took about 30 min). The final version of the generativity document was given to the patient, to be passed along to a recipient of the patient’s choice, from whom follow-up data were later obtained (the effect of dignity therapy on family members given the generativity documents will be reported separately). At the conclusion of this session, participants were asked to complete a psychometric follow-up battery described in the outcome measurements section below. [Generativity or the ability to guide the next generation, encompasses how patients might fi nd strength or comfort in knowing that they will leave behind something lasting and transcendent after death]
Client-centred care is a supportive psychotherapeutic approach, in which the research nurse therapist guides the patient through discussions that focus on here-and-now issues—ie, participants are asked about their illness, associated symptoms, and what is being done to address their distress. The content of client-centred care was kept as distinct from dignity therapy as much as possible and did not focus on issues of generativity, meaning, or purpose. If these issues were raised, the therapist did not probe for additional detail, allowing the interview to gently return to illness-related inquiry. Although these sessions were audiorecorded for purposes of auditing protocol adherence, no permanent record of these conversations was provided to the patient or the patient’s family. The number of contacts for client-centred care and dignity therapy were identical, with the initial, middle, and final meetings designed to take about the same time in both groups. During the final meeting, 7–10 days later, the participants completed the psychometric battery.
Participants assigned to standard palliative care had access to the complete range of palliative-care-support services that were available to all study patients, including specialist palliative-care physicians and nurses (ie, experts in the management of pain and symptoms), social workers, chaplains, and psychologists or psychiatrists. No participating site provided a formal approach to addressing generativity issues; therefore, a programme similar to dignity therapy was not available to patients who were not randomly assigned to this group. Patients were asked to complete the battery of psychometric questionnaires as soon as they were assigned to standard palliative care and then 7–10 days later—a timeframe roughly corresponding to the time between the first and last contact in the other two study groups.
Outcome Measurements
The primary outcomes—reductions in various dimensions of distress—consisted of mean changes between baseline and end of intervention in measurements of psychosocial, spiritual, and existential distress. The primary measurements were the Palliative Performance Scale (for physical performance; 100%=healthy, 0%=death),
9 Functional Assessment of Chronic Illness Therapy Spiritual Well-Being Scale (spiritual wellbeing with two subscales— meaning or peace and faith),
10 Patient Dignity Inventory,
11 and Hospital Anxiety and Depression Scale.
12 We also administered items from the Structured Interview for Symptoms and Concerns,
13 including dignity, desire for death, suffering, hopelessness, depression, suicidal ideation, and sense of burden to others. Additional measurements were a two-item Quality of Life Scale
14 and an Edmonton Symptom Assessment Scale, modified to include a will-to-live visual analogue scale.
15 All scales were administered at baseline and immediately after study completion. Secondary outcomes, addressing to what extent the intervention might have affected the participants’ end-of-life experiences, were measured with a survey done after study completion, with detailed questions about their experience of participation in the study and how it had affected them and their family (for the questionnaire see webappendix pp 1–18).
Statistical Analysis
Analyses were done on all patients with available data at baseline and at the end of the study intervention. The data were summarised with standard descriptive measurements. Two group comparisons were undertaken—
t tests when the data approximated a normal distribution and Mann Whitney
U tests when the data were ordinal. Three group comparisons were undertaken by use of ANOVA when a normal distribution was reasonably approximated and Kruskal-Wallis tests when it was not. With an α set at 0·05, desired power set at 80%, and small-to-medium effect size with Cohen’s value for such an effect size of 0·15, the estimated recruitment target was 120 patients per group.
16 The effect size here refers to the standard deviation of the group means divided by the postulated common standard deviation. With three groups, an effect size of 0⋅15 would imply that at least one group mean is at least a third of a standard deviation away from the other two. SPSS (version 18.0) was used for the statistical analysis.
When a significant result was obtained in a multigroup comparison, the precise nature of the group differences was investigated with Tukey’s test (if ANOVA had been used) or a series of Mann-Whitney U tests (if the Kruskal-Wallis test had been used). Comparisons of before and after therapy were undertaken by use of the paired t test if the data were roughly normal or the Wilcox signed-rank test if they were not. All comparisons were done on a two-tailed basis. Since the number of comparisons was large and the risk of type 1 errors was increased, a probability of less than 0·01 was prespecified as the minimum acceptable designation of significance.
Role of the Funding Source
The funders had no role in the study design, data collection, analysis or interpretation of the data, or in writing the final report. The corresponding author had full access to all the data and final responsibility to submit for publication.
Results
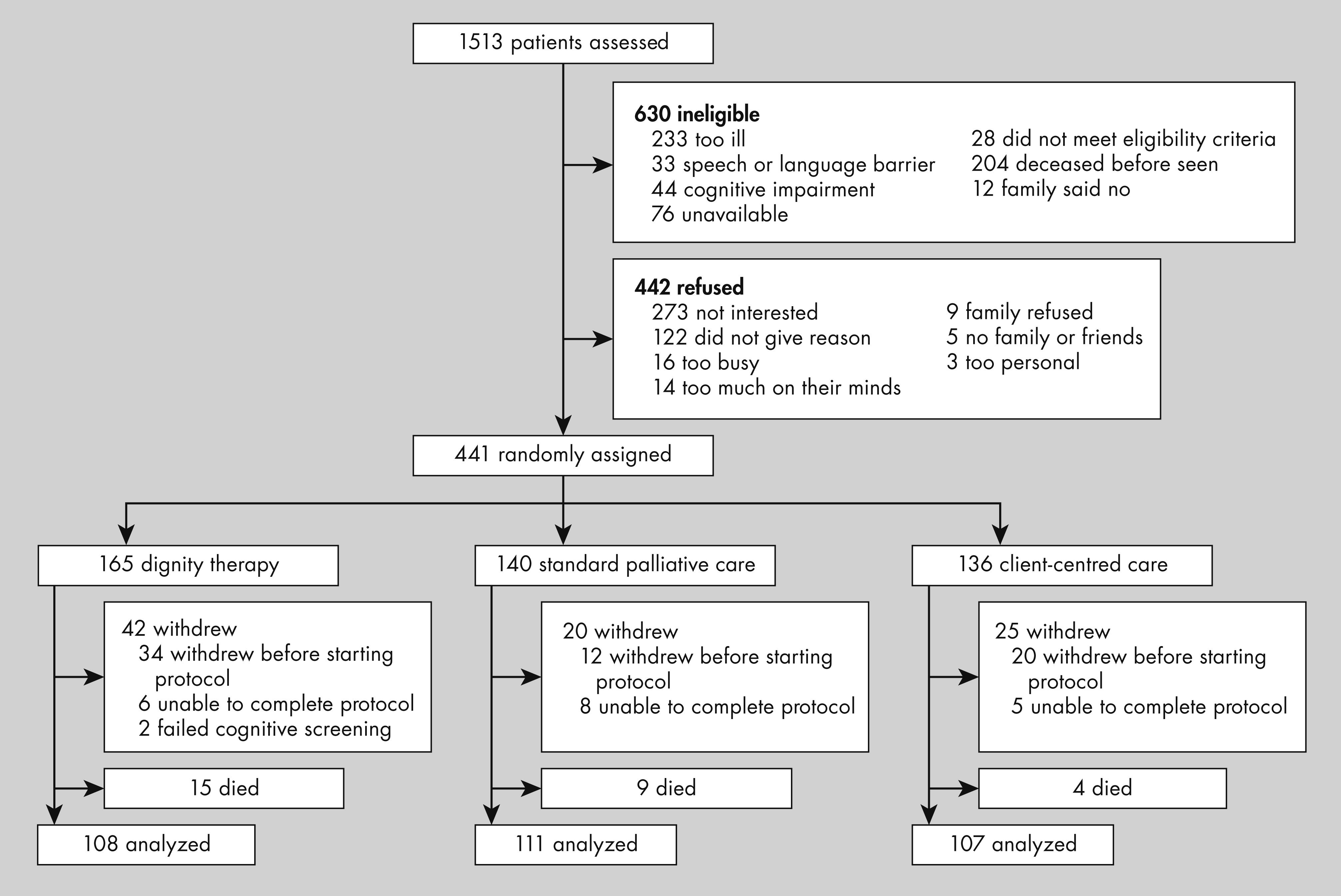
The figure shows the trial profile. 1513 patients were assessed for eligibility by use of a consecutive sampling approach between April, 2005, and October, 2008. After randomisation, 28 patients died, 85 withdrew because of declining health, and two failed Blessed Orientation Memory Concentration screening. These individuals were excluded from the analysis because we had either no or only incomplete data for them. Therefore, 326 participants—108 (33%) assigned to dignity therapy, 111 (34%) to standard palliative care, and 107 (33%) to client-centred care—completed the study. Recruitment was fairly even across the three study sites (Winnipeg [n=119], Perth [n=99], and New York [n=108]), with the number of participants at each site balanced across the study groups.
Table 1 shows that the baseline demographic characteristics of participants assigned to the three groups were well balanced. 161 (49%) of 326 participants were men (
table 1). The mean age of the participants was 65⋅1 years (SD 14⋅4; range 22–102). 192 (59%) participants were married or living in common-law partnerships, and the rest were widowed, divorced, or not married. 138 (42%) were living with their spouse or partner, 86 (26%) were living alone, 70 (21%) were living with children, and the rest were living with others, such as friends or other relatives. 196 (60%) were receiving home-based palliative care, 72 (22%) palliative care in an inpatient unit, 31 (10%) acute care in an inpatient unit (followed by palliative care on a non-palliative-care unit), and 27 (8%) freestanding hospice care. 68 (21%) participants were Protestant, 86 (26%) Catholic, 43 (13%) Jewish, 51 (16%) Anglican, 43 (13%) other, 33 (10%) no religious affiliation, and two individuals did not provide an answer to the question about religious affiliation. 30 (9%) individuals had less than high school education, 107 (33%) had completed high school, and 188 (58%) had completed college or postgraduate training (one individual was unable to answer). Cancer sites were gastrointestinal (108 [33%]), genitourinary (26 [8%]), lung (48 [15%]), breast (29 [9%]), gynaecological (11 [3%]), miscellaneous solid tumours (67 [21%]), haematological (14 [4%]), and brain (nine [3%]), and 12 [4%] patients had non-malignant terminal illness (ie, end-stage organ failure and amyotrophic lateral sclerosis). The mean Palliative Performance Scale rating for all participants at baseline was 44⋅3% (SD 15⋅1).
134 (41%) participants reported that they had lived with their life-limiting illness for less than 1 year, 104 (32%) for 1–3 years, and 88 (27%) for more than 3 years. The median survival time was 110 days (IQR <56 to <235); 213 [65%] patients had died by the time the study ended; the proportion of patients surviving in each of the study groups was not significantly different between groups (62 [57%] of in dignity therapy group, 78 [70%] of 111 in standard palliative care group, and 73 [68%] of 107 in client-centred care group; p=0·1). No difference was noted in the survival times after study completion between the three groups (81 days [IQR 48–249] in dignity therapy group, days [61–222] in standard palliative care group, and 128 days [67–233] in client-centred care group; p=0·51). Age and sex distribution, Palliative Performance Scale ratings, and dropout rate (death and withdrawal because of deterioration in health), in all three study groups showed no significant differences at completion of the study.
Because no initial threshold level of distress was stipulated as an entry criterion, the sample was most noteworthy for its paucity of distress at baseline (
table 2;
table 3). In most instances, patients were not greatly distressed, as indicated by the average Patient Dignity Inventory item scores and other baseline psychometric scores (
table 2;
table 3). Differences between before and after study measurements were calculated for Patient Dignity Inventory and Structured Interview for Symptoms and Concerns items, modified Edmonton Symptom Assessment Scale individual subscale scores, Quality of Life Scale, Functional Assessment of Chronic Illness Therapy, and Hospital Anxiety and Depression Scale; no significant differences were noted between the three groups (
table 2 and
table 3). The survey after the study, however, showed differences between the three study groups (
table 4). Patients given dignity therapy were significantly more likely than were those in either of the two other groups to report that the treatment was helpful to them, improved their quality of life, and sense of dignity (
table 4). The patients in the dignity therapy group, compared with the other study groups, were also significantly more likely to report that the study treatment changed how their family saw and appreciated them, and that it had or would be of help to their family (
table 4). Dignity therapy was significantly better than the client-centred care in improving spiritual wellbeing, and was significantly better than standard palliative care in terms of lessening sadness or depression; significantly more patients who had received dignity therapy reported that the study group had been satisfactory than did those who received standard palliative care (
table 4).
Discussion
Although floor effects precluded our ability to show significant differences between the study groups in terms of the primary outcomes, our secondary outcomes showed substantive benefits of dignity therapy, a novel psychotherapeutic approach, over standard palliative care and client-centred care. Patients in this group, when surveyed after the study, were significantly more likely to report benefits in terms of finding the treatment helpful, improving their quality of life, their sense of dignity, changing how their family saw or appreciated them, and helping their family than did those in the standard palliative care and client-centred care groups (panel 2).
Comprehensive palliative care requires that careful attention be paid to the physical, psychosocial, existential, and spiritual sources of end-of-life distress. Restricting the clinical focus on any of these domains to the exclusion of others does not achieve standards of palliative care as specified by WHO
20 and the US Institute of Medicine.
21 In describing factors associated with a good death, the Institute of Medicine includes preparation for death and opportunities for closure or sense of completion of the life.
21 Yet, although much progress has been made in our ability to achieve physical comfort for patients who are dying, few novel interventions have been designed to address the psychosocial, existential, and spiritual dimensions of end-of-life care.
Dignity therapy was developed for the purpose of lessening distress and enhancing end-of-life experience for patients nearing death. In our phase 1 trial,
6 nearly all patients reported that dignity therapy was helpful, whether they had disclosed substantial initial distress or not. On the basis of that finding, baseline distress was not specified as an entry criterion for the randomised controlled trial. Because the base rates of distress within our sample were quite low, it is perhaps unsurprising that we were unable to measure any significant changes in distress in the three study groups. Improvement in indicators of depression, will to live, and quality of life, presupposes that patients’ initially consider these a problem. In the absence of such initial distress, little room exists for improvement.
Perhaps the scales we used for assessment of our primary outcome were less responsive and less sensitive to changes than were those used for the secondary outcome, whereby patients reported their experiences in the survey undertaken after study completion. The difficulty in showing end-of-life psychosocial change with self-reported measurements has been well documented. Unlike a trial of chemotherapy, in which survival time, tumour load, and overall mortality provide readily measurable and objective outcomes, defining outcomes for dignity therapy is a greater challenge. Dignity therapy was designed to positively affect the experience of people who are dying. Measurements of overt distress, with indicators of psychosocial, existential, and spiritual effect, were incorporated into the study protocol. In a recent review of quality of life measurements that are suitable for use in palliative care, none of the items could be identified as having an established responsiveness to change.
22 The conclusion drawn from the results of a meta-analysis is that distress before the intervention is a critical moderator of efficacy of psychosocial interventions in patients with cancer.
23 Murray and colleagues
24 have suggested that a more successful approach might be to have serial qualitative interviews. This approach, however, would not be well suited to a randomised, controlled trial.
With the lack of significant difference for the three study groups for the primary outcome measurements, we also considered whether our trial might have been underpowered. A post-hoc power calculation, based on the actual number of trial participants, determined that with 326 patients, this study had a power of 0⋅72-0⋅95 to detect an effect size of 0⋅15-0⋅30.
Patients in the dignity therapy group were significantly more likely than were those assigned to the other groups to report that this approach was helpful, improved their quality of life, enhanced their sense of dignity, and provided benefits to their family. Although they reported their initial state of psychosocial or existential wellbeing as satisfactory, patients given dignity therapy often had an enhanced quality-of-end-of-life experience that they simply could not have expected. The effect, although difficult to assess, was often poignant and profound. For example, a 72-year-old woman with bowel cancer stated that “[dignity therapy] brought to the forefront that I have to prepare my family to the best of my ability”. A 56-year-old woman said, “Mostly I want my family to know that I’m okay with dying and they must move on”. She went on to say that “the therapy showed me I am not the cancer, I am still in here. I am so grateful for that because I lost myself….it really helped me remember who I am”.
With hindsight, the argument could be that we should have screened patients for some baseline critical distress. That might have improved the likelihood of showing differences, based on changes reported in the questionnaires before and after the intervention, in the three study groups. Our disinclination to do so, however, was based on previous findings, showing the beneficial effects of dignity therapy for nearly all patients nearing death, whether overtly distressed or not. Introduction of critical thresholds of distress for study inclusion would have excluded most patients who were most likely to participate in this study. Another consideration might have been a crossover study design, in which patients could experience and thus compare dignity therapy with other possible study treatments. However, such a design would not have been feasible, with many patients either deteriorating or dying before a comparison of the groups was possible.
Notably, of the 1513 patients who were assessed for eligibility, 42% were ineligible, mainly because they were too ill to take part in the study. Of the patients who met the eligibility criteria, half consented to participate, and nearly three-quarters of these completed the protocol. For palliative care protocols that require participants who do not have any cognitive impairment, this recruitment pattern is not at all atypical.
25 The nature of dignity therapy is such that only patients who are mentally capable of providing personally meaningful responses are those who will be approached to take part. Therefore, generalisability should be defined in terms of patients who maintain their cognitive capacity while they are nearing death. Although in this trial we mainly enrolled patients with cancer, the application of dignity therapy in non-cancer populations has been investigated in other studies.
26We are not aware of any instance in which patients withdrew from dignity therapy because of feeling upset or distressed. Many patients, however, indicated moments during therapy that were emotionally evocative—eg, talking about hopes or wishes for family members in anticipation of a time after their death. Mostly, however, patients appreciated the opportunity to articulate these issues. The only safety issue, which will be reported fully in a separate report of families’ experiences of dignity therapy, was that on a few occasions family members were dissatisfied with the generativity document. The family members felt the patient had become too ill to give fulsome responses, or that the answers provided a distorted image of the participant. Therefore, patients who are delirious or otherwise cognitively impaired should not be given dignity therapy.
Several studies have been done to assess dignity therapy under different circumstances. The conclusions drawn from a phase 1 Danish study
27 of ten health-care professionals and 20 patients was that, with minor cultural adaptations, dignity therapy was “a manageable, acceptable and relevant intervention for Danish patients admitted to palliative care”. The results of a pilot study of eight patients in rural Kentucky, USA, with end-stage cancer showed that dignity therapy could be delivered by videophone, and achieve overall benefit and high patient satisfaction.
28 In a phase 1 study of a cohort of 33 terminally ill patients that was done in French-speaking Canada, relevance and satisfaction were high for patients and their families.
29Despite the beneficial effects of dignity therapy, its ability to mitigate outright distress (eg, depression, desire for death or suicidality) has not yet been proven. Future research in more severely distressed patients might indeed establish its role in such circumstances. However, the purpose and potential benefit of individual psychotherapy for patients with advanced or terminal disease is not solely the symptomatic relief of stress.
30 Psychotherapy is also offered for the prevention of distress, promotion of wellbeing, and establishment of a sense of personal meaning and life purpose. Psychotherapeutic support can help patients cope with disappointments, process the reality of leaving behind loved ones, deal with feelings of sadness, loss, isolation, and a damaged sense of identity and personal value. It can also help patients consider personal priorities in terms of relationships, religious and spiritual beliefs, and deal with the urgency of resolving conflicts or achieve personally meaningful goals.
30–33 Palliative care must offer patients opportunities to engage in these complex issues, and dignity therapy is a means by which it might do so. Future research exploring the beneficial effects of dignity therapy will help to unravel the psychological, spiritual, and existential complexities for an individual facing death, and the best way to support patients with advanced and terminal illness and their families.