Case Vignette
Jessie Hartwell is a 28-year-old Caucasian female who was referred to you by her primary care physician for help with addressing issues of sleep disturbance and daytime somnolence.
She reported to you that she has been having trouble sleeping for much of the past year. “It started with trouble falling asleep. I would get into bed but just lie there and think and think and think. It was like hamsters running in an exercise wheel in a cage—I just couldn’t turn off my mind.” She described that her thoughts were a mixture of regrets about the past and worries about the future, mostly tied to financial concerns. She reported that she often experienced headaches for the first few hours after awakening, and had trouble with concentration and energy during the day. She had initially talked about this with her primary care physician 6 months ago, but the offer of a prescription for “some tranquilizer drug to zonk me out” was not acceptable to the patient at that time, and so she did not pursue prescription pharmacotherapy.
Jessie described that she had tried a number of interventions on her own. A friend from work had recommended she visit the local “health food” store, where the clerk suggested she try chamomile tea at the first visit, then valerian root, and then at subsequent visits to the store, “some Asian herbs” that she could not recall by name. She reported that each herbal preparation had “helped maybe a little” for a few nights, but then the perceived benefits had dissipated. In efforts to avail herself of what tools were accessible, she then tried drinking “a glass or two” of red wine about an hour before bedtime, and found that this initially helped her feel relaxed and tired, but then she would get a “second wind” when she finally got into bed. She reported that she would then watch shows on cable TV or stream shows online until 3 or 4 a.m., when she would finally “conk out” and then awaken when her alarm went off at 7 a.m. with the lights on and the video still running.
Consideration Point A
At this point in the patient’s history, your differential diagnosis includes
| A.1_____ | Major depressive disorder |
| A.2_____ | Insomnia disorder |
| A.3_____ | Generalized anxiety disorder (GAD) |
| A.4_____ | Substance-induced disorder |
| A.5_____ | Obstructive sleep apnea |
Vignette Continues
You probed for any evidence of mood or anxiety disorders, and the patient reported that she has been worried about financial stability for several years, but denied symptoms meeting criteria for a current major mood or anxiety disorder. She explained that she had been let go from a previous position as a shift manager in a “big box” store when they terminated one-third of their workforce. After a couple of months of job searching, she landed another job with another retailer and has been consistently employed since then. Some of her friends have not been as fortunate and have struggled to find employment.
As you inquired more about her history, she denied any prior times with experiences of depressive, manic or hypomanic symptoms, obsessive thoughts or compulsive behaviors, hallucinatory experiences, or delusional thoughts.
As you inquired about her early life history, you learn that the patient had an unremarkable childhood as the elder of two sisters who grew up in an intact family of origin. She was an average student in high school and attended 2 years at a local junior college, receiving an Associates degree in their business studies program before entering the workforce full-time.
The patient reported never using drugs of abuse or smoking tobacco. Her use of alcohol was limited to the two glasses of wine she consumed to try to address her sleep issues. She admitted to having a brief period as a “party animal” while in her early 20s, but since leaving college she denied having any blackouts or indiscretions while under the influence. She reported that she was casually dating but did not have a serious romantic partner.
In reviewing her medical history, the patient denied having major medical conditions. When you evaluated her, she reported taking no routine prescription medications but did endorse having taken the herbal products she mentioned earlier.
On examination, she was pleasant and cooperative with the interview and neatly and casually attired. There was mild psychomotor slowing noted. Eye contact was adequate. Speech was of slightly slowed rate, but normal prosody and volume. Affect was fatigued. Mood was endorsed as “worried about why I can’t sleep.” Thought process was generally linear and coherent but slightly sluggish. Thought content was without hallucinations, delusions, or current suicidal or homicidal intent. Cognitively she was awake, alert, and oriented to self, place, date, and circumstances. Memory registration was intact with 3/3 stimuli, and recall after delay was 3/3 items. She recalled the prior six U.S. Presidents without difficulty. Her similarities were abstract (apple/orange = “fruit”; watch/ruler = “measurement tools”). Insight was adequate in that she recognized she was not doing well and needed to receive professional help. Judgment currently was adequate, in that she was open to considering all options for treatment. Neurologically, gait-stride length was normal, as were arm swing and turning, and rapidly alternating movements. You detected no focal neurological deficits.
Consideration Point B
At this point, the recommendations you consider with this patient include which of the following:
| B.1_____ | Cognitive behavioral therapy for insomnia (CBT-I) |
| B.2_____ | Instruction about sleep hygiene |
| B.3_____ | Relaxation training |
| B.4_____ | Abstinence from alcohol |
Vignette Continues
After discussion of the options for treatment, the patient accepted your recommendation to start with treatment using CBT-I, as she still wished to pursue treatments that did not involve prescription psychotropics. She was eager to try the computerized CBT-I program that you recommended for her (
1). She also agreed to “try to cut back” on her evening consumption of wine.
After 2 weeks of this regimen, the patient reported that she was falling asleep more easily but that she continued to be very fatigued during the day. She reported yawning excessively and feeling great pressure to take a midafternoon nap. She had become worried that she might be viewed as a “slacker” at work; some of her closer friends at work joked with her that she “must have had a rough night last night” because of her visible drowsiness. When you probed for additional data, she acknowledged that she had increased her caffeine consumption to drinking up to six cups a day, along with two or three “energy drinks.” She sheepishly admitted that she was still tempted to have a drink or two of wine in the evening if she felt “too wired to sleep” by 9 p.m., and did this an estimated three nights in a week. Additional detailed history revealed that, although she was only modestly overweight (BMI 27), a previous boyfriend had joked that she “snored like a banshee.”
Consideration Point C
Given all the details of the case, your next therapeutic step(s) is/are
| C.1_____ | Recommend that she try a period without the use of any alcohol or caffeine |
| C.2_____ | Offer a prescription for a Federal Drug Administration (FDA)-approved GABA-A agonist hypnotic agent |
| C.3_____ | Recommend an over-the-counter sedating antihistamine agent |
| C.4_____ | Obtain polysomnography (PSG) data from a sleep study |
Vignette Concludes
The patient agreed to having a sleep study after being fully abstinent from alcohol and energy drinks for 2 weeks, and reducing her coffee to one cup a day, consumed before 10 a.m. This change improved her daytime energy somewhat, but she still felt a degree of daytime somnolence.
The PSG study revealed that she was having numerous apneic events during the night, with frequent episodes of desaturation (pO2<90%), brief arousals by EEG, and disrupted sleep architecture. She was sufficiently impressed by the quantitative information about her sleep disturbance that she agreed to a trial of continuous positive airway pressure (CPAP) therapy. She used the device as directed and within 2 weeks of nightly use reported that her daytime energy and alertness had meaningfully improved.
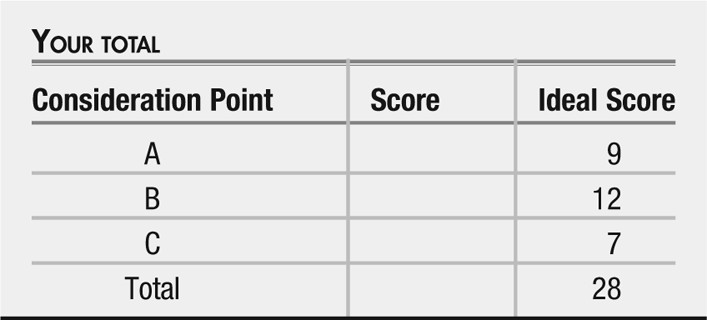
Answers: Scoring, Relative Weights, and Comments
Consideration Point A
| A.1_____ | (+1) Major depressive disorder. While sleep disturbance is one of the DSM–V criteria for major depressive disorder (2) this patient did not yet endorse other core symptoms, such as depressed mood or anhedonia, as central to her presentation. |
| A.2_____ | (+3) Insomnia disorder. In DSM–V, the conceptualization of primary and secondary insomnia has evolved into insomnia disorder, which may be accompanied by comorbidities (2). This patient has endorsed insomnia and may or may not have other related conditions. |
| A.3_____ | (+2) Generalized anxiety disorder (GAD). Difficulty falling or staying asleep, or restless unsatisfying sleep, can be a core symptom for some patients with GAD (2). |
| A.4_____ | (+2) Substance-induced sleep disorder. Withdrawal from sedating substances and acute exposure/intoxication with stimulants can make it difficult for individuals to fall and stay asleep (2). |
| A.5_____ | (+1) Obstructive sleep apnea (OSA). Patients with obstructive sleep apnea experience periods when they stop breathing while asleep, due to mechanical obstruction of the airway, and may experience symptoms including daytime sleepiness, headaches, and dry mouth or throat (3). |
Consideration Point B
| B.1_____ | (+3) CBT-I. Cognitive behavioral therapy for insomnia is an evidence-based treatment for insomnia (4). |
| B.2_____ | (+3) Instruction about sleep hygiene. Education about optimizing a person’s daily routine to promote good sleep can include elements such as making the bedroom a dark, quiet, and cool place reserved primarily for sleeping (not work, study, and/or arguments), and following a prebedtime calming routine (4). |
| B.3_____ | (+3) Relaxation training. Different methods can be employed to relax both mind and body in preparation for sleep, and can be practiced throughout the day, not just at bedtime (4). |
| B.4_____ | (+3) Abstinence from alcohol. Alcohol may worsen insomnia (4). |
Consideration Point C
| C.1_____ | (+3) Recommend a period without alcohol or caffeine. Both alcohol and caffeine can worsen insomnia and can also interfere with the interpretation of PSG findings (4). |
| C.2_____ | (+2) Prescribe a hypnotic agent. The FDA has approved a number of agents for time-limited use as a hypnotic agent to promote sleep and treat insomnia (5). |
| C.3_____ | (0) Prescribe an antihistaminic agent. Although some histamine-blocking agents such as diphenhydramine are sedating, and are included in over-the-counter agents for the short-term use in promoting sleep, tolerance may develop with time and they may impair cognition, affect urinary retention, and worsen glaucoma (6, 7). |
| C.4_____ | (+2) Obtain polysomnographic PSG data. A sleep study can provide objective, quantitative information about sleep architecture, arousals during sleep, movements during sleep, and other physiologic aspects of sleep (3, 8). |