Comorbidity in Hoarding Disorder
A recent review commissioned by the DSM-5 Anxiety, Obsessive-compulsive Spectrum, Post-traumatic, and Dissociative Disorders Work Group recommended the addition of Hoarding Disorder (HD) as a separate diagnostic entity.
[1] Hoarding is characterized by excessive acquisition of and difficulty discarding possessions, resulting in severely cluttered living spaces.
[2] It has a high prevalence rate of 2–5%,
[3–5] and the resulting cluttered home environment can lead to health code violations, eviction, fire, family strain, significant cost to the community, and even death.
[6]Because hoarding has previously been considered a subtype of obsessive–compulsive disorder (OCD), much of the research on hoarding has used samples drawn from patients seeking treatment at OCD specialty clinics. However, reviews of accumulating evidence have led to conclusions that the two are distinct disorders.
[1,7] As most large sample studies are of hoarding within the context of OCD, our understanding of the diagnostic placement and comorbidity of hoarding is limited. To underscore this concern, in the few studies in which participants were solicited for hoarding rather than OCD symptoms, non-hoarding OCD was diagnosed in only a small number of cases.
[5] Because of the small number of cases in these studies, the prevalence of OCD in people with HD is not yet clear.
An additional limitation in the research on hoarding is the reliance on inadequate definitions and measures of the construct.
[8] Not surprisingly, the variability in assessment has resulted in wide variability in reported comorbidities. Several studies failed to find increased risk for any axis I disorder in OCD patients who reported hoarding,
[9,10] whereas the majority of studies have shown increased comorbidity for selected disorders.
Recent advances in definition
[1] and measurement
[11,12] provide the ability to more reliably diagnose and assess comorbidity in HD; however, studies using these improved assessment strategies have used small samples. The majority of studies of hoarding comorbidity have reported very high rates of depression, often significantly greater than among OCD comparison groups.
[13–21] Hoarding behaviors have been observed in anxiety disorders other than OCD, especially generalized anxiety disorder (GAD) and social phobia.
[22] Among hoarding patients with OCD, rates of these disorders have exceeded non-hoarding OCD in some studies,
[16,18,19,23] whereas the opposite pattern has been found in studies of patients solicited for hoarding and not OCD.
[13,20] Interestingly, Pertusa et al.
[17] reported higher rates of GAD in OCD cases (with or without hoarding) compared to HD cases without OCD, whereas higher rates of social phobia occurred in all HD cases, regardless of accompanying OCD. That is, GAD seemed more strongly associated with OCD, whereas social phobia was more strongly associated with hoarding. Despite apparently elevated rates of traumatic events in hoarding cases,
[15,24,25] rates of comorbid posttraumatic stress disorder (PTSD) among patients reporting hoarding have been equal to or lower than rates for other anxiety disorders in most studies, ranging from 0 to 23%.
[13,15,17]Hoarding has been thought to be associated with impulse control problems, particularly those characterized by acquisition such as compulsive buying, kleptomania, and the excessive acquisition of free things.
[4,26] Frost et al.
[26] found that over half of hoarding cases had clinically significant compulsive buying, and when the tendency to excessively acquire free things was included, 86% had at least moderate acquisition problems. Similarly, Mueller et al.
[4] found that nearly two thirds of hoarding individuals suffered from compulsive buying. To date, however, there are no data on acquisition problems in a large, carefully diagnosed sample of people with HD. Although kleptomania has been reported anecdotally among people with hoarding problems
[27] and found to be associated with hoarding behaviors in a nonclinical sample,
[28] as yet, no data have linked the two clinical conditions. Rates of attention deficit-hyperactivity disorder (ADHD) among hoarding samples have exceeded that of nonclinical groups
[29,30] and often exceeding that of people with OCD and other clinical comparison groups.
[29,31] Tolin and Villavicencio
[32] reported that inattentive ADHD symptoms, but not hyperactivity, predicted severity of hoarding after controlling for negative affect.
Hoarding has been associated with a wide variety of personality disorders as well. The most frequent finding has been that hoarding is associated with obsessive–compulsive personality disorder (OCPD), and in some cases even when the hoarding criterion is excluded.
[5,16,18,19,23] However, studies using hoarding samples not drawn from OCD patients have failed to find elevated rates of OCPD when the hoarding criterion was excluded.
[17,33] Other personality disorders have sometimes, but not routinely, been found to be associated with hoarding.
Reports of gender differences in hoarding comorbidity have been mixed. Labad et al.
[34] found no gender differences in hoarding frequency among OCD patients, whereas Wheaton et al.
[21] reported greater OCD symptom severity among women with versus without hoarding, although no such differences emerged among men. In contrast, Samuels et al.
[23] found higher frequencies of most types of obsessions and several compulsions in men with hoarding-related OCD compared to men with non-hoarding OCD. Among women, only symmetry obsessions and ordering compulsions were more frequent in hoarding than non-hoarding OCD patients. No studies have reported on gender differences in samples recruited for hoarding. Because of the inconsistencies in the findings and the narrow population from which these samples were drawn (OCD patients), no clear hypotheses regarding gender can be made with respect to comorbidity.
This study employs the largest sample to date of participants solicited solely for hoarding symptoms and using diagnostic criteria for HD that match those currently proposed for DSM-5.
[1] This study also solicited participants regardless of their interest in treatment and utilized well-validated measures of hoarding and other symptoms. Comorbidity was compared across participants with HD and participants with OCD without hoarding. Based on previous research, we predicted that:
1.
A minority of individuals with HD will be diagnosed with OCD.
2.
Major depressive disorder (MDD) will be the most frequent diagnosis in both groups and significantly more frequent in HD than OCD participants.
3.
GAD and social phobia will be diagnosed in HD participants at least as frequently as OCD.
4.
Frequency of traumatic events but not PTSD will be greater among HD than OCD participants.
5.
Acquisition-related impulse control problems (compulsive buying, excessive acquisition of free things, kleptomania) will be more frequent in HD than OCD participants.
6.
Inattentive ADHD, but not hyperactivity, will occur more frequently in HD than OCD participants.
7.
OCPD will occur more frequently in HD than OCD, but not when the hoarding criterion is removed.
No gender differences were hypothesized, but exploratory analyses of gender were conducted.
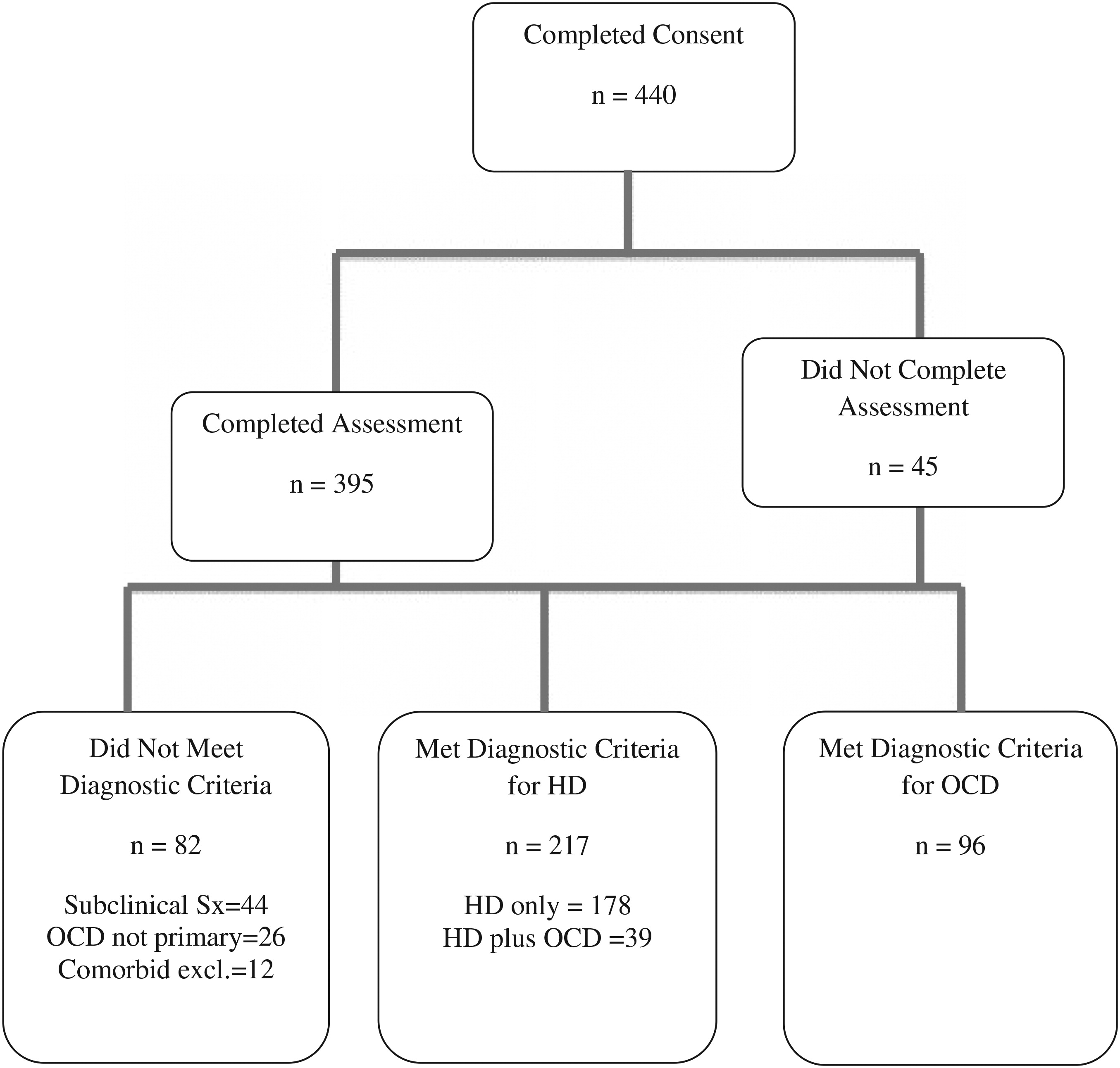
Results
Hoarding Severity
t-tests conducted on SI-R scores indicated that, as expected, the HD group had significantly higher scores than did the OCD group on each subscale as well as the total score (
Table 1). The mean SI-R total score of the HD group was comparable to other studies involving clinically significant hoarding cases
[11] and well above the clinical cutoff
[8].
Frequency of OCD in HD
Among the 217 HD participants, only 39 (18.0%) met criteria for OCD, although this varied by gender. Only 15.0% (25/167) of women with HD met criteria for OCD, whereas 28.0% (14/50) of men did so (χ2 = 4.43, P = .035).
Axis I Diagnoses: Frequency and Comparisons of HD Versus OCD by Gender
Table 2 presents comparisons of the frequency of diagnoses and odds ratios for HD and OCD participants by gender. As predicted, MDD was the most common diagnosis among HD participants, occurring in 50.7% of the sample, and was more frequent in HD than OCD participants. The frequency did not differ by gender. No other mood disorder was significantly related to group status.
Because the younger age of the OCD group may mean they had less opportunity to develop MDD, we conducted additional analyses. First, there was no age difference between participants with or without an MDD diagnosis, t (311) = 1.03, P>.05, as would have been expected if sample differences were accounted for by age. Second, the MDD frequencies in HD participants exceeded the OCD group frequencies in each decade of life (ages 21–30: 42.9 versus 21.9%; 31–40: 53.8 versus 47.4%; 41–50: 64.3 versus 46.2%; > 50: 45.3 versus 29.4%). Furthermore, the frequency of MDD among the oldest group of HD participants (n = 139 over age 50) was lower than the frequency found among the younger 41 to 50-year-old age cohort (n = 56; χ2 = 5.75, P =.017).
Social phobia (23.5%) and GAD (24.4%) were the most frequently diagnosed anxiety disorders among HD participants; no one in the HD group was diagnosed with panic disorder. Overall, HD and OCD participants did not differ in the frequency of any specific anxiety disorder other than panic disorder. With regard to gender differences across the clinical samples, however, men with HD were more likely to be diagnosed with social phobia than were men with OCD (28.0 versus 11.8%; χ2 = 4.19, P = .041), but no such difference emerged among the women (22.2 versus 28.9%; χ2 = 0.89, P>.05). This difference appears to be due to the lower frequency of social phobia among men with OCD. Within the HD sample, men and women with HD did not differ in the frequency of social phobia (χ2 = 0.73, P>.05).
As expected, HD and OCD participants did not differ in the frequency of PTSD diagnoses, whereas HD participants were significantly more likely to have experienced a traumatic event than OCD participants (49.8 versus 24.4%; χ2 = 16.1, P<.001), as well as more likely to have experienced a trauma during childhood (32.8 versus 20.9%; χ2 = 4.1, P≤.042).
HD participants were no more likely than were OCD participants to have a comorbid anxiety disorder, and no more likely to have an anxiety and/or mood disorder.
Table 3 displays current comorbidities for MIDI impulse control disorders by gender. As expected, HD participants were more likely than OCD participants to be diagnosed with acquisition-related impulse control problems, specifically compulsive buying, acquiring free things, and kleptomania. Although the odds ratios for MIDI acquisition disorders appeared greater for men than women, none of these relationships varied significantly by gender. However, more women than men met criteria for compulsive buying for both groups combined (55.3 versus 27.0%, χ
2 = 21.8,
P<.001), and for HD participants (64.8 versus 48.0%; χ
2 = 4.54,
P = .033). Overall, 78.3% (166/212) of HD participants met criteria for one or more acquisition-related impulse control problems (buying, free things, kleptomania); 40.1% (85/212) met criteria for two such problems, and 6.1% (13/212) met criteria for all three. However, HD participants did not display a higher frequency of any other impulse control disorder than did OCD participants.
HD participants were significantly more likely than OCD participants to meet criteria for the inattentive subtype of ADHD (
Table 3). This difference did not vary by gender. As expected, there was no difference between HD and OCD participants in the frequency of hyperactivity, although Cochran’s χ
2 approached significance (
P = .051), with HD participants more frequently having this subtype. This also did not vary by gender.
Personality Disorders in HD and OCD Participants
The frequency of OCPD differed significantly by group, diagnosed in 29.5% of HD participants and 16.7% of OCD participants (χ2 = 4.85, P = .028). However, as hypothesized, when hoarding was removed from the criteria, the two groups did not differ (18.4 versus 14.6%, χ2 = 0.40, P>.05). Only 2 other personality disorders had frequencies greater than 4%. Avoidant personality disorder was diagnosed in 8.8% of HD and 6.2% of OCD participants (χ2 = 0.14, P>.05), and borderline personality disorder was diagnosed in 5.4% of HD and 3.3% of OCD participants (χ2 = 0.54, P>.05). A comparison across groups on the presence of any personality disorder was not significant (χ2 = 0.15, P>.05). No differences by gender occurred in any personality disorder analyses.
Comparison of HD Participants with and without OCD
A comparison of HD participants with and without OCD revealed few significant differences. There were no differences in severity of hoarding on the HRS-I (t(216) = −0.33, P>.05, or on the SI-R total, t(198) = 0.96, P>.05. However, the HD plus OCD group had a higher proportion of men than did the HD only group (36 versus 20%; χ2 = 4.43, P =.035). The only other difference was a higher frequency of pyromania in the HD plus OCD group than the HD only group (6.3 versus 0.0%; χ2 with continuity correction n = 5.0, P = .025). However, given the small number of cases (2 versus 1) and the large number of comparisons made, this difference should be viewed cautiously.
Discussion
As expected, relatively few HD participants (<20%) were diagnosed with OCD. In fact, several other disorders (MDD, GAD, social phobia) were more frequent among HD than OCD cases. This finding accords with recent research suggesting that hoarding is not a subtype of OCD, but instead a distinct condition related to a variety of disorders.
[1] Furthermore, the low rate of OCD in HD argues that studies of hoarding that recruit from OCD clinics will not represent the majority of people with HD. It should be noted, however, that the rate of OCD in hoarding (18%) is considerably greater than in the general population (1–2%), which suggests that although hoarding may be distinct from OCD, it is still related to it.
Men with HD were diagnosed with OCD nearly twice as often as women. Because there were few men in this sample, and the possibility that HD is more frequent in men than women,
[5] some caution is warranted with respect to this finding. Nevertheless, this gender difference deserves further scrutiny.
There were no differences between HD participants with and without OCD in the severity of hoarding symptoms, and the comorbidity pattern was similar. The higher frequency of men with both disorders deserves further study.
As hypothesized, MDD was the most frequent comorbid condition among HD patients, with more than half the sample receiving that diagnosis. Further, MDD was significantly more common in the HD than the OCD group, and age differences between groups did not appear to account for this finding. Although less frequent, GAD and social phobia were diagnosed in about one quarter of HD cases, similar to rates in the OCD sample. Accordingly, it is not surprising that the frequency of these disorders fall well within the ranges reported for HD participants recruited from both OCD and independent hoarding samples in previous research. Although men with HD were diagnosed with social phobia more frequently than women with HD (28 versus 22%), the significant interaction between group and gender appears to be due to the much lower frequency of social phobia in men versus women with OCD (11 versus 22%). Whether social phobia plays a role in the apparent social isolation and low marriage rate of many people who hoard
[13] merits attention in future research.
As predicted, the overall rate of PTSD was not higher in HD, but HD participants were more likely to have experienced any traumatic event as well as a traumatic event in childhood than were OCD participants. These findings are consistent with the reports of more frequent traumatic life events among people with OCD who hoard,
[5,21,24] and with Landau et al.’s
[15] finding of elevated traumatic life events among people recruited for hoarding. Nearly 50% of HD participants reported experiencing a traumatic event. Whether this was due to a lower threshold for defining trauma or an actual difference in life experience is not clear. If the latter, perhaps possessions buffer the development of full blown PTSD, consistent with reports by people who hoard that possessions are sources of comfort and security.
[2]As anticipated, more HD than OCD participants met criteria for compulsive buying, excessive acquisition of free things, and kleptomania. This is consistent with recent findings that well over 80% of people with self-reported hoarding problems acquire excessively.
[26] These may not be comorbidities, but rather part of the hoarding phenotype itself. However, at present, excessive acquisition is not included among required criteria for diagnosing HD.
[1] Nonetheless, these acquisition-related impulse control problems must be addressed during treatment. Although the odds ratio of MIDI acquisition disorders (especially compulsive buying) appeared greater for men than women, there were no gender effects. The lower odds ratio in women may need further exploration, but may be due partly to the fact that compulsive buying was relatively common for women with OCD (21%) compared to men with OCD (6%). Compulsive acquisition has been found to be associated with OCD symptoms in largely female samples.
[26] Perhaps it is less so for males. This is the first investigation to find elevated levels of kleptomania among people who hoard. With a base rate of nearly 10%, assessing kleptomania and stealing in HD clients is important for developing an effective treatment plan that prioritizes reduction of this dangerous behavior. Previous research has suggested an association between hoarding and pathological gambling.
[42] The absence of a difference in this study may be due to the use of a clinical (OCD) rather than a nonclinical comparison group as OCD has also been found to be associated with increased pathological gambling.
[42]Overall axis I comorbidity was high among HD participants as nearly 75% had a mood and/or anxiety disorder, although this rate did not differ from that for OCD participants. The high frequency of these conditions raises questions about the role of anxiety and depression in HD. Do they result from the significant burden and impairment produced by hoarding behavior
[6]? Or do anxiety disorders and depression predate hoarding and play a role in its development? Examination of the timing of the onset of HD versus comorbid conditions was beyond the scope of this paper, but is important for understanding the determinants of hoarding.
Consistent with our hypothesis, inattentive ADHD was significantly more frequent in HD than in OCD, evident in nearly 30% of HD participants. Attention problems have been hypothesized to be among information processing deficits that may underlie hoarding,
[2] but these findings make it clear that, although frequent, attention deficit is not a universal characteristic.
As hypothesized, OCPD was more frequent in HD than OCD, but when hoarding was omitted from the criteria for OCPD, samples did not differ. Overall, there were no differences between the HD and OCD groups on frequency of any other personality disorders. However, even when hoarding was removed as a criterion, OCPD was the personality disorder most characteristic of HD, occurring more than twice as often as the next most common PD.
There are several limitations to this study. As for much of the research on hoarding, many more women than men participated in the HD group, a difference not evident in the OCD group. The small number of HD men contrasts sharply with epidemiological findings suggesting that hoarding is more common among men than women in the general population.
[3,5] Perhaps the slightly higher rate of social phobia among men with HD explains why they do not volunteer to participate in research studies. A second limitation was that the HD group was significantly older than the OCD group. This is also characteristic of much of the research on participants solicited for hoarding. Nevertheless, the difference may have influenced some comparisons in this study. Additional research clarifying age of onset of these comorbidities will help determine whether the age difference played a role in the findings. Also, although there was no difference between groups on referral sources, it is possible the separate recruitment of HD and OCD participants introduced some bias that may have influenced the findings. Finally, our measures of ADHD relied on self-report rather than information gained from a diagnostic interview.