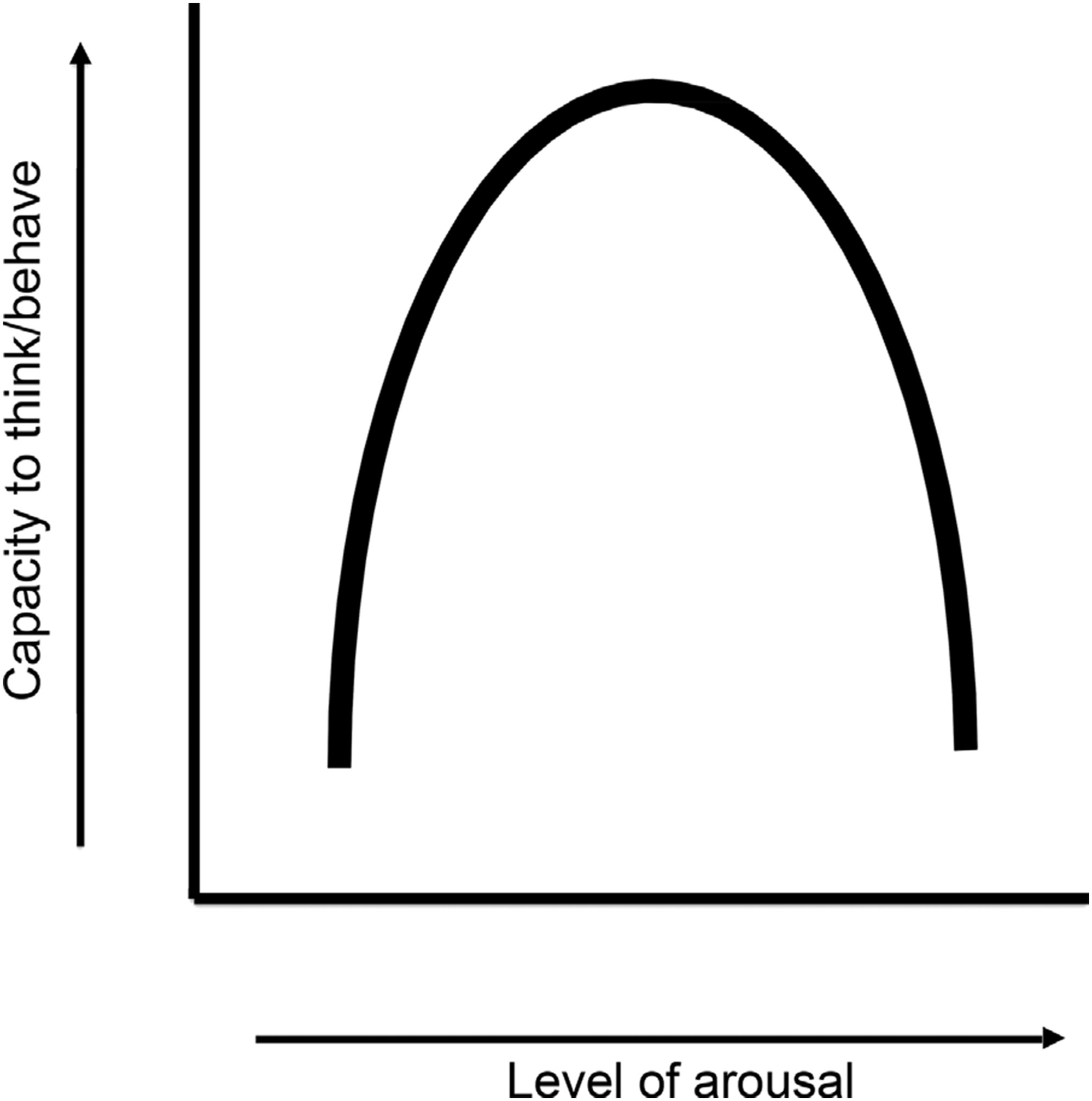
Posttraumatic stress disorder (PTSD), as defined by the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, (DSM-V), is a trauma- and stressor-related disorder characterized by persistent re-experiencing of a previously traumatic event. Those suffering from PTSD make significant efforts to avoid thoughts, feelings, and events associated with the trauma, as well as experiencing increased levels of arousal in response to generally neutral stimuli. Under normal circumstances, optimization of arousal follows an inverted “U”-shaped curve in its relationship to capacity to think critically and behave in an adaptive manner (
Fig. 1).
The chronic state of over-arousal experienced by those with PTSD results in elevated physiologic responses (ie, hypervigilence, exaggerated startle), diminished ability to control emotional reactions, and emergence of negative affective states and cognitions. Many individuals with PTSD will use substances such as alcohol, cannabis, and opiates in an attempt to reduce this chronic state of hyperarousal. This review will focus on two of these substances—alcohol and opiates, because they have FDA approved pharmacothera-pies. Among the larger number of substances with no FDA approved pharmacotherapies, we will review cannabis, because it is the most common of these substances, is being increasingly legalized, and has been considered by some to be itself a pharmacotherapy for PTSD. Continued use of these substances often leads to development of substance use disorders (SUD). Of note, individuals with SUD are also at greater risk for developing PTSD, presumably because of increased exposure to traumatic and/or stressful events as a consequence of the SUD lifestyle. These lifestyle factors include overdoses, deaths of friends, victimization, HIV exposure, sexual assaults and the violence associated with obtaining illicit drugs and with the dis-inhibition of violence associated with alcohol. Those patients suffering from both PTSD and SUD experience a unique set of challenges, and the treatment of these co-occurring disorders has been an important area of clinical study and focus. This review article examines the epidemiology of comorbid PTSD and SUD, and considers their shared neurobiological features in discussing potential options for pharmacologic management. An important aim would be to find single medications that would treat both PTSD and SUD since this would reduce potential side effects from medication interactions of polypharmacy and improve medication adherence by needing only a single medication.
The review began with a PUBMED search of the literature on the combination of PTSD and SUD in humans. We did not cover the animal models of PTSD or SUD for the neurobiology or potential pharmacotherapy of these disorders, and the epidemiology clearly only involves humans. Within the human literature, we covered both civilian and military trauma studies, but this trauma setting distinction confounded other differences in duration of PTSD and sex differences. Military PTSD pharmacotherapy was overwhelmingly in men with chronic PTSD, while civilian PTSD was predominantly in women with acute PTSD. Thus, sex or PTSD duration differences in treatment response were confounded by this military versus civilian setting distinction. Within the symptom clusters of PTSD we focused on hyper-arousal rather than other clusters such as numbing and detachment, because these other clusters have had a more limited focus in the literature and tend to be associated with the less pharmacologically responsive chronic rather than acute PTSD.
Epidemiology of PTSD and SUD
Several major epidemiological studies have documented the comorbidity of PTSD and SUD. In an early survey, Cottler et. al. found that individuals meeting criteria for DSM-III diagnosis of any SUD were more likely to have experienced a traumatic event, as well as increased vulnerability to developing PTSD once exposed.
1 A later study found that approximately 42.5% of patients who receive inpatient substance abuse treatment also report a diagnosis of PTSD.
2 According to the National Comorbidity Survey, SUD were two to three times more likely to occur among individuals with lifetime PTSD.
3 Other studies estimate the lifetime prevalence of any SUD in community samples of persons with PTSD to be between 21.6–43%, in comparison with 8.1–24.7% in those persons without PTSD.
4 Interestingly, gender differences have been found across several non-veteran samples, where drug abuse appears to put women at greater risk than men for developing PTSD, suggesting that treatment may require gender specific approaches.
5In the veteran population, co-occurrence of PTSD and SUD remains a specific area of focus, and it has been estimated that approximately 20% of veterans who are receiving treatment services for PTSD through a Veterans Affairs (VA) medical center also struggle with a comorbid SUD.
6 Among combat veterans, the rates of SUD may be even higher. Early study suggested that as many as 75% of combat veterans with lifetime PTSD also met criteria for alcohol abuse or dependence; yet, more recently, a study conducted by the Rand Corporation in veterans diagnosed with PTSD upon returning from Iraq and Afghanistan confirmed high rates of SUD.
7 More specifically, binge alcohol abuse rates were 50%, twice the community rate for these young adult men. It was also found that tobacco use occurred in 50%, 2.5 times greater than community rates of smoking; and opiate abuse was detected in 9%, three times the community rates. Other SUD included inhalants, sedatives, and marijuana. These high SUD comorbidity rates showed no differences by gender, however, though the relative number of women in the Rand study was small.
Sequelae of PTSD and SUD
Independently, both PTSD and SUD are associated with poorer health outcomes. For example, heavy drinking and problematic alcohol use in men was found to increase the likelihood of going on to develop depression or other psychiatric illness, cognitive impairment, and risk of onset of functional impairment.
8 By extension, PTSD is also associated with functional impairment, including self-reports of diminished well-being and increased physical limitations.
9,10 As expected, presence of co-occurring PTSD and SUD further compromise health status. In a comparison of the health of SUD patients with and without PTSD, Ouimette et al. found that patients with co-occurring PTSD and SUD report more cardiovascular, neurological, and chronic physical symptoms, as well as poorer functional status and well being.
10In a meta-analysis of the FDA database of clinical trials evaluating new anti-anxiety medications, psychiatric disorders featuring prominent anxiety (note: PTSD was categorized as an Anxiety Disorder prior to DSM V, and was included in the sample) were associated with greater risk of suicide.
11 Interestingly, unique psychological factors that increase suicide risk in patients with anxiety disorders are the presence of depression and mental health-related impairments.
12Like those struggling with anxiety disorders, persons with SUD also experience increased suicidality, although studies differ in regards to the exact extent to which addiction elevates this risk, ranging from as low as twice to as great as 100 times the risk. It has been suggested that the risk of suicide among persons with SUD is on average 10 times higher than the general population (see review by Wilcox, Conner, and Caine [2004]).
13 Anecdotal evidence and more recent study suggest that co-occurring PTSD and SUD are associated with a greater risk of suicide. To date, however, no study has demonstrated a direct, causal relationship between these conditions. Any associations are likely mediated by a variety of factors, including at the least, the actual presence of PTSD symptoms and an individual’s level of distress tolerance.
14Neurobiology of PTSD and SUD
Acutely traumatic events, perceived as uncontrollable and/or threatening to the individual, result in activation of the hypothalamic-pituitary-adrenal (HPA) axis as well as locus coeruleus and the noradrenergic system.
15 These regions are connected with the amygdala and hippocampus, areas that mediate fear conditioning and memory consolidation, respectively. As a result, the experience, associated sensory stimuli, and emotional response (fear) become encoded, such that later exposure to a related cue triggers reactivation of the traumatic memories as well as anxiety/increased arousal. When an individual moves from an environment where these cues are signs of danger to an environment where they do not represent a threat, the mechanism of extinction is responsible for eliminating the conditioned responses (such as hyperarousal) to the trauma-related cues.
16 Thus, the conceptual model of PTSD as a disorder of fear conditioning and extinction can assist our understanding of the underlying neurobiological dysfunction observed in persons suffering from the illness.
In considering the potential pharmacological options for treatment of comorbid PTSD and SUD, it is helpful to review three salient features related to the neurobiology of the extinction mechanism as well as the associated brain areas. First, hyper-responsiveness to stimuli that are reminders of previous trauma appears to reflect amygdalar hyperactivity. Second, over-generalization of stimuli appears to reflect hippocampal dysfunction. Third, poor control of anger and failure to extinguish these behaviors seem related to medial prefrontal and anterior cingulate cortex dysfunction. In PTSD, then, failure of extinction means that conditioned aversive and unpleasant responses to relatively neutral cues (ie, driving a car, hearing a loud noise) do not decrease during repeated exposure, even when those cues are not followed by stressful or aversive consequences. Specifically, PTSD patients have an inability to extinguish conditioned fear responses and an inability to distinguish between dangerous and safe situations. Extinction is an active cortical process as demonstrated in cortical ablation studies.
17 These studies have shown that (1) acquisition of conditioned fear responses requires only subcortical structures and (2) cortical ablation greatly prolongs or prevents extinction of fear responses. These observations have suggested the “indelibility” of subcortical emotional memories. In summary, the coordination of the threat response that underlies the development of PTSD involves sights and sounds being fed into the thalamus and routed to the amygdala, which can also receive direct input from the olfactory system. The medial prefrontal and anterior cingulate cortex and hippocampus then modulate these sensory inputs through the amygdala, which produces a coordinated response to the threat.
The underlying neurobiology of addiction has been the subject of intense study over the past several decades, and many of the structures identified as key components in the development and/or perpetuation of the addictive process overlap with that of PTSD. For example, the amygdalar hyperactivity observed in PTSD is also seen in addiction, particularly as it relates to the chronic activation of brain stress systems and increased corticotropin-releasing factor (CRF) during acute withdrawal from all major drugs of abuse.
18 Also, the neurocircuit involving the medial prefrontal cortex and its connections to nucleus accumbens and ventral pallidum has been identified for its role in animal models of “craving,” and drug-induced reinstatement. These common neurobiological elements suggest the importance of considering single medications for treatment of comorbid SUD and PTSD.
Pharmacotherapy of PTSD and Alcohol SUD
Pharmacotherapy meant to address both PTSD and alcohol use disorders (AUD) allows consideration of agents that have obtained U.S. Food and Drug Administration (FDA) approval for conditions other than PTSD, including antidepressants, anticonvulsants, and antipsychotic medications. Two FDA approved selective serotonin reuptake inhibitor (SSRI) medications for treatment of PTSD are sertraline and paroxetine. In studies using the Clinician Administered PTSD Scale (CAPS) as treatment outcome measure, response rates have been relatively high (53–60%) and superior to placebo responses (32–38%).
19,20–22 An interesting study using sertraline in patients with PTSD and alcohol abuse found reduced alcohol consumption in those patients who had an improvement in their PTSD symptoms after treatment with sertraline.
23 In that study, conducted over a 12-week period, the percentage of days using alcohol was 10% for the PTSD responders and 32% for non-responders. Similarly, the days of heavy alcohol use were 9% for the PTSD responders and 22% for the non-responders.
Open pilot studies have examined a wide range of agents that do not have FDA approval for treatment of PTSD, and typically these agents are prescribed adjunctively with SSRIs. Adjunctive medications include anticonvulsants, antipsychotics, and adrenergic blockers. The anticonvulsants include carbamazepine, topiramate, gabapentin, tiagabine, valproate, and lamotrigine. The antipsychotics include olanzapine, quetiapine, and risperidone, and the adrenergic blockers include prazosin, disulfiram, or the more specific dopamine beta-hydroxylase inhibitor, nepicastat. The anticonvulsant valproate at 500–1500 mg daily was found to be no better than an SSRI alone in the treatment of PTSD.
24,25 The atypical antipsychotic olanzapine at 5–20 mg daily showed reductions in PTSD symptoms in two open trials, but no placebo-controlled studies are available.
26,27 Controlled trials of risperidone at 1–6 mg daily combined with an SSRI have shown reduction in PTSD symptoms compared to the SSRI alone, as well as demonstrating efficacy in reduction of associated psychotic symptoms associated with chronic PTSD.
28,29 Prazosin and nepicastat studies are ongoing, with support for prazosin as a treatment option for reduction of nightmares as well as daytime psychological distress associated with trauma.
30,31Two FDA approved treatments for alcoholism, naltrexone and disulfiram, have been examined in veterans with both PTSD and alcohol dependence. Petrakis and colleagues examined the effect of either one or both of these medications in comparison to placebo in the treatment of alcohol dependence and PTSD.
32 In this sample of 254 veterans, approximately 37% met DSM-IV-TR criteria for a diagnosis of PTSD. Among those diagnosed with PTSD, there were significantly greater days abstinent from alcohol in the medication conditions (ie, disulfiram, naltrexone, and disulfiram/naltrexone) when compared with placebo. Additionally, the medication conditions also demonstrated significant reduction in the percent of heavy drinking days in comparison to the placebo group. In regards to reduction of PTSD symptomatology, those treated with disulfiram demonstrated lower total scores over time and lower hyperarousal scores over time on the Clinician Administered PTSD Scale (CAPS) when compared to those on naltrexone. This reduction was thought to be due to disulfiram’s inhibition of dopamine beta hydroxylase and associated reduction in adrenergic activity.
Poor adherence with naltrexone may contribute to its limited efficacy for alcohol dependence in PTSD patients, and this problem might be addressed using the depot formulation of the medication (Vivitrol) in this population.
33 The best candidates for naltrexone are those with a strong family history of alcoholism (more than half of their first-degree family members are alcohol dependent) and more severe bingeing or dependence. There are no significant contraindications to naltrexone except concurrent opiate agonist treatment, since as an antagonist it would block the analgesic effects of opiates and/or precipitate opiate withdrawal.
In summary, SSRI pharmacotherapy with either sertraline or paroxetine is the standard option for treatment of PTSD, and when these medications effectively reduce PTSD symptoms, alcohol consumption may also be reduced in patients with AUD comorbidity.
23 Among anticonvulsants, only valproate has been examined in controlled trials, and when used adjunctively with SSRIs, it has not been found superior to placebo for reduction of PTSD symptoms or alcohol consumption. In placebo-controlled trials, the combination of an SSRI with risperidone has produced greater reduction in PTSD symptoms when compared to SSRI alone. Whether this combination will be superior to SSRIs alone for veterans with combined PTSD and SUD has not yet been tested. Disulfiram reduces alcohol consumption in PTSD and might be considered as an adjunctive agent with SSRIs, since disulfiram also appears to independently reduce PTSD symptoms. Finally, there is no contraindication to adding the FDA-approved medications for treatment of alcohol dependence, naltrexone or acamprosate, to proven treatments for PTSD when patients have comorbid AUD.
Pharmacotherapy of PTSD and Opioid SUD
Researchers have traditionally made a distinction between those opiate-addicted persons using heroin and those using prescribed opiate medications. Heroin addicts are typically thought to have initiated use of this substance as part of a longer history of polysubstance abuse and may be associated with higher levels of premorbid trauma, psychiatric comorbidity, and correlates of poverty. Prescription opiate abuse, however, can be characterized as either (1) medical use, where the individual takes the medication as prescribed and develops dependence despite adherence, or (2) extra medical use, where an individual obtains and uses opiate medications in an illicit fashion. To further complicate this picture, many often receive treatment with opiate pain medication as part of therapy for injuries that have resulted in PTSD, including mild traumatic brain injury (mTBI). Interestingly, recent data from a study conducted in a veteran population suggested that using higher doses of morphine to treat military related injuries are associated with lower rates of developing subsequent PTSD.
34 Ultimately, in regard to those diagnosed with both PTSD and comorbid opioid dependence, there may be two distinct populations of patients—one representing those heroin-addicted patients who are more likely to encounter traumatic experiences and subsequently develop PTSD and the other representing persons, particularly veterans, who experience some sort of trauma, with or without associated long-term physical injury, resulting in the need for opiate medications. In all cases of opiate dependence, however, addicts can benefit from use of pharmacotherapy, either in the form of methadone or buprenorphine, and experience improvement in their level of functioning and overall quality of life.
For those diagnosed with PTSD and prescribed opiates for chronic non-malignant pain (CNMP), the development of tolerance, need for repeated escalations in opioid dose, and emergence physiological dependence can become problematic. First, opioids can mask PTSD symptoms, being erroneously interpreted as “self-medication,” or obscuring the motivation for use of the medication. Second, PTSD symptoms may be exacerbated during opioid withdrawal, since there are elements shared by the two syndromes, and it could become difficult for patients to distinguish the source of their core anxiety as it is related to PTSD, abstinence from opioids, or the underlying pain syndrome. Lastly, opioids interfere with evidence-based behavioral interventions like prolonged exposure therapy, since patients need to experience PTSD symptoms in order to obtain efficacy from the treatment.
4,35,36 This distinction is critical for appropriate therapeutic intervention.
Addiction represents one final possible physiological complication of CNMP treatment with opioids. Rates of abuse and/or addiction in chronic pain populations are estimated to be approximately 10%, although published reports range from as little as 3% to as much as 23% for current substance use.
37,38 The known risk factors for development of substance abuse in the general population are good predictors for problematic prescription opioid use and include a history of early adolescent substance use, personal or family history of substance abuse and comorbid psychiatric disorders such as PTSD. Aberrant drug-taking behaviors can be predictive for identifying patients whose opioid use should be addressed in order to optimize treatment of comorbid PTSD. These behaviors include selling prescription drugs, prescription forgery, stealing or borrowing another person’s drugs, injecting oral formulations, obtaining prescription drugs from non-medical sources, concurrent abuse of related illicit drugs (ie, heroin, cocaine), multiple unsanctioned dose escalations, and recurrent prescription losses.
39Treatment for comorbid opioid SUD within the context of comprehensive PTSD therapy involves medical withdrawal (detoxification) and/or maintenance therapy using either a full opioid agonist, methadone, or partial agonist, buprenorphine. These treatments are needed to reduce tolerance and hyperalgesia, as these complications of chronic opiate treatment often worsen PTSD symptomatology and undermine its most effective treatments. Innovative approaches for detoxification include lofexidine and buprenorphine. Lofexidine is an effective and acceptable alternative to clonidine, which has side effects many patients find intolerable for medical withdrawal. Although lofexidine has not yet been approved by the FDA for treatment of opiate detoxification, it has been widely used in Europe for over ten years and Phase 3 clinical trials are currently being conducted in the US. Buprenorphine, a partial mu-opioid receptor agonist, provides relief of withdrawal when initiation of the medication occurs in low doses (ie, less than, or equal to 4 mg sublingually). At higher doses, however, it can precipitate withdrawal in opioid dependent patients.
40Importantly, opiate agonist therapy has demonstrated equivalent effectiveness in reduction of substance abuse among those patients with PTSD when compared to those without current psychiatric diagnosis.
41 However, PTSD among opiate-addicted persons in methadone clinics has been found to be associated with poorer treatment adherence and higher rates of co-occurring substance abuse.
42 Further research into specific treatment options meant to reduce PTSD symptomatology within opiate dependent persons is needed, particularly in light of its impact on these compounding factors. Additionally, as efforts are made within the medical field to curtail patient access to prescription opiates, appropriate referral and proper linkage to addiction services (ie, methadone maintenance or office-based buprenorphine) is critical.
Pharmacotherapy of PTSD and Cannabis SUD
The relationship between PTSD and cannabis use disorders (CUD) has been a subject of much study in the literature. In a survey of adults from the United States, PTSD was found to be associated with increased odds of lifetime cannabis use as well as daily cannabis use in the past year.
43 Similar findings were suggested in a study of adolescents and young adults, where PTSD contributed to development of cannabis use disorders, particularly in those persons with high levels of peer deviance or family history of SUD.
44 Increased cannabis use among those with PTSD could also be explained, in part, by self-medication behaviors.
45 For example, cannabis was found to be helpful in reducing PTSD symptoms among Vietnam veterans,
16 and in a separate study, Bonn-Miller et al. found a correlation between the severity of PTSD symptoms and the motivation to use cannabis in order to manage emotional distress.
46 In addition to its impact upon the incidence and risk of development of cannabis use disorders, PTSD also affects addiction-specific aspects of CUD. For example, in one recent study of veterans, in comparison to cannabis users without PTSD, those with PTSD reported significantly increased use of cannabis to cope; cannabis-related problems (ie, negative social, occupational, physical, and personal consequences); severity of cannabis withdrawal during quit attempts; and craving.
47Interestingly, while some studies have found cannabis use to be helpful in the reduction of PTSD symptoms, preclinical trials have found it to be anxiogenic in nature, suggesting its potential for worsening PTSD. In both mice and rat studies utilizing the elevated-plus maze test, delta-9 tetrahydrocannabinol (Δ
9-THC), the major psychoactive ingredient in cannabis, caused anxiolytic effects when administered in lower dosages, but increased anxiety-like behaviors when given in high doses.
48 Human clinical trials have not yet demonstrated a clear, causal link between cannabis use and increased worsening of PTSD; however, Δ
9-THC has been shown to elicit anxiety symptoms through neurotransmitter systems other than that of the endocannabinoid system (ie, serotonin, norpeinephrine, GABA and glutamate).
49Consideration of pharmacotherapeutic options that would be beneficial in treatment of comorbid CUD and PTSD occurs within the context of this complex relationship. Further complicating this matter, there are currently no FDA approved medications for the treatment of CUD. However, several medications have been examined, both directly and indirectly, for their ability to reduce withdrawal symptoms and/or reinforcing effects of cannabis use. While earlier pilot data suggests potential benefit, a more recent double-blind, placebo controlled trial found that buspirone did not significantly reduce cannabis craving or use, though a trend was observed toward reduction in positive urine drug screens and shorter time to first negative UDS.
50 In an earlier open label pilot study of adolescents and young adults with comorbid major depressive disorder (MDD) and SUD, Cornelius et al. reported that fluoxetine was able to decrease symptoms of depression as well as drinking and cannabis use; however, in a later double-blind study, fluoxetine did not significantly reduce number of days of cannabis use or cannabis related symptoms.
51 In addition, medications such as lithium and lofexidine have shown some efficacy in controlled laboratory studies and small open-label clinical studies, but additional study is necessary to determine their potential benefits.
52 Of the aforementioned medications, fluoxetine (as well as other SSRI medications) and buspirone are cornerstone components in the pharmacologic management of PTSD, and thus worth consideration in treatment of comorbid PTSD and CUD, given their potential to decrease cannabis use. Additional study, specifically in this clinical population, is warranted.
The use of cannabinoid agonists (ie, dronabinol) bears mention, since this category of medications will soon be undergoing study for treatment of both disorders. Given the success of agonist therapy in treatment of both opioid and nicotine use disorders, consideration of cannabinoid agonists for treatment of CUD has been a longtime subject of interest. In an early inpatient human laboratory study, oral Δ
9-THC was able to reduce positive subjective effects (ie, “good drug effect” and “high”), but did not significantly decrease subjects’ choice to self-administer smoked marijuana.
53 In a separate clinical trial, Δ
9-THC was shown to reduce withdrawal symptoms when administered orally in low doses.
54 Most recently, in a double-blind, placebo controlled trial, dronabinol was superior to placebo in reducing cannabis withdrawal symptoms and improving treatment retention, though there was no observed benefit in regards to cannabis use reduction or rates of abstinence.
55 The potential of cannabinoid agonist therapy for CUD may represent an important advance in the field and an exciting addition to our pharmacologic armamentarium.
To date, despite anecdotal reports from patients, there have been no controlled trials examining the efficacy of cannabis in the treatment of PTSD. However, that six states currently list PTSD as a qualifying condition to receive medical marijuana evidences the need for additional study. To that end, a study testing the effect of smoked or vaporized marijuana in treatment of PTSD in veterans is currently being considered by the National Institute on Drug Abuse (NIDA), having already been approved by both the FDA and the Department of Health and Human Services.
Innovative PTSD Treatments
As stated earlier, failure to extinguish learned associations between neutral cues and conditioned aversive responses is central to the pathogenesis of PTSD. Likewise, the development of associations between previously neutral cues and substances of abuse contributes to craving and assists in the perpetuation of the addictive process.
56 Thus, innovative pharmacologic approaches focusing on the modulation of extinction processes may have efficacy in the treatment of both PTSD and SUD.
The adrenergic system appears to play opposing roles in extinction and PTSD symptom relief. Prazosin, an alpha 1 adrenergic antagonist, has been found to be effective in reducing PTSD symptoms of hyperarousal and sleep disorders; however, these agents can also block extinction of aberrant learned associations. In contrast, adrenergic agonists, like yohimbine, can facilitate extinction, but worsen PTSD symptoms.
57,58 In regards to substance abuse, alpha-1 receptor antagonism has been extensively examined in both animal and human models in relation to alcohol, cocaine, and heroin dependence, since adrenergic activity is thought to be an important substrate in the neurobiology of both cue- and stress-induced reinstatement of drug use.
56Another promising approach focuses on the gamma amino butyric acid (GABA) and glutamate systems of neurotransmission. GABA agonists can enhance PTSD symptom relief; however, these agents also block extinction learning. GABAergic medications such as pregabalin have also shown some promise in augmentation of antidepressant therapy in treatment of PTSD.
59 However, some GABAergic medications (ie, benzodiazepines) carry the potential for abuse and dependence, so their use must be carefully considered.
60 More research into the effectiveness of GABAergic medications in those with comorbid PTSD and SUD is necessary.
PTSD and SUD pharmacotherapy involving activity at the N-methyl d-aspartate (NMDA) receptor has been a growing focus in research studies. Stimulation of NMDA receptors with partial agonists such as D-cycloserine (DCS) has been examined in the treatment of PTSD and is associated with a reduction in symptoms of anxiety, avoidance, and numbing.
61 DCS has been shown to enhance the effectiveness of exposure therapy for acrophobia (fear of heights) in humans and has also demonstrated an ability to augment the learning process for extinction of conditioned fear responses in both animal and human models.
62,63 Although there is a need for further study, DCS may hold significant promise as a medication to be utilized in conjunction with exposure therapy or cognitive-behavioral therapy for treatment of PTSD.
64Studies of DCS in the treatment of SUD have also yielded promising results. In animal studies, DCS has demonstrated an ability to facilitate extinction of conditioned alcohol-seeking behavior in rats and cocaine-induced conditioned place preference (CPP) in mice.
65,66 In humans, DCS demonstrated an ability to attenuate reactivity to smoking cues in nicotine-dependent individuals, although no effect on smoking behavior was observed.
67 The underlying neurobiology of this treatment approach involves NMDA receptors located in high densities in the hippocampus and the essential role of glutamate in learning and memory through its induction of long-term potentiation (LTP), an important component of synaptic plasticity.
68 Increased attention to LTP as well as the disordered learning and memory characteristic of addictive disorders represents a significant change since newer treatment approaches for both comorbid PTSD and SUD can be considered from within this paradigm.
In summary, innovations in the combined treatment of PTSD and SUD have benefitted from our growing understanding of the underlying neurobiology of these two illnesses. First, recognizing the critical role of hyper-arousal in both the early stages of PTSD symptoms and during withdrawal from substances of abuse allows for consideration of medications targeting the adrenergic system. Second, the overlapping components of the neural circuitry of addictive disorders with those of chronic PTSD creates shared pharmacotherapeutic targets and translates into potential action sites for medications that would ameliorate symptoms of both illnesses (ie GABAergic agents). In particular, while benzodiazepines are relatively contraindicated in patients with PTSD and SUD, a large study among veterans with PTSD and SUD showed that those who got benzodiazepines typically in combination with serotonin reuptake inhibitors had less hospitalizations, fewer emergency room visits and overall better outcomes than those who were not given benzodiazepines.
69 Finally, facilitating extinction learning processes benefits both PTSD and SUD therapy. Thus, continued examination of the glutamatergic system may have far-reaching consequences in our treatment of the aberrant patterns of learning experienced in PTSD and the drug cues associated with relapse in SUD.