Collaborative Care for Anxiety Disorders in Primary Care: a Systematic Review and Meta-Analysis
Abstract
Background:
Methods:
Results:
Conclusions:
Background
Rationale
Objectives
Methods
Eligibility Criteria
Design and population.
Intervention and comparison intervention.
Outcomes.
Search Strategy and Selection Criteria
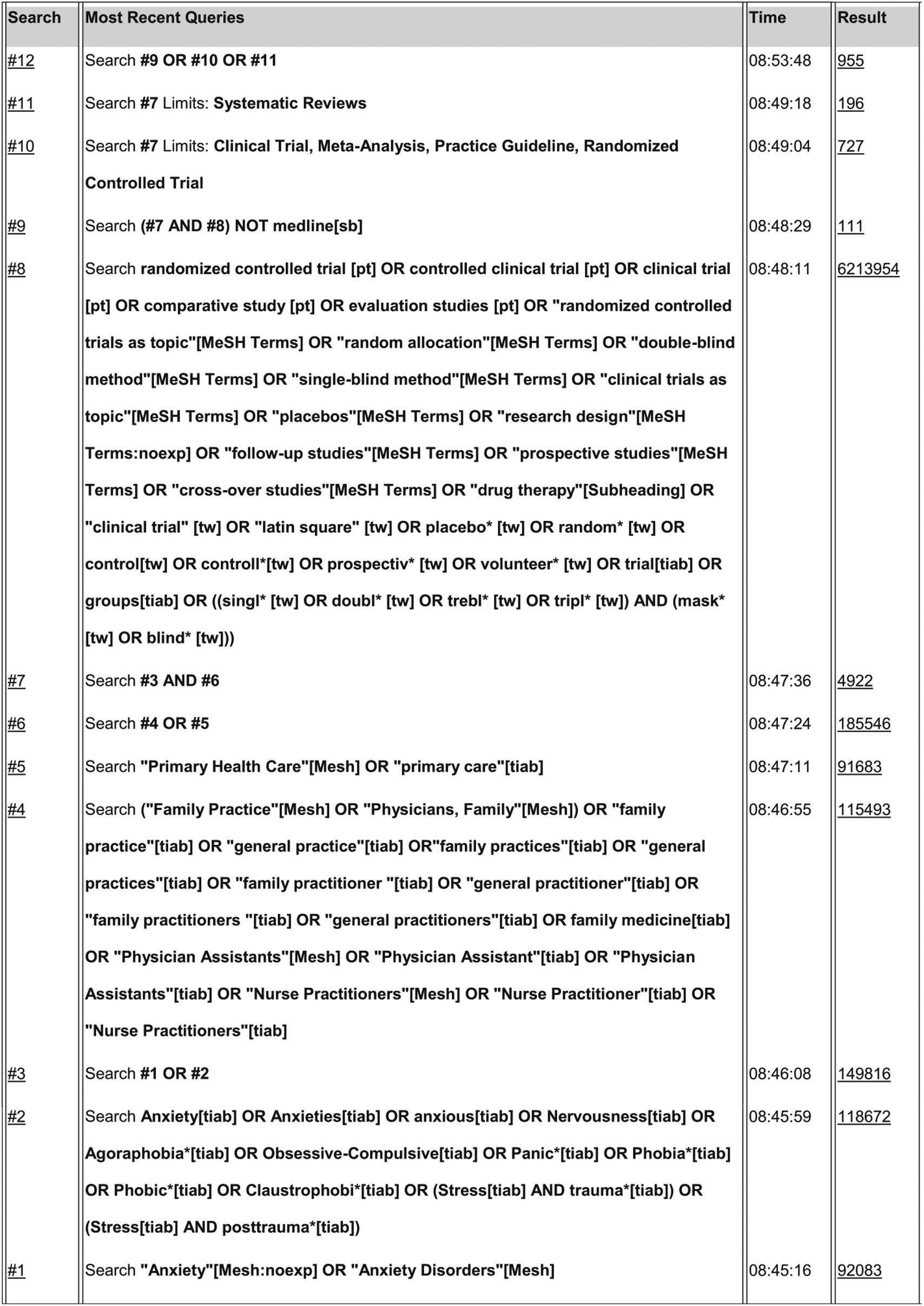
Study Selection
| Study No. | Authors/year | De-sign | Recruit-ment | Diagn instr. | Int. | Setting | N (ITT) | Collaborative care intervention | Professionals involved | Comparison intervention | Outcomes FU | Outcome CC vs CAU | Outcome at 12 months [95 % CI] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Roy-Byrne et al. 2001 (Study 1) | RCT | Referral Screening (waiting room, PHQ-2 PD) | PD CIDI | CC vs CAU | 3 primary care clinics (US) | CC: 57 CAU: 58 | Medication management by psychiatrist | PCP, psychiatrist | CAU by PCP, i.e. pharmacotherapy or referral to mental health professional | ASI, PDSS 3,6,9,12 months | -Improved anxiety outcome at 3,6 and 12 months -Improved panic outcome at 6 months | -Anxiety/panic (ASI): T = 2.14, p = 0.035 ES 0.45 [0.03-0.87] |
| -Panic (PDSS): statistics continuous outcome not reported | |||||||||||||
| 2 | Roy-Byrne et al. 2005 (Study 2) | RCT | Referral Screening (waiting room, PHQ-2 PD) | PD CIDI | CC vs CAU | University affiliated primary care clinics (US) | CC: 119 CAU: 113 | CBT and/or antidepressant medication | PCP, CM, psychiatrist | CAU by PCP, i.e. pharmacotherapy or referral to mental health professional | ASI 3,6,9,12 months | -Improved anxiety/panic outcome at all time points | -Anxiety/panic (ASI): Dif -6.64 [-10.73 to -2.48] p <0.001; ES 0.48 [0.18-0.78] |
| 3 | Rollman et al. 2005 (Study 3) | RCT | Screening (waiting room, PHQ) | PD/GAD PRIME- MD | CC vs CAU | 4 university affiliated primary care practices (US) | CC: 116 CC: 75 | Guided selfhelp and/or antidepressant medication and/or referral to mental health specialist | PCP, CM, psychiatrist/ Psycho- therapist | CAU by PCP and patients received a diagnosis specific brochure | SIGH-A, PDSS 2,4,8,12 months | -Improved anxiety outcome at 12 months -Improved panic outcomes at 12 months -No sign. improvement in GAD outcomes | -Anxiety (SIGH-A): Dif –3.6 [ –6.4 to –0.8] p = 0.01; ES 0.43 [0.10–0.77] -Panic (PDSS): Diff –3.3 [–5.5 to –1.1] p = 0.004; ES 0.58 [0.19–0.97] -GAD (SIGH-A): Diff–1.1 [–5.0 to 2.7] p = 0.57; ES 0.13 [–0.32 to 0.58] |
| 4 | Konig et al. 2009 (Study 4) | Clus-ter RCT | Screening (PHQ) | PD/GAD/any AD PHQ | CC vs CAU | 46 primary care practices (GER) | CC: 201 CAU: 188 | Counselling (CBT) by the PCP | PCP, psychiatrist/ Psycho- therapist | CAU by PCP, including referral to mental health professional | BAI 6,9 months | -No difference in anxiety outcomes | -Anxiety (BAI): CC: M 18.18 SD 12.17 CAU: M 16.72 SD 10.34, p = 0.35; ES –0.13 [–0.36–0.10] |
| 5 | Roy-Byrne et al. 2010 (Study 5) | RCT | Referral | PD/GAD/SOP/PTSD MINI | CC vs CAU | 17 primary care clinics (US) | CC: 503 CAU: 501 | CBT and/or antidepressant medication | PCP, CM, psychiatrist | CAU by PCP, i.e. medication, counseling or referral to mental health professional | BSI, PDSS, GADSS, SPIN, PCL 6,12,18 months | -Improved anxiety outcome at all time points -Improved panic outcome at 6 and 12 months -Improved GAD outcome at all time points -Improved SOP outcome at 6 and 12 months -No sign. improvement in PTSD outcomes | -Anxiety (BSI): Diff –2.63 [ –3.73 to –1.54] p <0.001; ES 0.33 [0.19-0.47] -Panic (PDSS): Diff –2.71 [ –4.29 to -1.14] p = .003; ES 0.48 [0.20-0.76] -GAD (GADSS): Diff –2.34 [–3.22 to –1.45] p <0.001; ES 0.49 [0.30 to 0.68] -SOP (SPIN): Diff −5.71 [−10.74 to −0.68] p = 0.08; ES 0.43 [0.05 to 0.81] - PTSD (PCL-C): Diff −7.7 [−17.55 to 2.15] p = 0.49; ES 0.45 [−0.12 to 1.02] |
| 6 | Oosterbaan et al. 2013 (Study 6) | Clus-ter RCT | Referral | PD/AGO/GAD/SOP/SP MINI | CC vs CAU | 22 primary care practices (NL) | CC: 28 CAU: 27 | Step 1) CBT based guided self-help with antidepressant medication for moderate disorder Step 2) CBT and medication in specialty care | PCP, CM, psychiatrist, CBT therapist | CAU by PCP, i.e. medication, counseling or referral to mental health professional | CGI-I, CGI-S, HRS-A 4,8,12 months | -Improved anxiety outcomes at 4 months | -Anxiety (HRS-A) CC: M 6.14 SD 5.26 CAU M: 8.11 SD 7.83 p = 0.02 ES 0.29 [−0.29 to 0.87] |
| 7 | Muntingh et al. 2014 (Study 7) | Clus-ter RCT | Referral Screening (PHQ) | PD/GAD MINI | CC vs CAU | 43 primary care practices (NL) | CC: 114 CAU: 66 | Step 1) CBT based guided self-help Step 2) CBT Step 3) antidepressant medication | PCP, CM, psychiatrist, CBT therapist | CAU by PCP, i.e. medication, counseling or referral to mental health professional (including CM randomized to CAU) | BAI | -Improved anxiety outcome at all time points -Improved panic outcome at all time points -No sign. improvement in GAD outcomes | -Anxiety (BAI) Diff −6.84 [ −10.13 to −3.55] p <0.001; ES 0.73 [0.37-1.09] - PD (BAI): Diff −9.29 [−12.99 to −5.59] ES 1.03 [0.60 to 1.46] - GAD (BAI): Diff −1.13 [−7.33 to 5.08] p = 0.72 ES 0.13 [−0.56 – 0.81] |
Data Collection Process
Risk of Bias in Individual Studies
Synthesis of Results
Risk of Bias Across Studies
Additional Analyses
Results
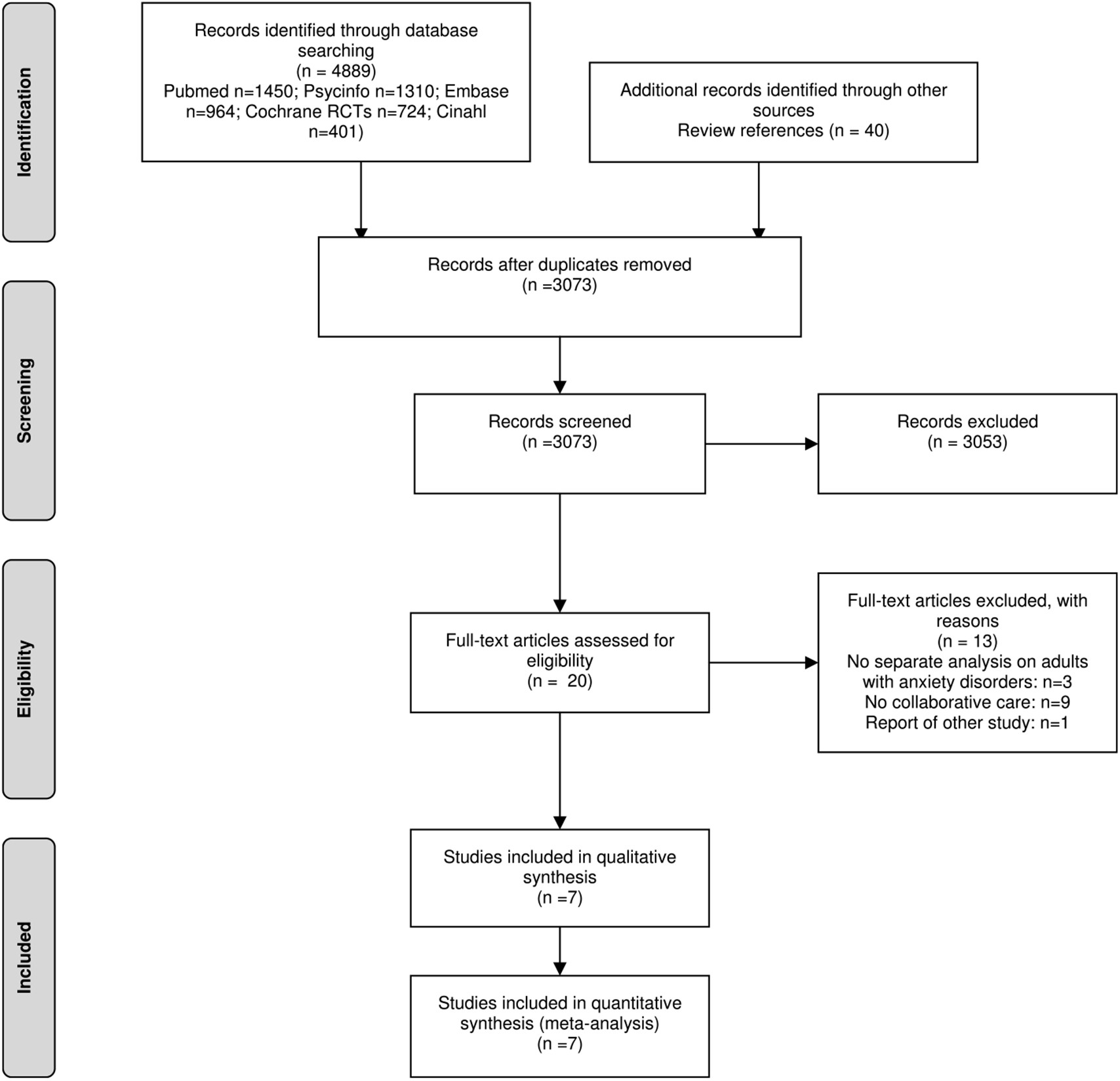
Study Selection
Study Characteristics
Design and participants.
Collaborative care and comparison interventions.
| Study no. | Study (first author, year) | Professionals involved | Professional training | Interventions used | No. contacts with professionals | Collaboration between professionals | Monitoring | Follow-up / relapse prevention |
|---|---|---|---|---|---|---|---|---|
| 1 | Roy-Byrne et al. 2001 | PCP Psychiatrist | PCP: 1-h didactic, medication algorithm | Medication management (paroxetine) and encouragement of adherence and exposure by psychiatrist Educational patient video | 2 visits and 2 phone calls by psychiatrist | The PCP received a typed consultation note after each psychiatric visit. | No information provided | 5 follow-up calls by psychiatrist |
| 2 | Roy-Byrne et al. 2005 | PCP, Psychiatrist CM | PCP: 1-h didactic on, medication algorithm CM: treatment protocol, six videotapes, 1 day long workshop in care management and CBT | Face-to-face CBT Antidepressant medication according to algorithm by PCP Educational video and workbook | 6 sessions by CM | Weekly caseload supervision of CM by psychiatrist 2-way communication of CM and PCP by telephone, fax, and e-mail. | No information provided | Intended were 6 telephone follow-up contacts during 10 months after the active treatment phase by CM |
| Recommendations as needed from a consulting psychiatrist to the PCP via the CM | ||||||||
| 3 | Rollman et al. 2005 | PCP, Psychiatrist CM | PCP: 1-h conference and in dividual meeting of study investigators with PCPs, medication algorithm CM: study protocol and self-management workbooks, attending lectures at the University | CBT based guided self-help Antidepressant medication according to algorithm by PCP Referral to a community mental health specialist | 7 telephone contacts by CM | Weekly caseload supervision of CM by psychiatrist | Monitoring by CM with PDSS/GADSS | Telephone contacts every 1–3 months after the acute phase to monitor symptoms |
| Advice from the psychiatrist to the PCP and patient via CM Communication facilitated through an ambulatory EMR system | ||||||||
| 4 | König et al.2009 | PCP, Psychiatrist/Clinical psychologist | PCP: 10 h training and two additional sessions on counseling skills and CBT | Counseling by PCP, including CBT techniques | No information provided | As needed consultation by psychiatrist/clinical psychologist at PCPs’ practices | No information provided | No information provided |
| 5 | Roy-Byrne et al. 2010 | PCP, Psychiatrist CM | PCP: single-session training, medication algorithm CM: treatment protocol, 6 half days of didactics in care management and CBT | Face-to-face CBT by CM supported by computer program Antidepressant medication according to algorithm by PCP | 6–8 sessions by CM | Weekly caseload supervision of CM by psychiatrist/psychologist Regular” interaction between PCP and CM in person and by telephone | Monitoring with OASIS by CM | Monthly follow-up telephone calls by CM |
| As needed consultation of PCP by psychiatrist Communication facilitated through a webbased monitoring system | ||||||||
| 6 | Oosterbaan et al. 2013 | PCP Psychiatrist/CBT specialist CM | PCP: one educational session, medication algorithm | Stepped care (according to severity): | Step 1: 5 sessions by CM Step 2: No information provided | 2-weekly supervision of CM by CBT specialist | Monitoring with CGI by CM | No information provided |
| CM: treatment protocol, 2-day training session in basic CBT strategies | 1. CBT based guided self-help with support by CM (face-to-face) with antidepressant medication according to algorithm by PCP for patients with a moderate disorder | As needed consultation of PCP by psychiatrist | ||||||
| 2. CBT and antidepressants in specialised mental health service | ||||||||
| 7 | Muntingh et al. 2014 | PCP Psychiatrist/CBT specialist CM | PCP: 3 h workshop, medication algorithm CM: treatment protocol, 3-day workshop in care management and CBT strategies | Stepped care: | Step 1: 5 sessions by CM | Intended was 3-weekly supervision of CM by psychiatrist/CBT specialist GP and CM were “instructed to frequently discuss treatment progress” | Monitoring with BAI by CM | Monthly follow-up telephone calls by CM |
| 1. CBT based guided self-help with support by CM (face-to-face) | Step 2: 6 sessions by CM | As needed consultation of PCP by psychiatrist | ||||||
| 2. CBT by CM | ||||||||
| 3. Antidepressant medication according to algorithm by PCP |
| Content of care* | Pharmaco-therapy (%) | Approriate pharmaco- therapy (%) | Counseling (%) | CBT (%) | Referral to mental health professional(%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study | CC | CAU | CC | CAU | CC | CAU | CC | CAU | CC | CAU |
| Roy-Byrne et al. 2001* | 77 %a | 48 %a | 47 %b | 33 %b | NA | NA | NA | NA | NA | 25 % |
| Roy-Byrne et al. 2005 | 54 %c | 52 %c | 41 %b | 39 %b | 70 % | 34 % | 63 %d | 14 %d | NA | NA |
| Rollman et al. 2005 | 77 %e | 66 %e | NA | NA | 79 %f | NA | 66 %g | NA | 18% | 26 % |
| König et al. 2009 | NA | NA | NA | NA | NA | NA | NA | NA | 33 % | 33 % |
| Roy-Byrne et al. 2010 | 70 %h | 68 %h | 46 %i | 42 %i | 88 % | 51 % | 82 %j | 34%j | NA | NA |
| Oosterbaan et al. 2013* | 45 % | 33 % | NA | NA | NA | NA | 75 %g | NA | NA | NA |
| Muntingh et al. 2014 | 21 %e | 35 %e | NA | NA | 92 % | 12% | 78 %g | NA | 11 % | 21 % |
Outcome measures.
Risk of Bias Within Studies
| Adequate Sequence Generation? | Allocation concealed? | Patients blinded? | Professionals blinded? | Outcome assessors blinded? | Incomplete outcome data addressed? | Free of selective reporting? | Free of other bias | |
|---|---|---|---|---|---|---|---|---|
| Roy-Byrne et al. 2001 | + | ? | ? | ? | + | ? | ? | ? |
| Roy-Byrne et al. 2005 | ? | + | – | – | + | + | ? | + |
| Rollman et al. 2005 | + | + | – | – | + | + | ? | + |
| König et al. 2009 | + | + | – | – | ? | + | ? | + |
| Roy–Byrne et al. 2010 | + | + | ? | – | + | + | + | + |
| Oosterbaan et al. 2013 | + | + | – | – | + | + | + | + |
| Muntingh et al. 2014 | + | + | – | – | + | + | + | + |
Results of Individual Studies
Risk of Bias Across Studies
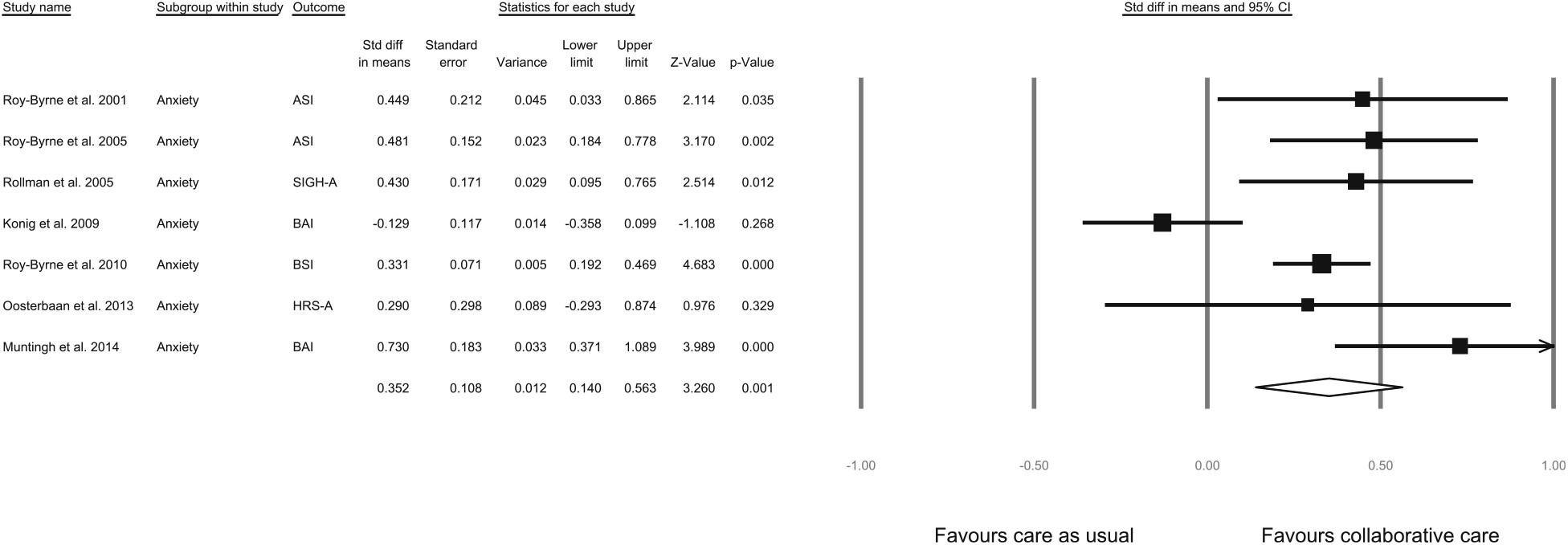
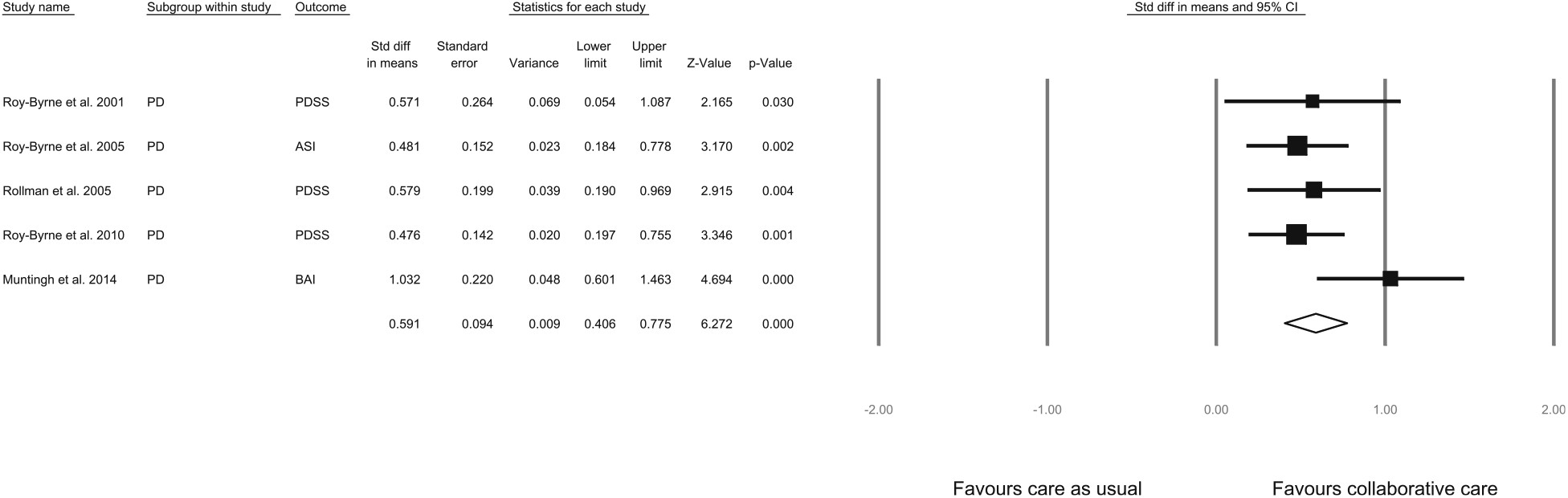
Additional Analysis: Disorder-Specific Impact of Collaborative Care
Additional Analysis: Variables Related to Outcome
| Covariate | Number | SDM | 95% CI | Q | I2 | P |
|---|---|---|---|---|---|---|
| All studies | 7 | 0.35 | 0.14 − 0.56 | 21.73 | 72.39 | |
| Country | 0.031* | |||||
| US | 4 | 0.37 | 0.26 − 0.49 | 1.10 | 0.00 | |
| European | 3 | 0.29 | –0.31 −0.89 | 15.98 | 87.50 | |
| Randomization procedure | 0.031* | |||||
| Patient randomization | 4 | 0.37 | 0.26 − 0.49 | 1.10 | 0.00 | |
| Cluster randomization | 3 | 0.29 | –0.31 −0.89 | 15.98 | 87.50 | |
| Recruitment method | 0.65 | |||||
| Referral by professional | 2 | 0.33 | 0.19 − 0.47 | 0.02 | 0.00 | |
| Systematic identification (or both) | 5 | 0.38 | 0.05 − 0.71 | 21.51 | 81.41 | |
| Care manager | 0.001* | |||||
| Care manager | 5 | 0.42 | 0.29 − 0.55 | 4.66 | 14.24 | |
| No care manager | 2 | 0.13 | –0.43 −0.70 | 5.69 | 82.43 | |
| Intervention content | 0.82 | |||||
| Psychological intervention (CBT) with/without medication management | 5 | 0.42 | 0.29 − 0.55 | 4.66 | 14.24 | |
| Medication management alone | 1 | 0.45 | 0.03 − 0.87 | – | – | |
| Not applicable | 1 | – | − | – | – | |
| Stepped care | 0.041* | |||||
| Stepped care | 2 | 0.57 | 0.06 − 0.53 | 1.58 | 36.85 | |
| No stepped care | 5 | 0.29 | 0.16 − 0.99 | 15.97 | 74.95 | |
| Supervision frequency specialist–care manager | 0.056 | |||||
| Ad hoc | 1 | 0.73 | 0.37 − 1.09 | – | – | |
| Scheduled (i.e. at least 2–weekly) | 4 | 0.36 | 0.25 − 0.48 | 1.03 | 0.00 | |
| Not applicable | 2 | – | − | – | – |
Discussion
Summary of Evidence
Strengths and Limitations
Comparison With the Literature
Implications for Research
Conclusions
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).