Complementary and Alternative Medicine for Posttraumatic Stress Disorder Symptoms: A Systematic Review
Abstract
Objectives:
Design:
Results and Conclusions:
Introduction
Methods
Literature Search Methods
Study Eligibility
Study Design.
Types of Participants.
Interventions.
Outcome Measures.
Data Extraction and Management
Assessment of Methodological Quality
Instruments Used to Assess Risk of Bias and Methodological Quality.
Data Synthesis and Evidence Grading
| Level of Evidence Grade | Criteria |
|---|---|
| A (Strong scientific evidence) | Statistically significant evidence of benefit from >2 properly randomized controlled trials, OR evidence from 1 properly conducted randomized controlled trial AND 1 properly conducted meta-analysis, OR evidence from multiple randomized controlled trials with a clear majority of the properly conducted trials showing statistically significant evidence of benefit AND with supporting evidence in basic science, animal studies, or theory. |
| B (Good scientific evidence) | Statistically significant evidence of benefit from 1 to 2 properly randomized trials, OR evidence of benefit from >1 properly conducted meta-analysis OR evidence of benefit from >1 cohort/case-control/nonrandomized trials AND with supporting evidence in basic science, animal studies, or theory. |
| C (Unclear or conflicting scientific evidence) | Evidence of benefit from >1 small randomized controlled trial(s) without adequate size, power, statistical significance, or quality of design by objective criteria, OR conflicting evidence from multiple RCTs without a clear majority of the properly conducted trials showing evidence of benefit or ineffectiveness, OR evidence of benefit from >1 cohort/case-control/nonrandomized trials AND without supporting evidence in basic science, animal studies, or theory, OR evidence of efficacy only from basic science, animal studies, or theory. |
| D (Fair negative scientific evidence) | Statistically significant negative evidence (ie, lack of evidence of benefit) from cohort/case-control/nonrandomized trials, AND evidence in basic science, animal studies, or theory suggesting a lack of benefit. |
| F (Strong negative scientific evidence) | Statistically significant negative evidence (ie, lack of evidence of benefit) from >1 properly randomized adequately powered trial(s) of high-quality design by objective criteria. |
| Lack of evidence | Unable to evaluate efficacy because of lack of adequate available human data. |
Results
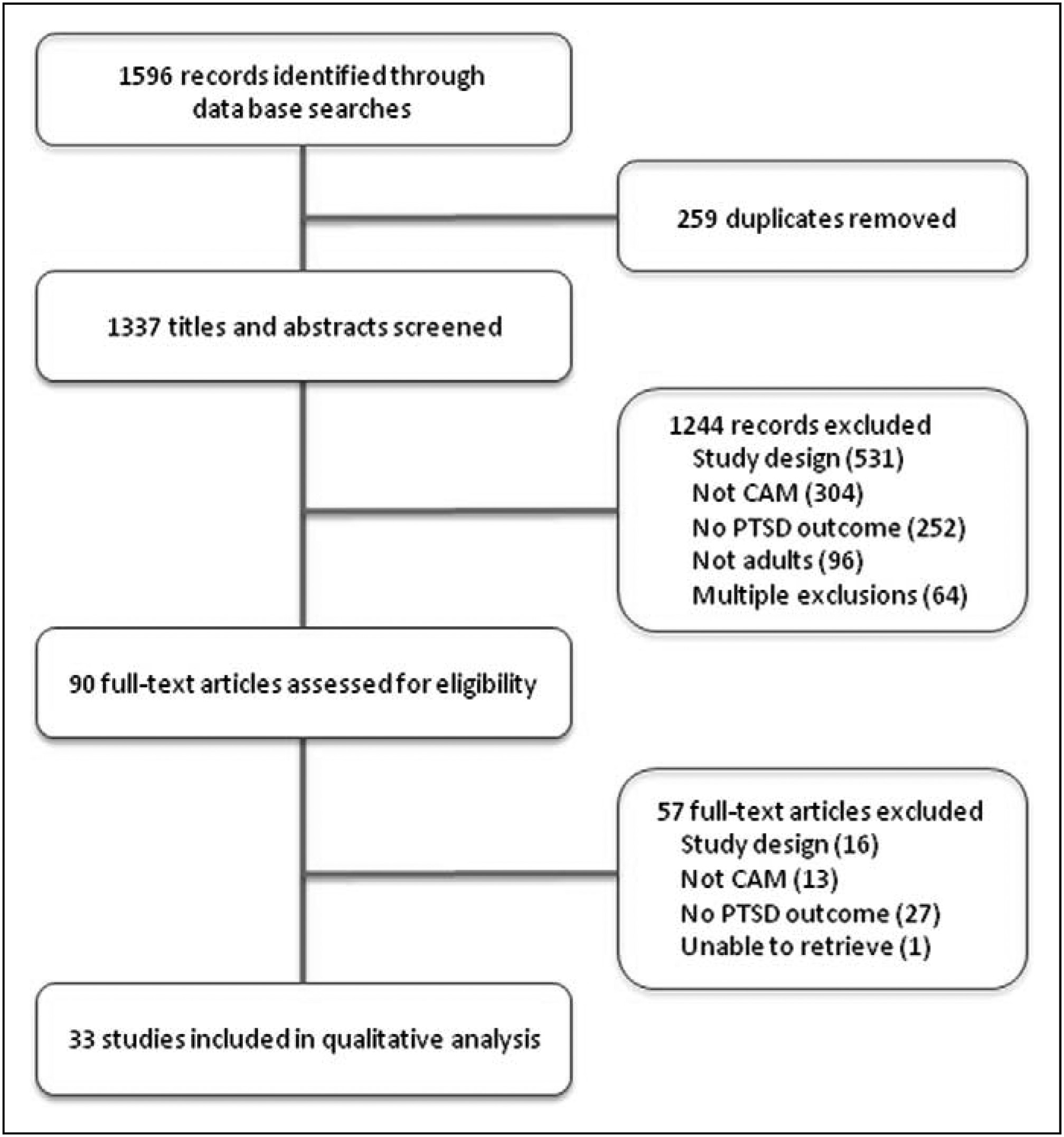
Search Results
| Study/Design | n | % Dropout or Missing Data | Gender Female: Male | Mean Age, Years ± SD (Range) | Intervention Versus Comparator | PTSD Dx Required | Participant Characteristics | Duration of Intervention | PTSD Outcomes | Results | Overall Study Outcome** | Reisch Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Energy Medicine | ||||||||||||
| Boggio, 2010/RCT | 30 | 13 | 21:9 | 44.5 ± 4.4 | rTMS 20 Hz to right or left dIPFC vs Sham rTMS | Yes, SCID criteria | Mixed trauma types | 5 sessions (1600 pulses per session)/wk for 2 wk | PCL, TOPS | Right and left rTMS sig dec PTSD outcomes vs sham (PCL P < .001; TOPS P < .001). | Positivea | 92 |
| Cohen, 2004/RCT | 29 | 17 | 7:17* | 41.7 ± 11.4 (22-68) | rTMS 10 Hz or rTMS 1 Hz to right dIPFC vs Sham rTMS | Yes, SCID criteria | Mixed trauma types | Five 20-min sessions/wk for 2 wk | PCL, TOPS, CAPS-Hebrew version | For PCL and TOPS: 10 Hz rTMS sig better than sham and 1 Hz (P < .002). No diff I Hz rTMS vs sham. | Positivea | 85 |
| Grisaru, 1998/Pre-post | 10 | 0 | 3:7 | 47 (21-53) | rTMS 0.3 Hz | Yes, DSM-IV criteria | Mixed trauma types | Single session of 30 pulses at I-min intervals | IES | No sig change in total IES or IES-1; Sig dec IES-A at 7-day followup (P = .033); no sig diff 28-day follow-up. | Mixedc | 71 |
| Osuch, 2009/Crossover | 9 | 0 | 8:1 | 41.4 + 12.3 (24-56) | Imaginal exposure therapy plus rTMS 1 Hz to right dIPFC v. Imaginal exposure therapy plus sham rTMS | Yes, no criteria specified | Mixed trauma types | Three to five 30-min sessions/wk for a total of 20 sessions | CAPS, IES | No sig diff between exposure + active rTMS vs exposure + sham rTMS except for moderate dec CAPS hyperarousal subscale (P = .08). | Mixeda | 70 |
| Watts, 2012/RCT | 20 | 0 | 2:18 | Tx: 54 ± 12.3; Ctrl: 57.8 ±11.8 | rTMS 1 Hz to right dIPFC vs Sham rTMS | Yes, SCID criteria | Veterans with mostly combat trauma | Five 20-min sessions/wk for 2 wk | CAPS, PCL | rTMS sig reduced CAPS (P = .009) and PCL (P = .0002) vs sham rTMS. | Positivea | 80 |
| Chinese Medicine | ||||||||||||
| Hollifield, 2007/RCT | 84 | 27 | 57:27 | Acu: 42.3 ± 12.1; CBT: 40.9 ± 13.4; Ctrl: 43.4 ± 13.5 | Acupuncture vs (1) CBT; (2) 12-wk waitlist control | Yes, SCID criteria | Mixed trauma types | Acupuncture: two I-h sessions/wk for 12 wk; CBT: one 2-h session/wk for 12 wk | PSS-SR | Both acupuncture and CBT dec PTSD outcomes vs waitlist controls (P < .01). No diff between acup and CBT as both groups improved (P = .29). | Neutrala; Positiveb | 88 |
| Zhang, 2011 RCT | 91 | 1 | 55:36 | 35.0 ± 19.3 (4-89) | Acupoint stimulation (50 Hz) + CBT vs CBT | Yes, WHO criteria | Acute PTSD from China’s 2008 Zhejiang Province earthquake | Acupoint and CBT: 30-min session every other day over 1 wk | IES-R Chinese version | Acupoint + CBT more effective reducing IES-R than CBT alone (P < .01). | Positivea | 77 |
| Mind-body: Biofeedback | ||||||||||||
| Lande, 2010/CT | 49 | 20 | 6:33* | Mean/range not reported | HRV Biofeedback vs TAU | No | Active duty combat soldiers with self-report PTSD | Two 20-min sessions/wk for 3 wk | PCL-M | Both biofeedback and control groups experienced sig dec in PTSD symptoms overtime, no sig diff between groups. | Negativeb | 62 |
| Muller, 2009/Pre-post | 13 | 15 | 8:3* | 35.7 ± 6.1 | Pain-focused cognitive behavioral biofeedback | Yes, MINI criteria | Refugees with PTSD, chronic pain, and experience of torture or war | One 90-min session/wk for 10 wk | Posttraumatic Diagnostic Scale | No sig changes in PTSD symptoms over time. | Negativec | 76 |
| Tan, 2011/RCT | 20 | 5 | 0:20 | 36.0 ± 13.1 (24-62) | HRV Biofeedback vs TAU | Yes, no criteria specified | Veterans with combat-related PTSD | One 30-min session/wk for 8 wk | CAPS, PCL | Biofeedback sig dec CAPS (P < .001) and PCL (P = .035) pre-post; Only CAPS-AN better in biofeedback group vs TAU; no other between-group diff but moderate effect sizes for change in overall sx (Cohen’s d = 0.52 and 0.70 for CAPS and PCL, respectively). | Mixedb | 80 |
| Zucker, 2009/RCT | 50 | 24 | 17:21* | (18-60) | RSA Biofeedback vs progressive muscle relaxation recording | No | Substance use disorder and elevated PTSD sx; mixed trauma types | Personal instruction for portable biofeedback device or PMR recording: 20 min/day for 4 wk | PCL, PTS-T | Both groups decreased PTSD scores over time (both groups P < .01). Biofeedback did not improve PCL scores (P = .32) or PTS-T scores (P = 0.73) over control. | Neutrala | 81 |
| Mind-body: Thought field therapies | ||||||||||||
| Folkes, 2002/Pre-post | 61 | 49 | Not reported | 27.7 (5-48) | TFT | No | Adult and child refugees from 5 language groups | One 60- to 90-min session | PCL (adult or child version) | 50% dropout rate, analysis completed on 31 individuals with complete data sets. PCL-C scores dropped 40% from pre- to postintervention (P = .05). | Positivec | 62 |
| Karatzias, 201 l/RCT | 46 | 43 | 26:20 | EFT: 39.7 ± 10.9; EMDR: 41.5 ± 10.8 | EFT vs EMDR | Yes, DSM-IV criteria | Mixed trauma types | Up to eight I-h sessions. EMDR group received 3.7 + 2.3 h, EFT group received 3.8 ± 2.6 h. | CAPS, PCL | 43.5% dropped out from the EMDR group, and 39.1% dropped out from the EFT group. Both EFT and EMDR improved all outcomes (P < .001). Effect size Cohen’s d = 0.80 for both modalities. | Neutrala | 85 |
| Mind-body: Hypnosis | ||||||||||||
| Abramowitz, 2008/RCT | 32 | 0 | 0:32 | 31.7 (21-40) | Hypnosis vs Zolpidem 10 mg | Yes, DSM-IV criteria | Chronic combat-related PTSD with insomnia | Hypnosis: Two 1.5-h sessions/wkfor 2 wk; Zolpidem: 10 mg nightly for 2 wk | IES-R, PDS | Hypnosis group had sig reductions in PDS (P < .034) and IES scores (P < .0005) compared with Zolpidem over the course of the study. | Positivea | 77 |
| Abramowitz, 2010/Pre-post | 37 | 3 | 0:37 | 41.2 ± 12.2 (24-64) | Hypnosis paired with olfactory-based exposure | Yes, semistructured interview with DSM-IV criteria | Combat trauma | One 90-min session/wk for 6 wk | IES-R | Hypnosis technique decreased stress reaction after 6 wk (P < .0001). | Positivec | 81 |
| Bryant, 2006/RCT | 87 | 46 | 53:34 | (17-60) | Hypnosis + CBT vs (1) CBT; (2) Supportive counseling | No | Acute stress disorder from motor vehicle accident or sexual assault | CBT and CBT plus hypnosis: Both groups five 90-min sessions | CAPS, IES | No diff in IES scores among groups. CAPS scores for CBT and CBT hypnosis groups were 43% lower than counseling group at 3-year follow-up (P = .05). | Neutrala | 77 |
| Mind-body: Meditation | ||||||||||||
| Bormann, 2005/Pre-post | 101 | 39 | 6:56* | 61.8 ± 13.2 (33-84) | Mantram meditation | No | Veterans with combat-related trauma | One 90-min instructional session/wk for 5 wk plus home practice | PCL | PTSD scores (only available for n = 30) decreased 13.7% from pre- to postintervention (P = .02). | Positivec | 90 |
| Bormann, 2008/RCT | 33 | 14 | 0:33 | 56 ± 6.6 (40-76) | Mantram meditation vs Waitlist control | Yes, no criteria specified | Veterans with combat-related PTSD | One 90-min session/wk for 6 wk | PCL, CAPS | Intervention improved CAPS score (effect size −0.33) and PCL score (effect size −0.72), no P values provided. | Positiveb | 85 |
| Brooks, 1985/CT | 25 | 28 | 0:18* | 33.3 | Transcendental meditation vs psychotherapy | No | Vietnam veterans with chronic PTSD | Meditation: One 60-min session/wk for 12 wk; Therapy: One 60-min session/wk for 12 wk | Nonstandard PTSD Scale (no reference provided in article) | Meditation showed positive effect compared with psychotherapy for PTSD and related subscales of emotional numbness, anxiety, depression, alcohol use, insomnia, and family problems (all P < .05). | Positivea | 54 |
| Harris, 2011/RCT | 54 | 6 | 6:48 | 45.5 ± 13.5 | Spiritual prayer and/or meditation vs waitlist control | No | Veterans with trauma exposure, mixed trauma types | One 2-h session/wk for 8 wk | PCL | Spiritual prayer/mediation group dec PCL vs waitlist control (P < .02) | Positiveb | 73 |
| Kearney, 2012/Pre-post | 92 | 20 | 22:70 | 51.0 ± 10.6 | Mindfulness-Based Stress Reduction | No | Veterans, 74% screened positive for PTSD at baseline | One 2.5-h session/wk for 8 wk | PCL | MBSR decreased PCL total and all subscores (P < .001). | Positivec | 86 |
| Kimbrough, 2010/Prepost | 27 | 22 | 24:3 | 45 (23-68) | Mindfulness-Based Stress Reduction | No | Adults with history of childhood sexual abuse | One 3-h session/wk for 8 wk, followed by 3 refresher courses | PCL | MBSR decreased PCL total and all subscores at 8 and 24 wk postenrollment (P < .0001). | Positivec | 95 |
| Price, 2005/RCT | 25 | 4 | 25:0 | 41 (median) (26-56) | Mindful Awareness in Body-Oriented Therapy vs massage | No | Adult women currently in therapy for childhood sexual abuse | Two 60-min sessions/wk for 4 wk | Crime-related PTSD Scale | Both body-oriented therapy and regular massage improved PTSD symptoms, no sig diff between the groups (P > .05). | Neutrala | 81 |
| Price, 2006/RCT | 8 | 0 | 8:0 | (28-52) | Mindful Awareness in Body-Oriented Therapy vs waitlist control | No | Adult women currently in therapy for childhood sexual abuse | One 60-min session/wk for 8 wk | Crime-related PTSD Scale | Body-oriented therapy group had sig pre-post improvement in PTSD scale (P < .01), control group did not experience sig improvements. | Positiveb | 72 |
| Rosenthal, 2011/Pre-post | 6 | 17 | 0:6 | (25-40) | Transcendental meditation | PTSD as judged by investigator | OEF/OIF vets with combat-related PTSD | 3 to 5 h of instruction followed by home practice: 20 min twice a day for 12 wk | CAPS, PCL-M | Participants showed sig improved CAPS (P = .02) and PCL-M (P = .02) scores | Positivec | 86 |
| Mind-body: Relaxation | ||||||||||||
| Colosetti, 2000 Cross-over | 5 | 0% | 5:0 | 38.8 (25-50) | Relaxation (control condition) vs EMDR | Yes, CAPS criteria | Incarcerated women with history of abuse in an intimate relationship | One session relaxation training/wk for 3 to 6 wks followed by one session of EMDR/wk for 3 wks | IES | Neither relaxation training or EMDR exhibited sig changes in PTSD outcomes, no statistics provided due to small sample size. | Negativea | 65 |
| Echeburua, 1997/CT | 20 | 0 | 20:0 | 20 ± 7.1 | PMR (control condition) vs gradual self-exposure with cognitive restructuring | Yes, ADIS-R DSM-III criteria | Women with history of sexual abuse | 1 x/wk for 6 wk; home practice 2x/day | Scale of Severity of Posttraumatic Stress Disorder Symptoms | Cognitive restructuring lead to the reversal of DSM-III PTSD diagnosis in 100% of participants while relaxation was only 40% by 12 months. PTSD scale score was 4x lower in the cognitive restructuring group. | Negativea | 60 |
| Mitani, 2006/Pre-post | 22 | 0 | 0:22 | 42.2 ± 9.7 | Relaxation | No | Japanese fire fighters in a select fire station | One 60-min instructional session followed by home practice: 2-3x/wk for 2 mo | IES-R (Japanese version) | Total IES-R scores dec 60% from pre- to post in PTSD stress-related group (P = .04). Intrusion subscale dec sig in the PTSD stress-related group (P = .038); hyperarousal and avoidance did not change sig. No sig changes in the non-PTSD stress-related group IES scores noted (P = .76-1.0). | Mixedc | 68 |
| Taylor, 2003/RCT | 60 | 25 | 45:15 | 37 ± 10 | Relaxation (control condition) vs (1) exposure therapy; (2) EMDR | Yes, DSM-IV criteria | Mixed trauma types | Eight 90-min individualized session of relaxation, exposure, or EMDR therapy | CAPS, PTSD Symptom Severity Scale, PTSD dx | Exposure superiorto relaxation in reducing number who met PTSD dx (P < .02); no sig diff between EMDR and exposure or EMDR and relaxation for this outcome. CAPS and Symptom Severity Scale dec sig in all groups with no difference between groups. | Neutrala | 85 |
| Mind-body: Guided imagery | ||||||||||||
| Jain, 2012/RCT | 123 | 17 | 11:112 | Tx: 27.1 (20-42); Ctrl: 27.9 (20-48) | Healing touch plus guided imagery vs TAU | No | Returning combat-exposed active duty military with sig PTSD sx | Two 60-min sessions/wk for 3 wk | PCL-M | Healing touch/guided imagery group had sig dec in PCL score compared with controls (P < .0005). | Positiveb | 92 |
| Mind-body: Yogic breath work | ||||||||||||
| Descilo, 2010/CT | 183 | 3 | 160:23 | Tx 1: 30.8; Tx 2: 35.1; Ctrl: 34.7 | Yogic breath work-vs (1) Yoga breath work with exposure therapy; (2) 6-wk waitlist control | No | 2004 Southeast Asian tsunami survivors living in refugee camps who scored > 50 on the PCL | Breath work: one 2-h session/day x 4 days. Exposure therapy: as above + 3-5 exposure sessions | PCL | Both treatment groups showed improvement in PCL scores over waitlist control (P < .0001), no diff between active treatments. | Neutrala; Positiveb | 83 |
| Nutraceutical | ||||||||||||
| Kaplan, 1996/Crossover | 17 | 24 | 5:8* | 39.7 (25-56) | Inositol powder 12 g/d vs placebo (glucose powder) 12 g/d | Yes, DSM-III-R criteria | Trauma type not reported | Inositol or placebo daily for 4 wk, 2 wk washout between crossover | lES-Hebrew version | No sig diff between inositol and placebo for total IES scores or avoidance and intrusion subscales, no P values reported. | Negativeb | 73 |
| Shams, 2007/RCT | 40 | 0 | 34:6 | Tx: 38.2 ± 11.2; Ctrl: 38.5 ± 13.7 | Gingko biloba 200 mg vs placebo | Yes, DSM-IV | Earthquake survivors | 12 wk | Watson’s PTSD Scale | Sig improvement in gingko group over control (P < .01). | Positivea | 73 |
Description of Included Studies
Methodological Quality of Included Studies
| Study | Intervention | Random Sequence Generation | Allocation Concealment | Blinding of Participants/Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Fidelity of Intervention Assessed |
|---|---|---|---|---|---|---|---|---|
| Energy modalities | ||||||||
| Boggio, 2010 | rTMS | + | ? | + | + | + | + | N/A |
| Cohen, 2004 | rTMS | ? | ? | + | + | ? | + | N/A |
| Watts, 2012 | rTMS | ? | ? | + | + | + | + | N/A |
| Chinese medicine | ||||||||
| Hollifield, 2007 | Acupuncture | + | + | – | + | + | + | + |
| Zhang, 2011 | Acupoint stimulation | ? | ? | – | – | + | + | – |
| Nutraceutical | ||||||||
| Shams, 2007 | Ginkgo biloba | ? | ? | + | ? | + | + | ? |
| Mind-body modalities | ||||||||
| Tan, 2011 | Biofeedback | ? | ? | – | ? | + | + | + |
| Zucker, 2009 | Biofeedback | + | ? | – | ? | + | + | ? |
| Karatzias, 2011 | EFT | + | ? | – | + | + | + | ? |
| Abramowitz, 2008 | Hypnosis | ? | ? | – | ? | + | + | ? |
| Bryant, 2006 | Hypnosis | + | – | – | + | – | + | + |
| Bormann, 2008 | Meditation | + | ? | – | + | + | + | + |
| Harris, 2011 | Meditation | + | ? | – | ? | + | + | + |
| Price, 2005 | Meditation | ? | ? | – | ? | + | + | + |
| Price, 2006 | Meditation | ? | ? | – | ? | + | + | + |
| Taylor, 2003 | Relaxation | ? | ? | + | + | – | + | + |
| Jain, 2012 | Guided imagery | + | + | – | + | ? | + | ? |
Quality of the Body of Evidence for Each Modality
Repetitive Transcranial Magnetic Stimulation.
Acupuncture.
Biofeedback.
Emotional Freedom Technique/Thought Field Therapy.
Hypnotherapy.
Meditation.
Relaxation.
Visualization.
Yoga Breath Work.
Natural Products.
Discussion
Implications for Research
Overall Completeness and Applicability of Evidence
Implications for Clinical Practice
Agreement and Disagreements With Other Studies or Reviews
Limitations
Conclusions
Included Studies
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).