“I have an opportunity to become the psychiatrist on a systematic case review (SCR) team for a local primary care clinic. What would my role be, and how would it affect my patients and my practice?”
The systematic case review (SCR) is a key component of the collaborative care model (
1), which is a cost-effective approach (
2–
4) to caring for patients with depression (
1) and anxiety disorders (
5). It can be modified into TEAMcare for patients with comorbid psychiatric and medical illnesses (
6,
7). Dr. Katon called the SCR the “secret sauce” of collaborative care. As a member of an SCR team, you will work closely with a care coordinator and an SCR primary care provider (when caring for patients with comorbid medical and psychiatric problems). Some SCR teams also include a social worker and a pharmacist. The team usually meets together either in person or virtually for two hours a week and uses their electronic registry to review the progress of patients enrolled in the program and make recommendations to their primary care providers to help patients achieve their goals and improve clinical outcomes. The COMPASS (Care of Mental, Physical and Substance-Use Syndromes) initiative found that having fewer SCRs was associated with lower depression response and remission rates (
8). The SCR team is able to provide a holistic approach and avoid overwhelming patients with multiple simultaneous interventions. This is especially valuable for the subset of primary care patients whose psychiatric, medical, and social problems require more help than any one health professional can individually provide.
Imagine the first patient you see today is a 60-year-old man who lost his ability to cope when his back gave out in 2005. He presents with symptoms of depression and a score of 20 on the nine-item Patient Health Questionnaire (PHQ-9). He lost his job and cannot afford either his medication or his housing costs. In addition, his type 2 diabetes is out of control, as evidenced by his glycated hemoglobin (HgA1c) level of 10.7; his hypertension is poorly controlled; and he has a history of myocardial infarction and a stent.
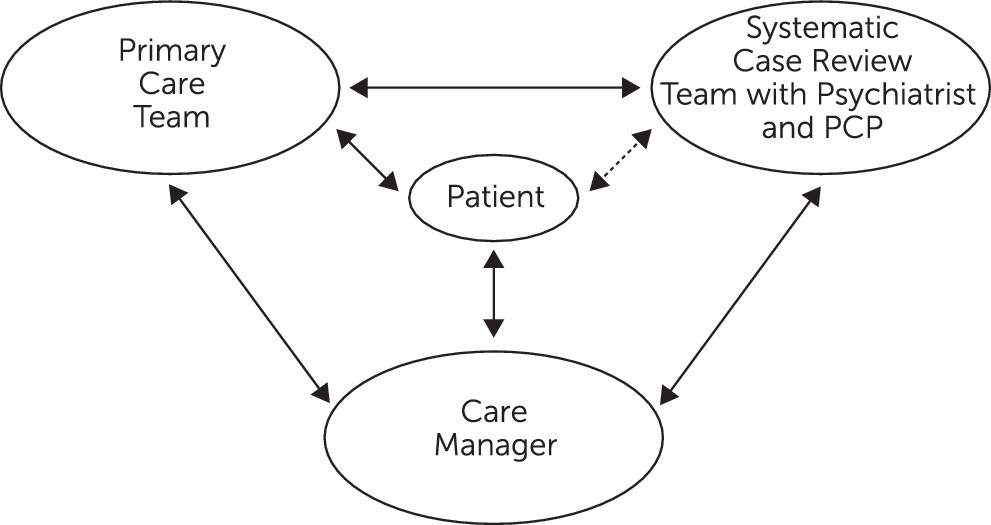
The first challenge for the team is to decide where to start. The patient is actively discussing his situation with his care coordinator, who uses motivational interviewing and suggestions for self-management techniques to engage him in improving his health. The diagram, next page, shows how the patient, care coordinator, SCR psychiatrist, SCR primary care provider, and primary care team interact with each other (see
Figure 1).
The SCR team usually has a checklist to systematically determine whom to review each week. For example, the team may prioritize all new patients, ensuring they are reviewed within a week of care coordinator intake; patients not improving per their individualized care plans; severe and challenging patients; patients recently hospitalized or seen at the emergency room; and patients whom the care coordinator is unable to engage in treatment. The registry is a critical tool that helps the SCR team longitudinally track each patient’s individualized treat-to-target goals and increase the intensity of care as needed.
Participating in the SCR team allows you and the team to provide timely input for a much larger population of patients than you could possibly interact with if you were seeing them on a one-to-one basis. Having support from care coordinators for monitoring patients between visits, motivational interviewing, behavioral activation, and making referrals can help make providers much more efficient. Some psychiatrists initially have medicolegal concerns about making recommendations for patients they have not seen directly. This has been addressed by the American Psychiatric Association (APA), which actively supports psychiatric participation in the collaborative care model. The key is that the psychiatrist on the SCR team makes recommendations but does not write prescriptions or orders unless he or she directly sees the patient. The responsibility for the patients remains with the primary care team. Many SCR psychiatrists also have some time to see patients in person when there is a need to resolve outstanding diagnostic or treatment issues. It is important for the psychiatrist to be reachable throughout the week to support the care coordinators if any patients are in crisis.
Checking back six months after your 60-year-old gentleman was enrolled, the SCR team determines that his financial and housing issues need to be addressed immediately with help from the social worker. Next, they suggest an antidepressant to help alleviate his depression and decrease his pain without exacerbating his diabetes. The care coordinator works with him to identify what he cares about most. The patient is most motivated by the prospect of being able to visit his grandkids. The SCR team discovers that his depression and unstable diabetes are major barriers to his goal of seeing his grandkids, and the members of the team suggest ways to tackle these problems. As the patient becomes less depressed, he becomes more motivated to monitor his glucose and begin a walking program. He does not really care about his HgA1c level but is very happy to spend time with his grandkids again. His HgA1c level, blood pressure, and PHQ-9 score substantially improve.
A major barrier to dissemination of the collaborative care model has been lack of financial reimbursement for SCR team members. Fortunately, since January 2017, this has changed, with the Centers for Medicare and Medicaid Services initiating monthly per-patient bundled reimbursement for teams delivering the collaborative care model, including SCR to patients with Medicare.
Most psychiatrists find that being on an SCR team is very rewarding and provides a change of pace from their other clinical responsibilities. The role involves, among other responsibilities, teaching care coordinators about mental health problems; the coordinators then become more effective over time in managing such problems. Psychiatrists also learn from both care coordinators and primary care providers about medical and system issues. It can be very rewarding to see patients who often would have failed to follow up with their care providers in person do very well with the support of the care coordinator and the extended team.