The Social Determinants of Mental Health: Psychiatrists’ Roles in Addressing Discrimination and Food Insecurity
Abstract
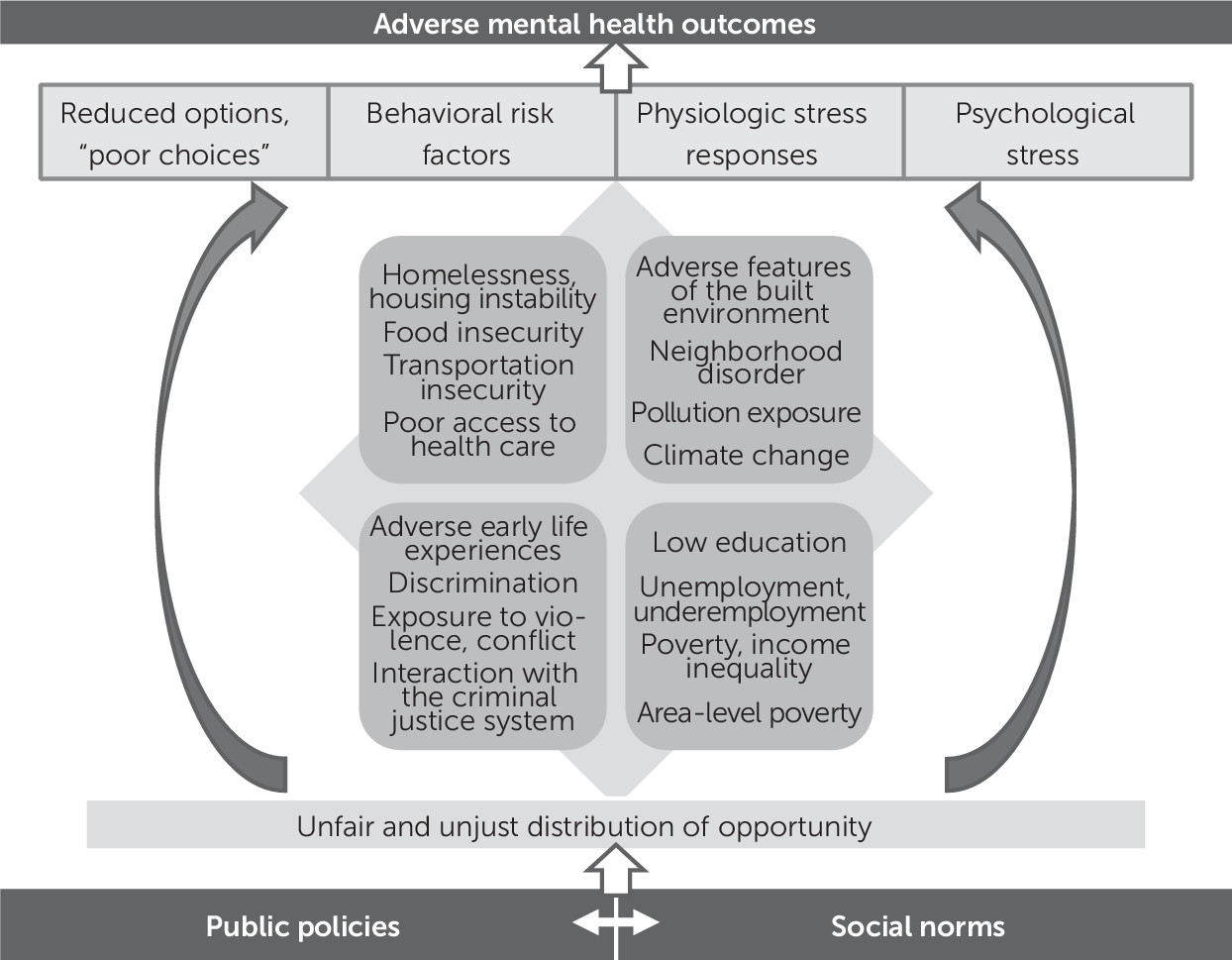
Conceptualizing the Social Determinants of Mental Health
Two Examples of the Social Determinants of Mental Health
| Type of discrimination | Definition | Example |
|---|---|---|
| Interpersonal (individual) | Face-to-face or covert acts of discrimination toward a person | Physician’s implicit bias that leads to poorer treatment of a patient |
| Institutional (organizational) | Policies and practices within and across institutions that disadvantage certain groups | Denial of mortgage applications to black and Latinx populations compared with white populations with similar credit histories |
| Structural (systemic) | A system in which public policies, institutional practices, cultural representations, and other norms work in various, often reinforcing, ways to perpetuate group inequities | Mass incarceration and its disproportionate effects on people of color |
| Legal (de jure) | Discrimination that is mandated by law | Jim Crow laws; racial housing covenants |
| Illegal (de facto) | Discrimination that is without legal basis but sanctioned by custom or practice | Underrepresentation of women and minorities in leadership roles in medicine |
| Overt | Blatant forms of discrimination | Racist or sexist epithets |
| Covert | Subtle forms of discrimination | Microaggressions |
BOX 1. Two-item screening for food insecurity and examples of questions that clinicians can ask to follow up on a positive screening
Psychiatrists’ and Mental Health Professionals’ Roles
Conclusions
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing PsychiatryOnline@psych.org or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).