Geriatric psychiatrists can make a significant contribution to the quality of end-of-life care provided to older adults with mental disorders in the context of serious illness. Expertise in psychiatric, psychological, social, and spiritual symptom management is a natural fit with palliative and hospice care. Learning and applying knowledge and skills in palliative and hospice care allows geriatric psychiatrists to make valuable additions to the provision of high-quality end-of-life care by optimizing the quality of life of geriatric psychiatric patients and their families. Although this article is directed toward geriatric psychiatrists because of their frequent interaction with patients at the end of life, the concepts discussed are relevant to all psychiatrists caring for patients at any age who may be facing life-limiting illnesses. We provide an overview of palliative and hospice care, use a case study to illustrate components of palliative and hospice care relevant to geriatric psychiatry practice, and comment on considerations pertinent to the coronavirus disease 2019 (COVID-19) pandemic.
The Aging Demographic
Worldwide, people are living longer, and the population is aging (
1). The National Center for Health Statistics has estimated the current life expectancy of those older than age 65 to be 18.1 years for men and 20.7 years for women (
2). For people age 65 and older, the 10 leading causes of death are heart disease, cancer, chronic lower respiratory disease, cerebrovascular disease, Alzheimer’s disease, diabetes, injuries, influenza and pneumonia, kidney disease, and septicemia (
3). Many of these conditions require thoughtful end-of-life care, and people with these conditions could potentially benefit from palliative care. Of particular interest to the geriatric psychiatrist is end-of-life care for people with dementia.
Between 2006 and 2016, the death rate from Alzheimer’s disease increased 21.0% (
4). It is estimated that by 2025, 7.1 million Americans will be living with Alzheimer’s, and that number will climb to 13.8 million by 2050 (
5). As the US population rapidly ages and the number of people living with dementia or other life-limiting illnesses continues to rise, so too will the population’s need for end-of-life care, with a greater need for intervention from geriatric psychiatrists and palliative care specialists.
Functional Decline
Many of the leading causes of death, including Alzheimer’s disease, are chronic illnesses that lead to a gradual functional decline, whereas others are more abrupt. Patterns of functional decline are important to consider in end-of-life care.
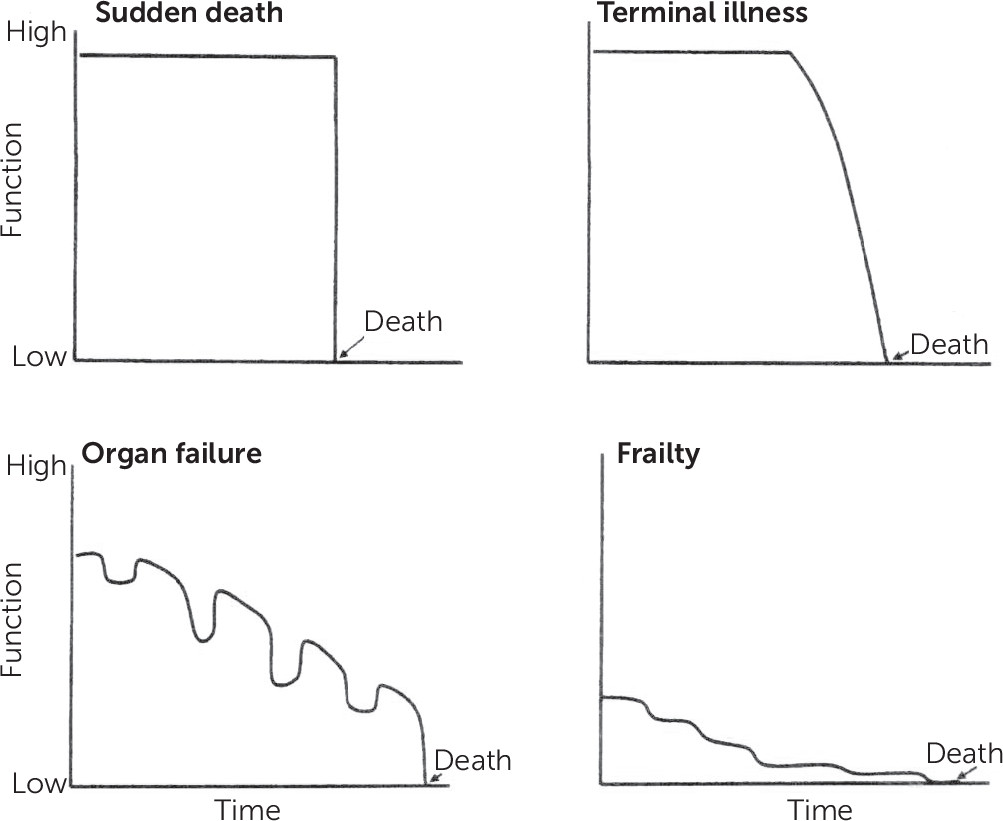
In 2002, Lunney et al. published a large study that evaluated patterns of functional decline during the last year of life, and they proposed four trajectories of decline: sudden death, terminal illness, organ failure, and frailty (
Figure 1) (
6). In sudden death, people are largely independent with minimal functional decline before death. In terminal illnesses, such as cancer, people have a steady functional decline with a short terminal phase. Those with organ failure (such as congestive heart failure or chronic lower respiratory disease) tend to experience a slow decline with periods of crisis and eventually sudden death. For conditions of frailty (such as dementia), people have progressive, significant debility in the last year of life. Understanding these patterns is useful in guiding discussions and decisions about end-of-life care.
Taking a closer look at the trajectory of decline in dementia, people age 65 years or older are expected to live only 4–8 years after receiving a diagnosis of Alzheimer’s (
5). To compare this trajectory with that of other types of dementia, one Swedish study used a database to evaluate mortality after diagnosis for more than 15,000 patients with dementia by calculating hazard ratios for each subtype of dementia compared with Alzheimer’s disease. Results showed the lowest mortality risk for people with Alzheimer’s disease, the highest adjusted mortality risk for those with frontotemporal dementia, and the highest crude mortality rate for those with vascular dementia. In addition, regardless of dementia type, risk factors for increased mortality included male gender, increased age, lower Mini-Mental State Examination score, and higher number of medications at the time of diagnosis (
7).
People with dementia experience the most debility in their last year of life. Functional decline in mobility, inability to swallow, and nutritional problems contribute to pneumonia being the leading acute cause of death among people with dementia. Because of the way in which deaths are reported, it can be difficult to obtain an accurate number of how many people die with dementia versus die from dementia each year (
5). In the case that follows, we discuss the functional decline seen toward the end of life of a patient with dementia and discuss the importance of palliative care in overall clinical management.
Case Study: Mr. A
Mr. A was an 84-year-old assisted living facility resident with major neurocognitive disorder who presented to the emergency department with severe behaviors unmanageable in his facility. He had moved into the assisted living facility 6 months earlier and had experienced increasing behavioral disturbance and functional decline over the 3 months before presentation. His medical history included coronary artery disease, cerebrovascular disease, recurrent urinary tract infections, and traumatic brain injury. Mr. A had been diagnosed 3 years earlier with multifactorial major neurocognitive disorder (elements of vascular, Alzheimer’s, and Lewy body dementia) after consultations with neurology and psychiatry. Mr. A had a medical power of attorney in place and an advance directive specifying his code status as do not resuscitate and do not intubate.
He was admitted to a medical floor, where a medical evaluation (blood counts, electrolytes, head computed tomography) was unremarkable. A urinalysis was indeterminate for urinary tract infection, and he was treated empirically. His family was involved throughout his hospitalization and recognized his need for an increased level of care after discharge.
Mr. A spent the next several weeks hospitalized on the medical service. He struggled with severe agitation, assaulted a care aide, and attempted elopement from the hospital several times. His sleep-wake reversal, distressing hallucinations, and fluctuating confusion suggested delirium or Lewy body dementia. He was treated with trials of quetiapine, mirtazapine, citalopram, lorazepam, haloperidol, olanzapine, and rivastigmine, targeting agitation. The medical team aggressively cared for his medical needs (acute kidney injury secondary to poor oral intake, intermittent constipation, and urinary retention) and made every attempt to reverse potentially reversible problems driving delirium.
Several weeks after admission, Mr. A was transferred to inpatient psychiatry with ongoing treatment-resistant agitation and aggression. The psychiatry team felt that his medical care had been optimized and assessed that Mr. A was likely at a new functional baseline with underlying neurodegenerative disorder. Palliative care was consulted with a question regarding hospice eligibility and for assistance in delineating goals of care. During this conversation, Mr. A’s family expressed his previously stated desire to not want to live with a poor quality of life such as he had witnessed other family members with dementia endure. Mr. A was found to qualify for hospice due to significant weight loss over the preceding months, functional decline, and Functional Assessment Staging (FAST) score of 7 (explained in the “Prognostication in Dementia” section). Hospice was agreed to be in line with his goals of care. A search was begun for memory care or skilled nursing placement with hospice support. In the meantime, comfort care was initiated, and he was transferred to inpatient hospice, where he passed away just 1 week later. Autopsy revealed the cause of death to be complications from neurodegenerative disorder, with underlying Alzheimer’s-type pathology, alpha-synuclein deposits consistent with Lewy body dementia, and cerebrovascular disease.
Mr. A’s case demonstrates the common occurrence of a significant delay in providing palliative care services to a patient with a life-limiting illness and multiple palliative needs. In the following sections, we discuss the primary tenets of palliative care, symptom and functional assessment, and identification of patients in need, and we explore barriers to its use.
Palliative Care Definition and Philosophy
There are multiple definitions of
palliative care from leading organizations in the field of palliative medicine.
Palliative care is defined by the World Health Organization as
an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial, or spiritual. (
8)
Several other definitions of palliative care are included in the online supplement. Each definition focuses on treating both the patient with serious illness and the family. The illness may be severe but potentially reversible, or the illness may be progressive and irreversible. Regardless of disease trajectory, the aim of palliative care is to alleviate suffering.
Palliative care has been shown to improve quality of life, decrease hospitalizations, improve family satisfaction with end-of-life care, and decrease health care costs, and in some cases it may prolong life (
9–
14). Goals of palliative care include relieving pain and suffering (physical and emotional), affirming life and regarding dying as a normal process, integrating biopsychosociospiritual care, helping patients live as actively as possible until death, supporting the family, and offering bereavement support (
8). These goals are met through multidimensional assessment and management with an interdisciplinary care team approach.
Palliative care can be delivered in a variety of settings, including hospital-based palliative care programs, long-term-care facilities, and community-based palliative care services. Palliative care services and staff must continuously adapt their model of care and interventions to the specific needs and values of each patient. Palliative care can also be divided into primary palliative care and specialty palliative care.
Primary palliative care often refers to care by providers who care for chronically ill patients (e.g., internists, oncologists, cardiologists), and they should be able to address the basic tenets of palliative care. These include basic symptom management, code status discussions, exploring psychosocial distress, and care coordination. More complicated symptom and psychosocial management may require assistance from clinicians specifically trained in palliative care—termed
subspecialty palliative care (
15,
16).
Table 1 outlines the levels of palliative care from basic symptom management by any clinician to the most specialized care in tertiary care settings (
15,
16). Although many clinicians will perform basic palliative care management, knowing when to get more specialized clinicians involved is also important. We address this in further detail later.
Comparison With Hospice Care
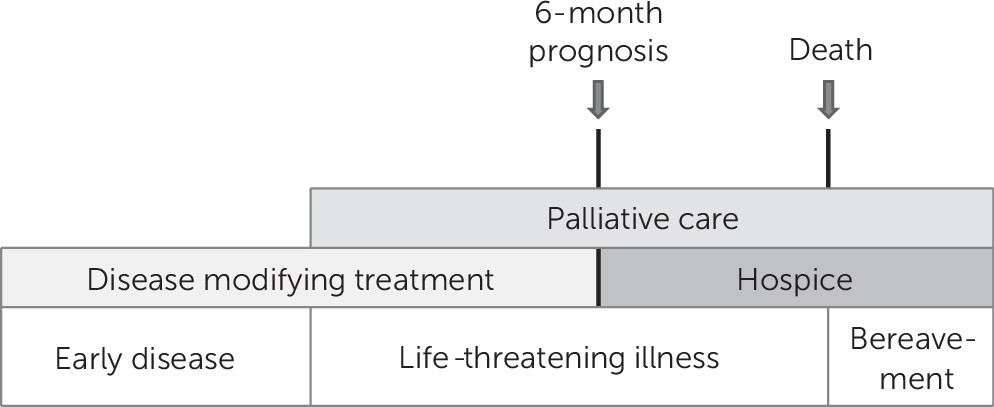
Palliative care differs from hospice care in important ways. As outlined in
Figure 2, whereas hospice care focuses on providing support in the last 6 months of life and requires the cessation of life-prolonging treatment, palliative care should ideally be incorporated early in the course of a life-threatening illness, in conjunction with life-prolonging medical therapies such as chemotherapy. Early integration of palliative care allows for management of distressing symptoms and enhancing quality of life alongside disease-directed therapies. It also improves support for family members, addresses social needs throughout the course of illness, and aids in a timelier transition to hospice care (
17–
19).
Barriers to Palliative Care Utilization
There are several barriers to palliative care referrals and optimization of end-of-life care, including limited provider and patient education, perception and stigma, and access to services (
20).
Two public polls found that three-quarters of people surveyed had never heard of palliative care; however, once they were informed about the services, most said they would consider palliative care if facing a serious illness (
21,
22). For physicians, the historical dichotomous model of medical care (in which comfort care is only provided when disease-modifying treatment is no longer appropriate) as well as the negative stigma associated with the term
palliative care leads to barriers to early referral (
20,
22). Studies have shown that health care providers view the terms
palliative care and
hospice care as synonymous and associate palliative care with death and hopelessness (
20). Access to palliative care is increasing in hospitals across the country, but a need remains to continue expanding community-based access, especially in rural communities (
21). To decrease barriers, it is important to increase education about palliative care philosophies and benefits for both patients and providers and to continue to increase access. Effective communication with patients about their prognosis, goals of care, and treatment opportunities, including palliative care treatment, is imperative to maximize quality of care for patients with life-threatening illnesses.
Palliative Care Assessment and Management
Identifying Individuals With Palliative Needs
Palliative care assessment and treatment is often grouped into domains that address physical symptoms, psychological and cognitive symptoms, spiritual concerns, social needs, understanding of illness and prognosis, goals of care, and care coordination (
16). Identifying those in need of a palliative assessment is imperative. The Center to Advance Palliative Care has proposed criteria to identify hospitalized patients who would benefit from palliative care assessment. Primary criteria assess global indications that a patient may have palliative care needs, whereas secondary criteria are more specific and, if positive, indicate a high likelihood of palliative care needs. If patients are identified as having a life-limiting or life-threatening condition at the time of hospital admission and meet primary or secondary criteria, referral to palliative care should be considered because the patient may have unmet needs (
16).
On admission, primary criteria to consider include whether one would be surprised if the patient died in the next 12 months; whether the patient has had recurrent hospitalizations, difficult-to-control symptoms, or complex care requirements; and whether the patient has had functional decline. For example, in the case of Mr. A, he had a life-limiting illness (dementia), it would not have been surprising if he died within 12 months (he died within 1 month), his behavioral symptoms were difficult to control, he needed complex care, and he had a functional decline over the preceding 3 months. Had these criteria been considered at the time of his admission, he likely would have received a timelier referral to palliative care and likely undergone less invasive medical care that aligned with his goals of care. Secondary criteria that may indicate the need for palliative assessment include living in a long-term-care facility, cognitive impairment, hip fracture, terminal cancer, home oxygen requirement, limited social support, and need for advance care planning, among other considerations (
16). These needs should be assessed not only on admission, but also throughout the course of hospitalization. Daily assessment considerations should include, but are not limited to, how long the patient has been in the intensive care unit, whether the patient has clearly outlined and documented goals of care or whether there is uncertainty about treatment decisions, whether the patient or the patient’s support system is experiencing emotional or spiritual distress, or whether long-term invasive medical treatments are being considered (
16). If there are concerns with any of these daily assessments, then palliative care referral should be considered.
Ideally, assessment of palliative care needs is first undertaken by the primary team caring for the patient, and if complex issues are identified that require more specialty-level palliative care, then a consultation may be placed. Although the criteria outlined here were designed for hospitalized patients, a similar approach can be taken when seeing patients in the outpatient setting or long-term-care facility.
Coming back to Mr. A, dementia is a life-limiting condition that ideally could have warranted involvement with palliative care in the outpatient setting. Although involved late in his care, the palliative care team and approach was invaluable in assisting Mr. A’s family with communication, end-of-life education and support, and relieving pain and suffering in his final days.
Evaluation and Management of Distressing Symptoms
Living with a life-threatening illness may lead to prolonged pain and suffering for both patients and their families, leading to decreased quality of life and survival. This suffering is not only physical in nature but also psychological and spiritual. Common physical symptoms include pain, nausea, dyspnea, fatigue, and constipation. Depression, anxiety, panic, agitation, isolation, and hopelessness are frequent psychological reactions. Spiritually, patients may experience a loss of purpose or meaning. Social relationships can be strained, and families or caregivers are at risk of exhaustion, burnout, and poorer quality of life. To relieve suffering among patients and families, a multidimensional, individualized assessment is needed to understand the patient’s and family’s unique needs for symptom control and goals of care (
23).
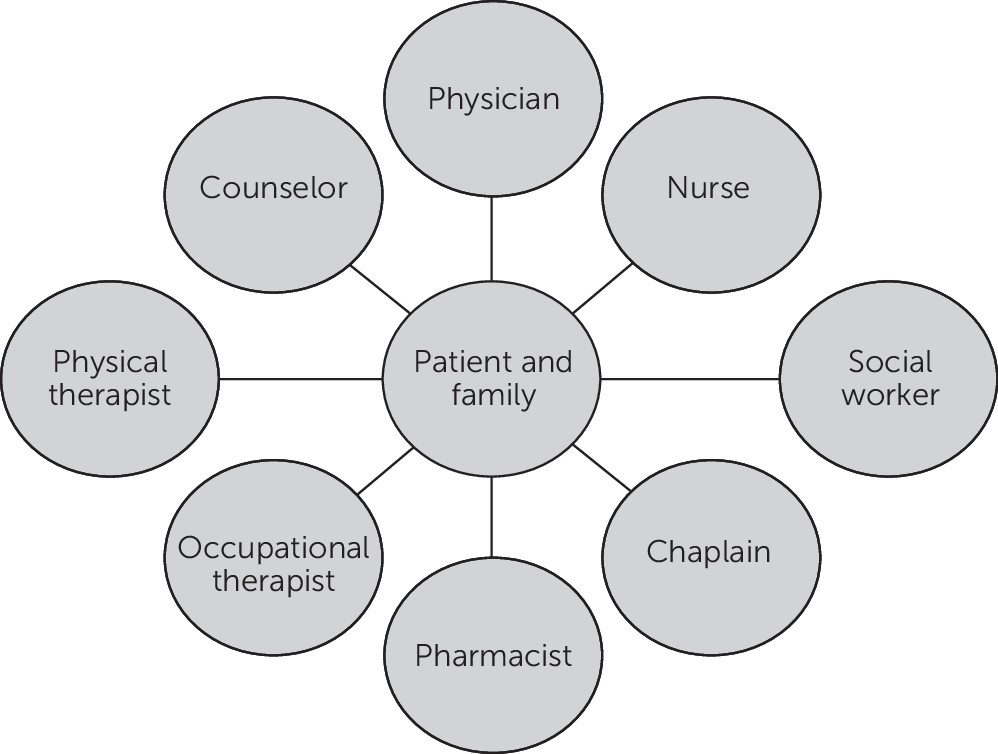
An initial evaluation should include obtaining a medical and surgical history, allergies, pertinent tests and imaging, a thorough review of pertinent diagnoses, and a timeline of illness progression and historic therapeutic modalities. A more comprehensive evaluation is essential to identify further areas of need (
23). Proper assessment and management require a multidisciplinary team, often consisting of physicians, nurses, social workers, chaplains, occupational therapists, physiotherapists, pharmacists, counselors, dieticians, and volunteers, as shown in
Figure 3.
A comprehensive assessment includes several domains: pain and physical symptoms, psychological and cognitive symptoms, understanding of illness and goals of care, social and economic resource needs, spiritual and existential distress, and care coordination (
24,
25). Several standardized scales are available to aid in the assessment of symptoms and needs (
Table 2).
Pain and physical symptoms.
In the assessment of pain and physical symptoms, close attention should be paid to assessing confusion, insomnia, shortness of breath, anorexia, nausea, constipation or diarrhea, and fatigue, which are some of the most common symptoms present in chronic illnesses (
26). Characterization of symptoms is necessary, including onset, location, duration, alleviating and aggravating factors, and severity. The Edmonton Symptom Assessment Scale can be used in the clinical setting to evaluate the degree of severity of some of the most common symptoms (
23).
Psychological and cognitive symptoms.
Psychiatrists will be well adept at evaluating psychological and cognitive symptoms. Mood disorders are particularly prevalent among chronically ill patients and may be associated with a high risk of mortality (
27). Aside from standard interview techniques, tools such as the Hospital Anxiety and Depression Scale can be self-administered to rate patients’ degree of distress (
23). It is important to identify adaptive and maladaptive coping strategies used by patients. Adaptive coping skills such as humor, sublimation, and acceptance should be recognized and reinforced by clinicians (
28,
29).
Delirium is a common and potentially reversible cause of altered mental status in severely ill patients, and psychiatrists are adept at assessing it. Frequently used assessments include the Montreal Cognitive Assessment (
30), the Confusion Assessment Method (
31), and the Clock Drawing test.
Understanding of illness and goals of care.
It is essential to assess patients’ understanding of their illness in combination with their goals for care (reviewed in more detail in the next section). Ideally, therapeutic interventions should closely align with the patient’s preferences, noting that goals of care may change over time. If there is a concern about a patient’s decision-making capacity, a capacity assessment should be performed. An evaluation should include whether the patient is able to understand information about the treatment, the consequences of accepting or refusing a treatment, manipulation of information and to consistently communicate choice (
32). Mr. A’s goals of care and assignment of a power of attorney had been completed early in his course of illness when he still had capacity, which aided his family in their discussions with the palliative care team during his final weeks of life.
Spiritual distress.
Evaluations regarding goals of care may naturally lead to discussions of spiritual and existential distress. Some patients faced with mortality may experience differing levels of distress. These experiences may result in spiritual turmoil as well. As physicians, psychiatrists’ focus should be on understanding how their patients’ spiritual beliefs may affect their goals of care and their coping abilities. Deeper questions regarding spirituality should be discussed with a chaplain (
23).
Social and economic needs.
Social and economic resource needs should be identified early in treatment. In some cases, financial and social support constraints may significantly alter the treatment choices patients and their families make (
33,
34). Social worker involvement may be beneficial in identifying areas of need and potential resources. In addition, caregivers are at risk for decreased quality of life, stress, exhaustion, and burnout (
35). Assessment of both the patient’s and the caregivers’ experiences is crucial in understanding their complete needs.
Care coordination.
Continuity of care is beneficial for the patient but is not always possible in the confines of the complex US health care system. Identifying and minimizing potential gaps in care can decrease medical error and morbidity (
36,
37). An interdisciplinary approach to care may alleviate some of the gaps and provide a more comprehensive treatment plan for patients.
Goals-of-Care Discussion
Patients with serious, life-threatening illnesses face many choices and challenges in coping with their diagnosis and treatment options. Establishing a person’s goals of care requires an understanding of the values and preferences that shape their desire for current and future medical treatments. These goals are used in advance care planning with patients to determine what treatments they may or may not want to undergo in the future, who they choose as their surrogate decision maker, and what nonmedical goals they hold. Having clear and compassionate discussions about a patient’s goals of care early and often during the course of treatment for a serious illness will allow them to obtain care that best aligns with their values (
38).
Multiple factors come into play for patients deciding their next steps in treatment, such as the severity of the disease, prognosis, and their personal values and preferences. Some may prefer to undergo rigorous treatment to maximize their length of life, and others may choose to forego certain treatment options to focus on quality of life in the time they have left.
When and how to have a goals-of-care conversation is important to consider. Ideally, the conversation should be started with a long-term-care provider who knows the patient and family well. This first conversation should happen early in the disease course, but preferably not on the same day that the news about a serious illness is delivered. It is important that the conversation not be rushed, that distractions be minimized, and that all important parties (e.g., family members, decision makers) be present for the conversation. This conversation should be revisited throughout the patient’s treatment to ensure the treatment still aligns with the patient’s goals. It is especially crucial to revisit this conversation at transition points in care, such as a change in prognosis or before a major treatment (
38,
39).
Despite best efforts, goals of care and advance care planning discussions often occur more acutely during hospitalization. In this situation, the conversation will likely be initiated by a provider who is relatively new to the patient’s care. It is important to still give proper time and space to these discussions, and palliative care consultation can be considered for additional support with these conversations.
Whether goals-of-care discussions are started by a long-term provider, hospitalist, or palliative care provider, a structured approach to the discussion should be taken. One common protocol that is used is the six-step SPIKES protocol (
40,
41), summarized in
Box 1.
Gaining a clear understanding of the patient’s goals for care is imperative for advance care planning and can aid the surrogate decision maker when the patient cannot make decisions for themselves. It has been shown that advance care planning increases the likelihood of compliance with patient wishes, improves quality-of-care satisfaction, and increases the family’s understanding of the dying process, among multiple other outcome improvements. In psychiatry, advance care planning can also decrease the risk of stress, anxiety, and depression among the patient’s family members (
42).
Prognostication in Dementia
Special consideration and assessment of functional decline among those with dementia is also important for the geropsychiatrist. The stages of dementia are mild, moderate, severe, and end stage. Prognosis is poor in end-stage dementia, and although life expectancy is short, it is very difficult to estimate. There are existing tools that help prognosticate and estimate survival, although these tools are known to be accurate only in the most advanced or end stages of a disease.
Although many tools are available to assess cognitive and functional decline, one of the most widely used and validated assessment tools is FAST (
43). FAST categorizes functional abilities and performance of tasks of daily living into seven levels, ranging from normal to end-stage dementia. Eligibility for hospice on the basis of dementia is a FAST level 7C, or a FAST level 7A with at least one of six dementia-related comorbid conditions over the previous 12 months (aspiration pneumonia, pyelonephritis or other upper urinary tract infection, septicemia, multiple decubitus ulcers higher than stage 3, recurrent fever after antibiotics, and severe eating problems or tube feeding accompanied by a more than 10% weight loss over the past 6 months or serum albumin <2.5 g/dL) (
44). In our case, Mr. A had level 7A with both upper urinary tract infection and greater than 10% weight loss over the past 6 months. A small study of patients enrolled in hospice for dementia showed a mean survival of 3.2 months for those who were at level 7C or higher (
45). The Mortality Risk Index uses risk factors for mortality from the Minimum Data Set, with a Mortality Risk Index score ≥12 showing a greater predictive value for 6-month prognosis than a FAST level 7C (
46). The Advanced Dementia Prognostic Tool is another tool found to have better performance to estimate 6-month survival among people with advanced dementia than current hospice eligibility guidelines (
47).
End-stage dementia is a terminal illness and a natural fit for hospice care. End-of-life care among people with dementia can be enhanced with the recognition of dementia as a terminal illness, knowledge of prognosis and estimates of life expectancy, discussion and delineation of goals of care, advance care planning, and a focus on providing relief and optimizing the quality of life of persons with dementia, and their caregivers, at the end of life.
Coronavirus Disease 2019 Context
It has been over a year since the beginning of the global pandemic, and the negative impact of COVID-19 on individuals and communities is now well established. Older individuals are at particularly high risk for severe outcomes from COVID-19, including more severe illness, hospitalization, and death (
48). Persons with dementia who have COVID-19 infection have a higher mortality risk than those without dementia (
49). The social isolation from closures and lockdowns has had a disproportionately negative affect on the Alzheimer’s community (
50). Isolation has also affected families’ and caregivers’ ability to connect with their loved ones with this illness. For the geriatric population, it is especially important to proactively discuss the increased morbidity and mortality associated with COVID-19 infection, engage in goals of care and advance care planning to determine the desired level of treatment, and continue supporting families and caregivers (
51,
52). One study from Philadelphia that evaluated palliative care utilization in March-April 2020 identified underutilization of palliative care services among the population of people with COVID-19, elucidating a need for stronger advocacy for patients to receive necessary palliative services (
53). To maximize palliative care services with a limited number of resources, it is important to use technology such as telemedicine to connect to patients and families and to continue educating primary teams about how to manage the basics of palliative care (
54). Geropsychiatrists are uniquely qualified to help identify and manage the psychological distress patients and families may face, in addition to helping to educate and advocate for palliative care interventions.
Conclusions
Palliative care is a care approach that aims to reduce suffering and improve quality of life among patients who are facing a life-threatening illness and their family members. This approach is consistent with the goal in geriatric psychiatry to relieve distress and suffering among older adults with mental disorders. Geriatric psychiatrists can make a significant contribution to enhancing the quality of care that older psychiatric patients receive at the end of life by adopting relevant palliative care approaches when appropriate and identifying when more specialized consultation is needed. This is especially important in the context of the aging population and in end-of-life care during the pandemic.