Borderline Personality Disorder: Updates in a Postpandemic World
Abstract
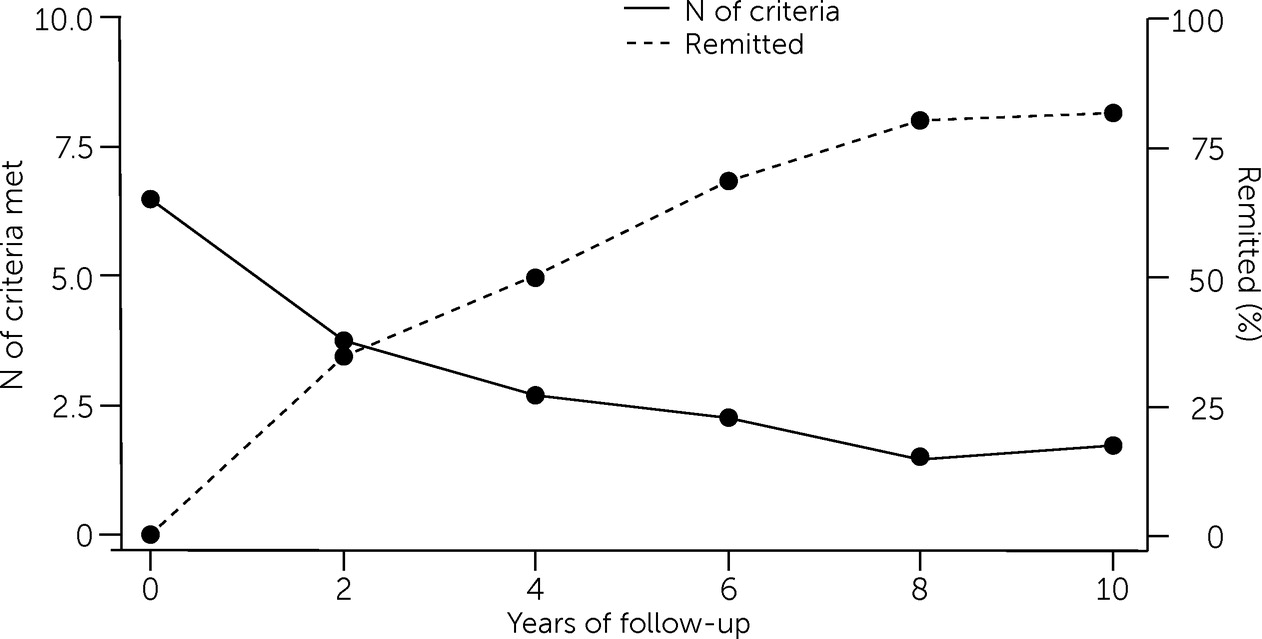
Basic Facts: Definitions, Epidemiology, Longitudinal Course
| Variable or assessment | Measure or population |
|---|---|
| Epidemiology % in adults (% in adolescents) (14, 15, 23, 32) | |
| General population | 2.7% (1%–3%) |
| Psychiatric inpatients | 20%–25% (33%–49%) |
| Psychiatric outpatients | 8%–18% (11%–22%) |
| Emergency room visits with suicidal ideation | 56% (88%) |
| Suicidal behavior (3, 5, 16) | |
| Average number of attempts | 3 |
| Suicide | 3%–10% (50×greater than among general population) |
| Proportion of all suicides with borderline personality disorder | 18% of all suicides; 33% of all youth suicides |
| Cost to society (10, 33) | |
| Indirect costs of lost productivity (Europe) | $12,484–$50,000 |
| Risk for disability with borderline personality symptoms<19 | 15-fold |
| Risk for unemployment with borderline personality symptoms<19 | 22-fold |
| Psychosocial functioning (24–37) | |
| Functional impairment and changes in symptom levels | Good premorbid function provides positive prognosis; remission predicts good functioning |
| Poorer interpersonal functioning | Improvement in close relationships occurs with reduction in borderline personality disorder symptoms |
| Assessments | |
| Semi-structured interviews or clinician rated | |
| Structured Clinical Interview for DSM-5 Personality Disorders | All personality disorders |
| Diagnostic Interview for DSM-IV Personality Disorders | All personality disorders |
| International Personality Disorders Examination | All personality disorders in DSM-IV and ICD-10 |
| Revised Diagnostic Interview for Borderlines | Borderline personality disorder only |
| Diagnostic self-reports | |
| Personality Diagnostic Questionnaire-4 | All personality disorders |
| Personality Assessment Inventory | All personality disorders |
| Borderline Symptom List | Borderline personality disorder only |
| Five-Factor Borderline Inventory | Borderline personality disorder only |
| Screening self-reports for borderline personality disorder | |
| McLean Screening Instrument for borderline personality disorder | |
| Borderline Personality Questionnaire | |
| Zanarini Rating Scale for BPD | |
| Dimensional personality functioning assessment | |
| Personality Inventory for DSM-5 | Personality traits |
| Level of Personality Functioning Scale Self-Report | Personality functioning |
Controversies: Dimensional Versus Categorical Diagnosis
| Psychiatric disorder | Odds ratio (controlled for sociodemographic characteristics) | 99% CI | Odds ratio (unadjusted) | 99% CI |
|---|---|---|---|---|
| Any substance use disorder | 3.2* | 2.73–3.97 | 4.50 | 3.57–5.71 |
| Any drug use disorder | 4.0* | 3.30–4.72 | 5.78 | 4.67–7.14 |
| Any anxiety disorder | 7.7* | 6.51–9.19 | 14.29* | 10.87–18.87 |
| Any mood disorder | 9.1* | 7.71–10.78 | 14.93* | 11.63–19.61 |
| Major depressive disorder | 2.5* | 2.07–2.90 | 11.76* | 9.35–14.93 |
| Dysthymia | 3.2* | 2.51–4.16 | 8.33* | 6.62–10.53 |
| Bipolar I | 9.9* | 8.11–12.01 | 16.39* | 13.33–20.41 |
| Bipolar II | 4.3* | 3.00–6.03 | 3.70* | 2.71–5.05 |
| Any other personality disorder | 12.5* | 10.54–14.86 | 15.87* | 12.82–19.61 |
| Paranoid | 5.8* | 4.69–7.25 | 12.20* | 8.93–16.39 |
| Schizoid | 4.5* | 3.55–5.76 | 14.29* | 8.40–24.39 |
| Schizotypala | 26.5* | 21.53–32.68 | 111.11* | 66.67–200.00 |
| Antisocial | 3.5* | 2.71–4.40 | 6.33* | 4.76–8.40 |
| Histrionic | 6.5* | 4.90–8.52 | 14.49* | 6.85–31.25 |
| Narcissistic | 14.5* | 12.12–17.42 | 55.56* | 40.00–83.33 |
| Avoidant | 7.2* | 5.45–9.56 | 11.63* | 7.87–17.24 |
| Dependent | 8.2* | 4.65–14.46 | 20.41* | 9.71–41.67 |
| Obsessive-compulsive | 3.7 | 3.06–4.52 | 7.75* | 5.65–10.64 |
| Variable | ICD-11 | DSM-5 AMPD | HiTOP |
|---|---|---|---|
| Components of global personality disorder severity | Global severity: self- and interpersonal functioning, risk of harm to self and/or others | Criterion A: self- and interpersonal functioning | Superspectra: general psychopathology severity (p factor) |
| Specific and/or stylistic trait domains | Trait qualifiers: negative affectivity, detachment, dissociality, disinhibition, anankastia | Criterion B trait domains: negative affectivity, detachment, antagonism, disinhibition, psychoticism | Spectra: internalizing, detachment, antagonistic externalizing, disinhibited externalizing, thought disorder, somatoform (provisional) |
Neuroimaging Advances
The Frontolimbic Hypothesis: Shared or Distinct Neurobiological Disruptions?
| Model supported | Citation | Sample | Method | Analysis or aims | Summary | Implications |
|---|---|---|---|---|---|---|
| Dimensional neurobiological model | Baranger et al., 2020 (62) | N=1,398 scans from the Duke Neurogenetics Study and Human Connectome Project | Structural MRI | 152 structural metrics examined (e.g., cortical thickness, cortical surface area, subcortical volumes) | Borderline traits not associated with any of 152 structural metrics investigated | Traits that are specific to borderline pathology are not associated with brain structure |
| Degasperi et al., 2021 (63) | 52 studies N=1,104 borderline personality disorder and 1,100 control participants | Task-based fMRI (any task) | Activation likelihood estimation meta-analysis | No clusters of significant convergence or differences identified during the performance of any task; when analyses were restricted to emotion processing tasks; two significant clusters of greater activation, in borderline personality disorder vs. controls, in amygdalate and ACC | Borderline-specific pathology is not associated broadly with brain function during fMRI task performance | |
| Traynor et al., 2021 (64) | N=45 borderline personality disorder and 29 control participants | Resting-state fMRI | Connectivity analysis | Limbic system connectivity strength in borderline personality disorder significantly associated with severity of impairments in dimensional self- and interpersonal functioning (DSM-5 AMPD criterion A); typology-specific measure of borderline personality disorder symptom severity not significantly associated with any resting-state connectivity patterns | Limbic system disruptions are related to dimensional psychopathology impairments and are not borderline personality disorder–specific | |
| van Zutphen et al., 2017 (65); van Zutphen et al., 2020 (66) | N=51 borderline personality disorder, 26 cluster C, and 44 nonpatient control participants | Task-based fMRI (emotion processing task and affective inhibitory control task) | Activation analysis | Insula and TPJ hyperactivation during emotion processing in borderline personality disorder vs. other groups; hyperactivation in FEF and IPL during inhibition of negative vs. neutral stimuli, in borderline personality disorder vs. other groups; activation differences showed significant linear trend related to diagnostic severity vs. category | Differences in brain activation may be related more to the severity of psychopathology vs. diagnostic category | |
| Kebets et al., 2021 (67) | 166 females with borderline personality disorder, bipolar disorder, or ADHD | Resting-state fMRI | Partial least squares analysis of resting-state signal variability | Frontolimbic network signal variability associated with emotion dysregulation across disorders; severity of emotion dysregulation accounted for 74% of shared variance in frontolimbic signal; depression and mania severity not associated with frontolimbic signal | Emotion dysregulation-related frontolimbic function is shared across disorders and not specific to borderline personality disorder | |
| Bilek et al., 2019 (68) | N=120 borderline personality disorder vs. 115 control participants | Task-based fMRI (threat processing task) | Activation analysis | Significant reduction in amygdala habituation to threat processing in borderline personality disorder vs. controls; effect unrelated to borderline personality disorder symptom severity or category but significantly associated with severity of childhood adversity | Abnormalities in brain activation during threat processing may be related more to severity of early adversity vs. categorical borderline personality diagnosis | |
| Metz et al., 2019 (69) | N=18 borderline personality disorder, 20 PTSD, 40 control participants | Task-based fMRI | RCT of autobiographical memory (AM) retrieval after administration of 10 mg of hydrocortisone or placebo | No between-group differences in neural activation during AM retrieval after hydrocortisone or placebo; hydrocortisone effects on amPFC, vlPFC, PCC, angular gyrus, and cerebellum positively correlated with childhood trauma questionnaire scores | Hydrocortisone-induced neural activation during AM retrieval is related to childhood trauma (vs. borderline personality disorder diagnosis) | |
| Schaub et al., 2021 (70) | N=313 with borderline personality disorder, cocaine use disorder, opioid use disorder, major depressive disorder, schizophrenia, or first-episode psychosis | Structural MRI | Examined associations between anhedonia and gray matter volume | Negative associations found between volumes of left putamen and bilateral cerebellum with anhedonia scores across disorders | Clinical problems, such as anhedonia, have shared neurobiological substrates across borderline personality disorder and other disorders | |
| Neukel et al., 2021 (71) | N=45 borderline personality disorder and 25 control participants | Task-based fMRI (emotion processing task) | Activation analysis | Abnormal precuneus activation during emotion processing of neutral and fearful stimuli in borderline personality disorder related to severity of impairments in self- and interpersonal functioning (DSM-5 AMPD criterion A) | Abnormalities in emotion-related brain activation may be related more to severity of psychopathology vs. diagnostic category | |
| Cremers et al., 2021 (72) | N=51 borderline personality disorder, 26 cluster C, and 44 nonpatient control participants | Task-based fMRI (emotion regulation task) | Support vector machine classification of borderline personality disorder | Unable to classify borderline personality disorder with high accuracy by using brain activation during emotion regulation; 55% classification accuracy was not statistically significant under permutation model | Brain activation during emotion regulation cannot be used to distinguish individuals with borderline personality disorder from those without the disorder | |
| Hybrid dimensional-categorical neurobiological model | Yu et al., 2019 (73) | 13 borderline personality disorder studies (N=395 borderline personality disorder and 415 control participants) and 47 bipolar disorder studies (N=2,111 bipolar disorder and 3,261 control participants) | Structural MRI | Meta-analysis of gray matter volume and density in borderline personality disorder vs. bipolar disorder | Shared: decreased gray matter volume and density in right medial OFC; specific to borderline personality disorder: decreased gray matter volume and density in amygdala and right parahippocampal gyrus; specific to bipolar disorder: decreased gray matter volume and density in right insula and thalamus and increased volume and density in right putamen (and putamen volume correlated with young mania rating scale scores) | Borderline personality disorder and bipolar disorder have both shared and distinct neural substrates |
| Lou et al., 2021 (74) | 15 borderline personality disorder datasets (N=442 borderline personality disorder and 441 control participants) and 11 PTSD datasets (N=214 PTSD and 258 control participants) | Structural MRI | Meta-analysis of gray matter volume in borderline personality disorder vs. PTSD | Shared: gray matter volume reductions in orbitofrontal gyrus and anterior cingulate cortex; specific to borderline personality disorder: gray matter volume increases in PCC/precuneus; specific to PTSD: gray matter volume decreases in amygdala and hippocampus | Borderline personality disorder and PTSD have both shared and distinct neural substrates | |
| De la Peña-Arteaga et al., 2021 (75) | N=19 borderline personality disorder, 20 major depressive disorder, and 19 control participants | Task-based fMRI (cognitive reappraisal task) | Activation analysis | Shared: decreased vlPFC activation during cognitive reappraisal; specific to major depressive disorder: overall prefrontal hypoactivation; specific to borderline personality disorder: abnormalities attributed to connectivity disruptions between vlPFC and temporal regions | Borderline personality disorder and major depressive disorder both have shared and distinct neural substrates |
Interpersonal Hypersensitivity, Negative Affectivity, and the Default Mode Network (DMN)
Biomarkers of Aggression and Hostility in Borderline Personality Disorder
Self-Harm in Borderline Personality Disorder and Biomarkers of Psychotherapy Outcomes
Treatment
Psychotherapy
Pharmacology and Novel Brain-Based Therapeutics
Conclusions
REFERENCES
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing PsychiatryOnline@psych.org or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).