To the Editor: Delusional misidentification syndromes (DMS) are conditions in which affected individuals falsely believe that the identity of a person, object, or place has been altered. The most common DMS is the Capgras delusion, which is the belief that a person or persons have been replaced by imposters; 25%–40% of DMS cases have an identifiable neurological etiology.
1 One specific type of misidentification, the “phantom boarder symptom” (PBS), in which affected individuals imagine that there are people in the home, has been identified in >20% of dementia patients.
2 We report on a case of DMS associated with right-hemisphere dysfunction that most closely resembles PBS.
Case Report
“Mr. S.,” a 63-year-old right-handed man with a history of posttraumatic stress disorder (PTSD) and alcohol dependence, was referred for evaluation of psychosis. He was living independently and employed as an aircraft maintenance engineer until a motor vehicle accident (MVA) 3 years earlier. Mr. S. was drunk-driving and sustained a severe traumatic brain injury (TBI) and several long-bone fractures. He was unconscious for several days while in an ICU. After hospital discharge, Mr. S. began living with a sister while engaged in physical rehabilitation. His cognitive and functional status progressively declined, with his family noticing concentration and comprehension difficulties, affective lability, and wandering from the house. He became apathetic and needed guidance to carry out some ADLs. He also developed visual hallucinations and delusional misidentification of his brother, C., who lives approximately 200 miles away. Mr. S. would consistently report seeing C. when looking in a mirror, and his sister rearranged and covered mirrors to reduce the frequency of this misidentification. He also reported spending time with C. on a daily basis, performing activities such as shopping, riding the bus, and purchasing two meals at fast-food restaurants. He emphatically denied that C. had been doubled and confabulated explanations for C.'s visiting and why C. could not reveal himself to family members or physicians.
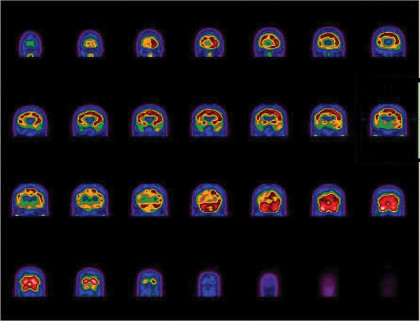
Mr. S.'s mental status exam was notable for blunted affect, slowed cognition, concrete thinking, indifference, and lack of insight. Mini-Mental State Exam (MMSE) score was 16/30. Neuropsychological testing revealed severe global cognitive impairments, executive dysfunction, and constructional apraxia. Routine laboratory studies were unremarkable. EEG showed diffuse, irregular delta/theta slowing bilaterally. Brain MRI showed diffuse cortical atrophy. Brain SPECT revealed a marked decrease in activity throughout the right hemisphere, most prominently in the frontal and superior parietal lobes (
Figure 1). Mr. S.'s condition was refractory to treatment with quetiapine.
DMS provide a testable model for the neurology of psychosis and are predominantly associated with right-hemispheric lesions.
1 Similar to our patient, a previous report found progressive dementia associated with visual hallucinations and multiple symptoms of misidentification, to include PBS, with right-hemisphere hypoperfusion on SPECT.
3 Right-hemisphere cortical involvement presumably prevents patients with DMS from rejecting anomalous sensory information originating in the parietal and temporal areas.
4,5 Objective neuropsychological dysfunction, however, cannot fully explain the specificity and intensity of delusions of misidentification.
6 A case study on the emergence of delusional companions in patients with right-hemisphere hypoperfusion by SPECT highlighted the contributions of neurobiological, cognitive, and emotional factors to the development of specific misidentifications.
7 Moreover, right-hemisphere dysfunction does not elucidate the precise etiology of our patient's cognitive and functional decline. His decline probably represents a convergence of multiple injuries, including chronic alcohol dependence, the temporally-related MVA and subsequent TBI, and a possible neurodegenerative process.
This case supports the previously established link between DMS and right-hemisphere dysfunction and encourages providers and researchers to consider the underpinnings of specific misidentifications as well as the diagnostic and treatment challenges inherent to patients with DMS.
Acknowledgments
A portion of this manuscript was presented at the 20th Annual Meeting of the American Neuropsychiatric Association, San Antonio, TX, February 19–22, 2009. An abstract was published in the meeting materials.
The authors report no financial relationships with commercial interests. Dr. Thode has an active-duty affiliation with the United States Air Force. The opinions expressed in this document are solely those of the authors and do not represent an endorsement by or the views of the United States Air Force, the Department of Defense, or the United States Government.