Treatment-resistant depression occurs in 50%–60% of depression patients.
1 Of these, a small but unknown percentage will remain unresponsive to all available interventions, including psychotherapy, pharmacotherapy, and ECT. For this small group of patients, limbic surgery is one of the few treatment options that remain. The surgical targets that are utilized vary across institutions and involve lesions produced bilaterally in the anterior limb of the internal capsule (anterior capsulotomy), the supragenual anterior cingulate gyrus and cingulum (anterior cingulotomy), and the subgenual anterior cingulate gyrus and subcortical orbitofrontal white matter (subcaudate tractotomy).
2,3 The combination of bilateral cingulotomy and subcaudate tractotomy is known as limbic leucotomy.
4Methods
In 1998, the Vancouver Limbic Surgery Group (VLSG) was formed as a clinical program to offer surgical treatment for refractory depression and obsessive-compulsive disorder. Bilateral anterior capsulotomy (BAC) was selected as the target after reviewing the available literature and the benefit that two British Columbian patients with major depressive disorder (MDD) had had from this procedure done at another center. In 2000, the first patient underwent BAC. This report details the experience of the Vancouver Limbic Surgery Group with BAC for intractable depression and reports on the eight patients, all of whom have been followed for at least 24 months.
The proposed limbic surgery protocol was reviewed and approved by the Department of Psychiatry, the Division of Neurosurgery University of British Columbia, and the Vancouver Hospital and Health Sciences Centre’s Medical Advisory Board and Ethics Committees. The inclusion and exclusion criteria are listed in
Table 1 and
Table 2. All patients must have had persistent, unremitting, severe depression for 5 consecutive years and have failed multiple medication trials that must include a tricyclic antidepressant and a monoamine oxidase inhibitor. Each medication must have been taken at the maximum or close to the maximum dose for at least 6 to 8 weeks. Each patient must also have been treated with at least two courses of electroconvulsive therapy (ECT), one of which must have utilized a bilateral electrode placement.
All patients go through a complex entry procedure that takes at least 3 to 6 months to complete because of the logistics of arranging all the required acceptance and competence adjudication interviews. As of July 2005, all patients screened for surgery are advised about the option of Deep Brain Stimulation, which will likely become an approved intervention once the initial studies have been replicated.
5,6 Once accepted, the patient undergoes a preoperative work-up consisting of a neurological examination, neuropsychological testing, MR imaging, SPECT scanning, and the completion of additional assessment instruments, including the Beck Depression Inventory,
7 the Geriatric Depression Scale,
8 and the Global Assessment of Functioning.
9Postoperatively, the patient is maintained on the same medication as preoperatively, with no changes, for at least 6 months. Thereafter, medications are gradually withdrawn as tolerated or adjusted as needed by patients’ treating community psychiatrists. Patients are seen in follow-up at 2 months, 6 months, 18 months, 2 years, and, logistics permitting, annually, biennially, or triennially, thereafter by TAH, with the intention that all patients will be followed for 10 years. At each follow-up, appropriate rating scales are completed. Neuropsychological testing is repeated at 2 months and at 1 year, with the option of repeat testing at 2 years if impairments are demonstrated at 1 year. The neuropsychological and behavioral domains and the tests utilized to probe these domains are listed in
Table 3. The comparison data for both the 2-month and 12-month testing are the findings of the pre-surgical test performance. A change (either improved or worse) in any given neuropsychological domain is identified if there is a difference of 2 or more scaled-score points between pre-surgical and post-surgical test performance. A change (either improved or worse) in behavioral domains is identified if there is a difference of 10-or-more T-score points between pre-surgical and post-surgical self-/other rating.
MRI is repeated at 2 months and at 1 year. Outcome is assessed with the Global Clinical Categories of Bridges and Bartlett
10 (
Table 4).
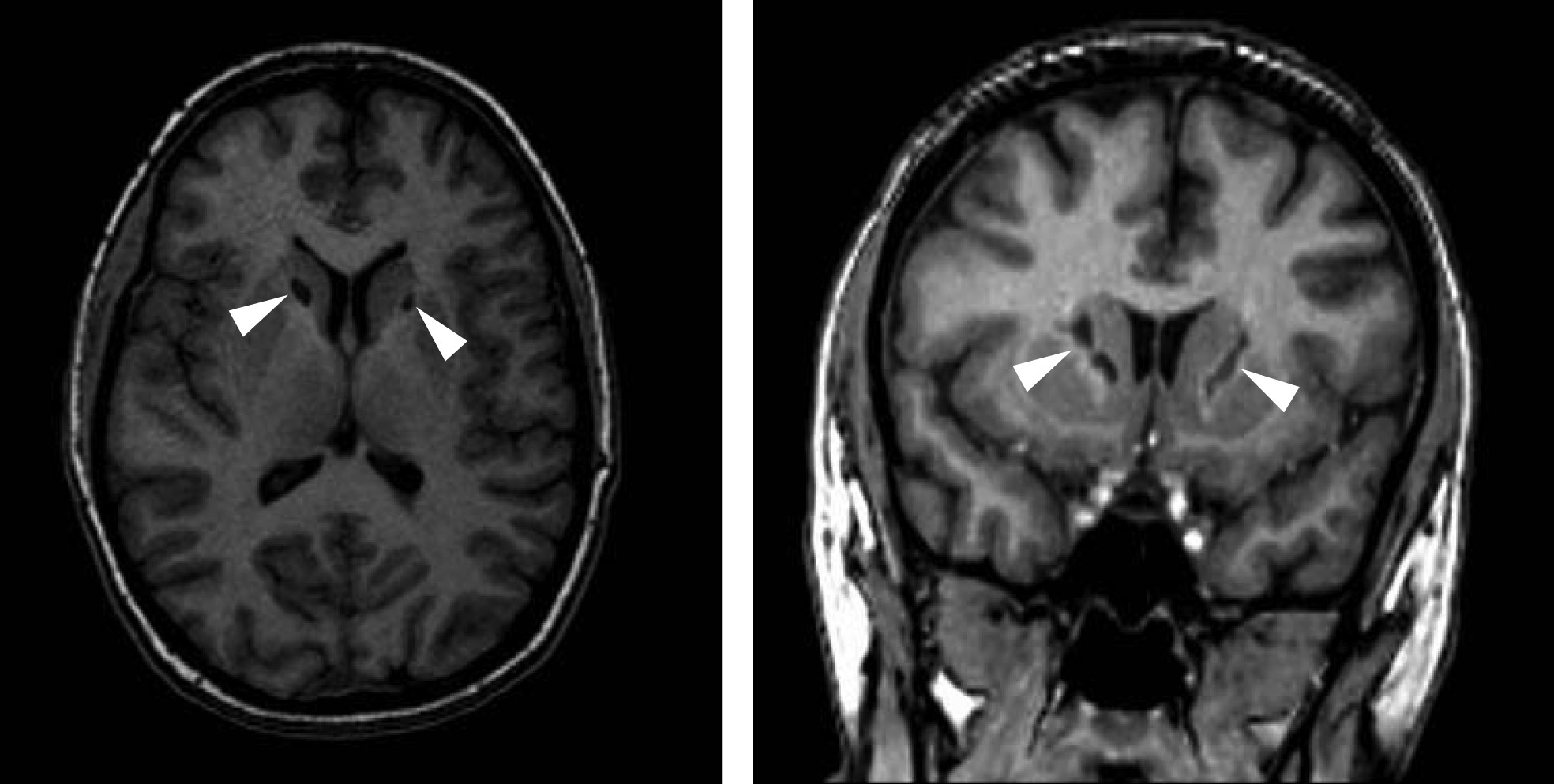
Bilateral anterior capsulotomy is done by stereotactic surgery. The procedure has been previously described.
11,12 Bilateral radiofrequency lesions are produced in the anterior limb of the internal capsule (
Figure 1). The mean diameters of the resultant ellipsoid lesion measure 4.8 mm (range: 4–6) × 4.4 mm (range: 2–7) × 14.2 mm (range: 11–16) on the left and 5.8 mm (range: 4–8) × 5.1mm (range: 3–8) × 14.8 mm (range: 13–16) on the right.
Results
The demographics, BDI, GAF, and GCC scores of seven patients are summarized in
Table 5. Severity of depression was categorized, based on the BDI and GDS score (
Table 6).
13 All patients had been experiencing their current depressive episode for at least 6 years (mean: 8; range: 6–10 years). Three patients (#2, #6, and #7) had had an episode of hypomania in the past. One patient (#3) had her first-ever hypomanic episode, which was possibly provoked by fluoxetine, in the fifth post-operative year. Thus, three patients had underlying major depressive disorder, and four had underlying bipolar II disorder.
Patient #5 is not included in the detailed analysis and comparison. He developed postoperative akinetic mutism, from which he improved after 1 month. His course was then confounded by the emergence of dementia with parkinsonism, which precluded obtaining reliable follow-up data about his depression or his subjective state because of his failing cognitive-intellectual capacities. He died 2 years post-surgery from renal failure. At autopsy, he was found to have extensive arteriolosclerosis secondary to his 40-year history of hypertension and responsible for his development of vascular dementia with parkinsonism.
14Six of the remaining seven patients are improved, as compared with their condition before surgery, and are conservatively classified as GCC III-or-better. Patient #4 is classified as GCC-V because of fatigue that was worse post-surgery than pre-surgery. However, with the exception of reactive depression for several weeks in Year 3 in response to marital distress and again in Years 5 and 6 in response to separation, her dysphoria related to depression, anxiety, and suicidal ideation have been, by her own account, meaningfully attenuated by surgery. All patients, including Patient #4, had an improvement in functioning captured in a rise in GAF scores. All patients are living independently in the community. Compared with pre-surgical levels, only Patient #8 has needed hospitalization because of worsened depression. She required a 2.5-week hospitalization, during which she was diagnosed with and treated for new-onset hypothyroidism.
Preoperatively, all patients were classified as having severe depression by BDI (≥30) and GDS scores (≥20). All seven patients, including Patient #4, demonstrated lessening of depression-severity during the course of follow-up (
Table 5). At 24 to 36 months, where follow-up data are available for all patients, BDI and GDS scores demonstrate that 5 (72%) of 7 patients’ depression had been reduced below moderate-to-severe in intensity. Four patients (57%) were either not-depressed or mildly depressed; one was mildly-to-moderately depressed; and one was moderately-to-severely depressed; and only one remained severely depressed (
Table 5). Using the criterion of a 50%-or-greater reduction in BDI score as a measure of response, four of the eight patients (50%) were Responders at 24-to-36 months post-BAC. This outcome analysis includes the patient with vascular dementia and parkinsonism.
Complications are summarized in
Table 7. Six patients had neuropsychological tests administered before surgery and at 2 months and 12 months post-surgery. One patient (#7) had her second round of neuropsychological testing delayed and done at 24 months because of the logistics of arranging testing in Vancouver. At 2 months post-BAC, the vast majority of neuropsychological domains were either unchanged or improved. The more important long-term neuropsychological outcomes showed a similar pattern. Patient #3 had a significant decline in visuoconstruction. Her visual memory demonstrated a nonsignificant deterioration, but had already been testing in the impaired range before the surgery. Two patients demonstrated a deterioration in semantic fluency. The combination of Attention, Mental Speed, and Executive Functioning domains that are at risk were only compromised in one patient (#6). She also demonstrated a decline in Recent Verbal Memory. Review of her BAC lesions showed no difference in placement or lesion volumes. She was, however, the oldest patient (57 years), raising the possibility that age may constitute a vulnerability factor for neuropsychological compromise. One other patient showed an isolated deficit, in Problem-Solving, at 12 months.
Long-term frontal psychobehavioral changes were only present in Patient #4. At 12 months, but not at 2 months, both she and her family endorsed executive problems, whereas her family, but not herself, identified apathy. These delayed psychobehavioral disturbances were attributable to the confounding effects of her fatigue, as her measured executive functions at 2 and 12 months were unchanged or improved.
Discussion
Since 2000, eight individuals with severe depressive illness of at least 6 years’ duration have undergone BAC. All of them have been followed for at least 24 months. All patients experienced relief, to some degree, from their previously-unremitting depressive illness. In four patients, depression was either completely remitted or persisted in a mild form. The most striking single benefit from BAC was the reduction or abolition of suicidal ideation, an effect experienced by all patients. Suicidal ideation resolved within the first 1-to-2 weeks after surgery in four patients, reported as the acute effects of surgery began to subside. In Patient #4, suicidal ideation abated at 2 months post-surgery, whereas, in Patients #1 and #6, the loss of suicidal ideation was delayed until 6 months post-surgery. The resolution of suicidal ideation has been explored with patients in the immediate post-operative period and at their follow-up assessments. Absent or abated suicidal ideation has not been due to an inability to formulate suicidal ideation because of blunted cognitive capacities. Patients were all clear-thinking when assessed and were fully aware of their predicaments and their choices. They explained that self-injurious ideation simply no longer surfaced as a problem-solving strategy to deal with the unbearable and unrelenting subjective distress of depression. Abated suicidal ideation thus reflected a reduction in sadness: a “tristolytic” effect (tristis: sadness; lysis: destruction of) and has been the best single phenomenological marker of improvement post-BAC. Attenuation or abolition of suicidal ideation has remained a robust effect over the course of follow-up. When present, suicidal ideation has been minor relative to pre-BAC intensity, and either reactive to significant psychosocial stress or, in the case of two patients, returning with pre-BAC severity when they relapsed into depression.
The time-to-optimal remission of depression post-BAC varied between 2 and 9 months. The gradual lessening of the depression syndrome over 2-to-9 months contrasts to the relatively rapid tristolysis and abated suicidal ideation in most patients. Tristolysis, which was immediate in half of the patients, may be accounted for on the basis of a biological process acutely interrupted by surgery. Other biological and psychological mechanisms likely account for the remission of the depression syndrome. Depressive illness is often accompanied by demoralization, which shows phenomenology that overlaps with depression. Demoralization is, at its core, a traumatized self, filled with a sense of personal failure and ineffectiveness, the result of frustration at persisting and intrusive symptoms, the inability to find relief, the loss of hope that things will ever be different, and the loneliness of the experience.
15,16 After BAC, the demoralization reverses because the patient has had symptomatic relief from the previously-unrelenting internal distress of depression. Anterograde and retrograde transneuronal degeneration provides an alternative or co-occurring biological explanation that may account for the improvement over time. In this process, neurons that are connected synaptically to form specific circuits undergo sequential cell-death due to loss of neurotrophic support, excitotoxic cell-death, or other factors.
17–20 This is a time-dependent process and may ultimately lead to loss of the neuronal circuitry that is critical for sustaining the depression syndrome.
Only one patient (Patient #3) has been able to discontinue psychiatric medications. All other patients have required medication. Patient #2 tried to discontinue her medications at 9 months, but relapsed into a mild depression 2 months later. She has remained on medications ever since. In two patients, residual depression at 18 months and 36 months post-BAC clearly improved when antidepressants were added to mood-stabilizers. The need to continue antidepressant medications indicates that BAC, despite its benefits, does not abolish the psychobiological disturbance that underlies the depressive illness.
The emotional effect of BAC appears to have selectively attenuated sadness associated with depressive illness. BAC has not prevented three patients from experiencing bereavement reactions in response to important deaths. BAC has also not interfered with the capacity to experience other emotions, such as pleasure, anxiety, and anger. This pattern of preserved reactive sadness suggests that BAC selectively interferes with sadness linked to the putative and primary limbic psychobiological disturbance of the depressive syndrome, a bottom-up effect, but not reactive sadness in response to psychosocial loss, a top-down effect.
21Our experience with BAC for depression is limited to eight patients, and our results should therefore be interpreted with appropriate caution. Moreover, we are working with the extreme end of the depressive spectrum. These patients’ psychobiology may be very different from most other patients, whose depressive illness responds to treatment. With these caveats in mind, our results to-date are nonetheless equal to or better than those reported for other surgical procedures for depression (
Table 8).
Conclusion
One patient, a 75-year-old man, had a poor outcome. His postoperative course was complicated by progressive dementia and parkinsonism secondary to hypertensive small vessel disease. Because of our experience with this particular patient, BAC will no longer be offered to anyone over 60 years of age because of the risk of initially undetectable but later emergent neuropathologies associated with aging that will result in an adverse outcome when combined with BAC. For the remaining seven patients, BAC has been life-saving and has provided sustained benefit, with alleviation of depression and suicidal ideation and an improvement in quality of life that, for some, has been dramatic. All patients, including the 75-year-old patient, had relief of intense suicidal ideation that had been a daily part of their mental state for the preceding several years.
In carefully selected and screened patients, BAC is a treatment option for severe, intractable, and life-threatening depressive illness. For patients under 60 years of age, BAC has had few significant persistent side effects. Fatigue is the one exception, seen in one patient. Long-term neuropsychological capacities and frontal psychobehavioral functioning are mostly unaffected or improved. Most, if not all patients will still need antidepressant medication. In our small cohort, benefit was often already present in the first few days after surgery. BAC appeared to rapidly reduce the intensity of subjective distress, an effect that was best reflected in the remission of suicidal ideation. Improvement continued over the subsequent 2 to 9 months. This current report is preliminary and provides encouraging data about the effectiveness and safety of BAC in patients under 60 years of age.
Acknowledgments
The authors thank Justice Barbara Fisher, who served on the screening committee from its inception in 1998 until her appointment to the Supreme Court of British Columbia in November 2004.
None of the authors have any financial or conflict-of-interest disclosures.