To the Editor: Punding is characterized by a peculiar stereotyped behavior, with complex, excessive, non–goal-oriented, repetitive patterns of engagement in various tasks. Even though often described as related to dopaminergic dysregulation neurotransmission, especially in parkinsonian patients, punding may be more complex than just dopaminergic stimulation, involving the brainstem serotonergic system and other neurotransmitters, thus explaining its genesis in seemingly unrelated neuropsychiatric disorders.
1,2 We describe, for the first time, an association between punding manifestations appearing as initial symptoms in a dementia picture. It was present in an elderly patient with cognitive deficit characterized especially by language and memory impairment, with adequate metabolic and nutritional profile, and with neuroimaging studies compatible with primary dementias. Although uncommon, punding provides many challenges for patients and physicians. Physicians, thus, should be aware of its presentations and implications, leading to correct diagnosis and treatment.
Punding is characterized by a peculiar stereotyped behavior with complex, excessive, non–goal-oriented, repetitive patterns of engagement in various tasks, first described in amphetamine and cocaine addicts in California and Denmark. Classic examples of punding are manipulation of technical equipment; handling, examining, or sorting through common objects; grooming; hoarding; or starting extended monologues devoid of content.
1,3,4The behaviors may be linked to increased dopaminergic effect, since amphetamines, cocaine, and levodopa share a presynaptic mechanism. Selegiline might also play a role, enhancing the action of levodopa.
1,2,4The prevalence reported of such finding was 26% among methylphenidate users and 8% among cocaine addicts.
1,3 Nowadays, it is usually associated with antiparkinsonian drugs, in a prevalence ranging from 1% to 14% among users.
2Predisposing factors for punding are high-dose levodopa (higher than 800 mg/day) and dopamine agonists as monotherapy or in combination.
3As far as we know, there is no reference in current literature linking punding with dementia, either in presentation or as complication or development. We describe here what we believe to be a case of punding being manifested as part of the first symptoms in an early-onset form of dementia.
Such clinical characterization is important to raise the possibility that such cases are underdiagnosed and that pudding might be a much more prevalent clinical finding than previously assumed.
Case Description
We describe the case of a 60-year-old Brazilian man. He had been a science teacher in high School when, 6 years ago, he presented with progressive memory failure and hypobulia, after retirement. He was single and had lived with a few siblings.
Relatives report that he became gradually more quiet and isolated, but initially without depressed mood.
He was in treatment for hypertension with loop diuretics and angiotensin receptor-blockers, and he had smoked regular cigarettes for 30 years, stopping 10 years ago.
The behaviors compatible with punding were initially noticed when, later on, he started to copy his own science books into a blank notebook, repeatedly and meaninglessly, occupying sometimes the whole day in this task, only stopping when strongly persuaded by his relatives. Such behavior was intermittent and appeared abruptly. Soon after that, aggressive behavior and motor agitation were also added to the general symptom list.
There were no other neurological deficits and no signs of tremor, rigidity, or bradykinesia. He denied seizures, headache, or sleep disorders. A difficult interaction with the patient was constant during the clinical examination, and his mood was irritable.
The initial hypothesis was that a depressive episode was leading to major cognitive impairment (pseudodementia), but a therapeutic proof with paroxetine failed to decrease depressive symptoms, guiding the clinical investigation more toward an early-onset form of neurodegenerative disorder, especially an early-onset Alzheimer´s disease (EOAD).
Mini-Mental State revealed a score of 3 out of 30, characterizing severe cognitive impairment. The laboratory screening for dementia was unremarkable. He was then evaluated by the Psychiatry and Neurology team and started on drugs to treat a potential EOAD, besides insomnia and psychomotor agitation (rivastigmine, trazodone, promethazine, and chlorpromazine). His follow-up showed partial control of the symptoms, without resolution. Chlorpromazine and promethazine were discontinued soon after. Trazodone and rivastigmine were maintained.
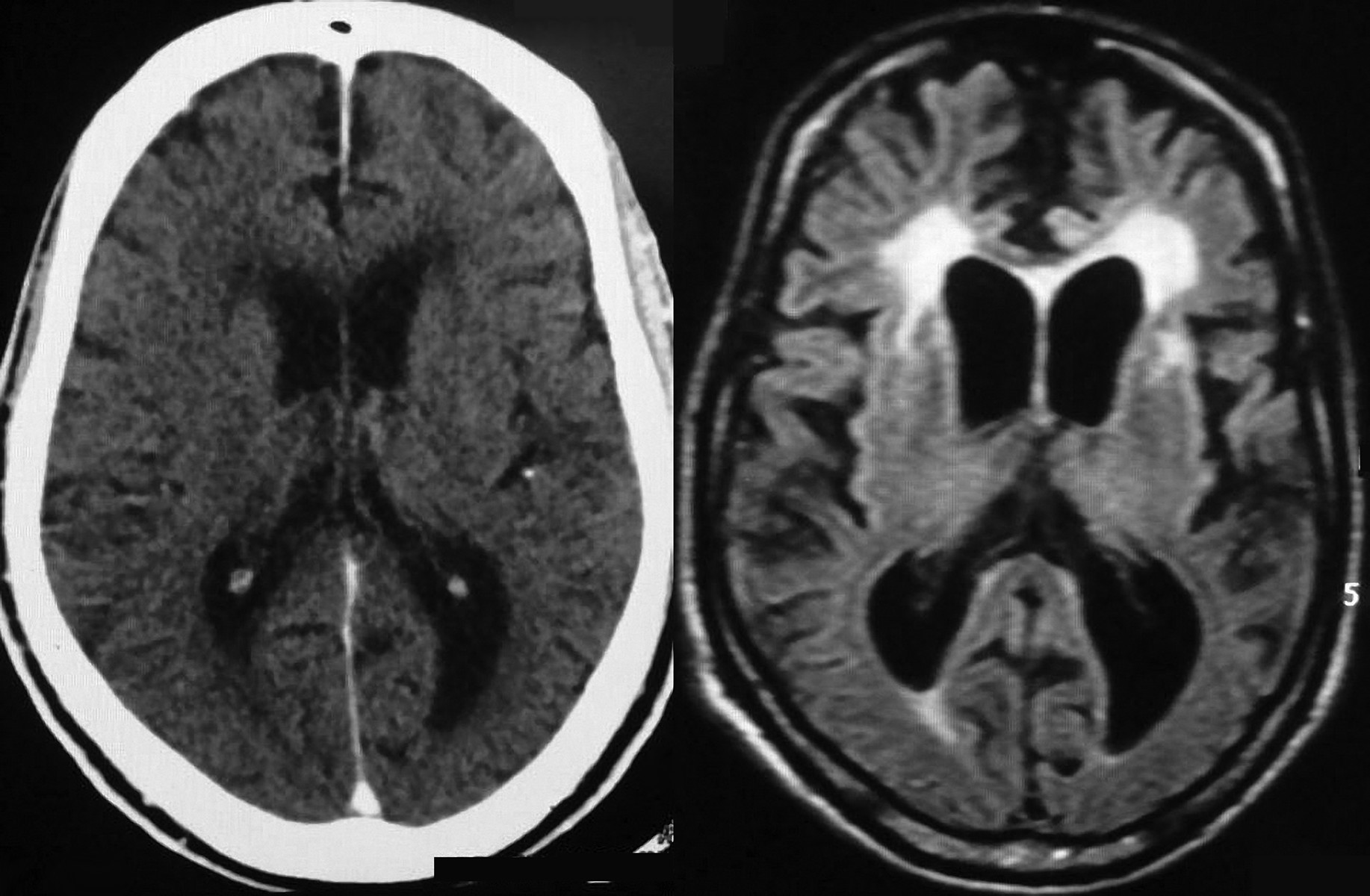
Initial imaging investigation with computerized tomography in 2007 showed global volumetric reduction of brain with deep sulci, fissures, and lateral ventricle dilation. A nuclear magnetic resonance (NMR) done in 2010 showed advanced signs of cortical atrophy and microangiopathy in diffuse white matter, with both hippocampi presenting with quite reduced volumes (see
Figure 1).
The nosologic retrospective definition, although hard to achieve in this particular case, was regarded as a dementia profile. The lack of biopsy finding to determine the specific cause led us to consider as differential diagnosis Alzheimer disease, frontotemporal dementia, vascular dementia, and associations of different types of dementia.
The patient is now 65 years old, and we still follow up on his case in our general hospital. The general cognitive decline is progressing.
Discussion
Punding includes excessive humming or singing, inordinate writing, paper shuffling, blogging/journaling, doodling, painting, walkabouts, and reciting long, meaningless soliloquies without an audience.
1–5In our report, we believe we are facing a new frontier toward the comprehension of the physiopathology of this symptom, now in dementia. It was present in an elderly patient with cognitive deficit characterized especially by language and memory impairment, with adequate metabolic and nutritional profile and neuroimaging studies compatible with primary dementias.
Even though often described as related to dopaminergic dysregulation neurotransmission, especially in parkinsonian patients, punding may be more complex than just dopaminergic stimulation, involving the brainstem serotonergic system and other neurotransmitters, thus explaining its genesis in seemingly unrelated neuropsychiatric disorders.
1,2Once punding is diagnosed, specific treatment strategies could be adopted. A number of parkinsonism cases have been treated successfully through a change or reduction in medication, although this requires careful balance between the control of side effects and worsening motor functions. Classic neuroleptics must be avoided to preserve motor function.
5Although uncommon, punding provides many challenges for patients and physicians. Physicians should be aware of the disorder because the spectrum of normal-to-abnormal behavior is unclear, and patient insight is impaired, reducing the likelihood of spontaneous self-reporting. Commonly, the symptom is only triggered at home, and its reporting depends on observation and cooperation of close relatives.
1,5Conclusions
To our knowledge, our report represents the first association between punding and dementia disorders to-date, giving light into new insights about physiopathology, clinical manifestations, and treatment of this symptom.
We highlight the need for increasing awareness about punding for general clinicians, neurologists, and psychiatrists, who deal more often with such patients in a daily basis.
The subtlety of this theme reinforces the need of better concepts, objective scale evaluations, and further studies in the purpose of better understanding this interesting symptom.