To the Editor: Clozapine is rarely associated with venous thromboembolic phenomena. The reason for the association between clozapine and thromboembolism is largely unknown. Here we report a rare case of pulmonary thromboembolism (PTE) in a middle-aged man who was admitted to the cardiac intensive care unit with a history of sudden-onset breathlessness and tightness in the chest. He had been on treatment for resistant schizophrenia with clozapine for the last 8 months. A thorough history did not reveal any possible risk factors for PTE.
A possible association between venous thromboembolism (VTE) and the use of antipsychotic agents was first suggested in the 1950s after the introduction of phenothiazines.
1 To-date, information on the risk of VTE is almost exclusively limited to clozapine.
2–5Clozapine is a tricyclic dibenzodiazepine that is efficacious in the management of treatment-resistant schizophrenia and is used when two treatment attempts with second-generation antipsychotics have failed.
6,7 The use of clozapine in clinical practice is restricted by its side effects and the need for frequent blood monitoring.
8 However, schizophrenia patients with persistent suicidal behavior, violence, or comorbid substance abuse may benefit from clozapine.
9,10Data from the Swedish Adverse Reaction Advisory Committee (SADRAC) suggest that use of clozapine is associated with venous thromboembolic complications.
4 Twelve cases of thromboembolic complications that occurred during clozapine therapy were reported to SADRAC between April 1, 1989, and March 1, 2000. Six cases were of pulmonary embolism, and the remaining cases were of venous thrombosis. Among these 12 cases, 77% of affected patients were men. In 67% of the patients, symptoms occurred within the first 3 months of clozapine therapy. The mean age was 38 years. The mean clozapine dose was 277 mg/day, which was slightly less than the defined dose of 300 mg/day, and therefore, authors concluded that the reaction was not dose-dependent. Known risk factors for thromboembolic disease are many, and include genetic factors, substance abuse, obesity, recent major surgery, immobilization, multiple traumas, hip or leg fracture, congestive cardiac failure, myocardial infarction, stroke, pregnancy, progesterone, and others.
11,12Case Report
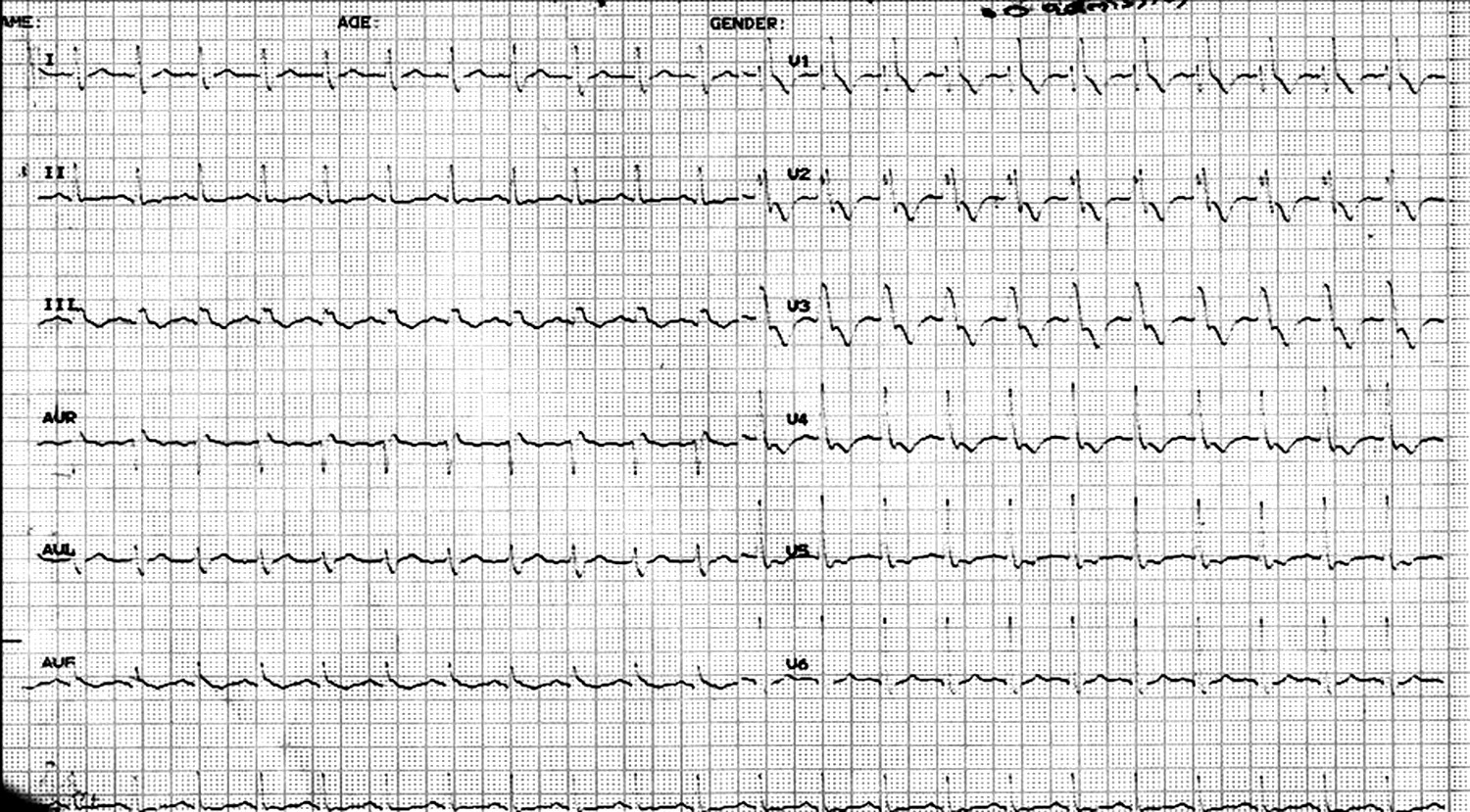
A 39-year-old man who was suffering from mental illness, on clozapine therapy, was admitted to the cardiac intensive care unit with a history of sudden-onset breathlessness and tightness in the chest of 4 hours’ duration. His ECG showed tachycardia, right bundle branch block (RBBB), and right axis deviation (
Figure 1). Chest X-ray PA view did not reveal any abnormality. 2-D echocardiography showed dilation of right and left atria and dilated pulmonary artery with severe pulmonary arterial hypertension. However, the ventricles were healthy and did not reveal any clot formation within them. His arterial blood gas analysis showed the following values: pH: 7.472; PCO
2: 33 mmHg; PaO
2: 72.6 mmHg; Bicarbonate: 25.3 mmol/lit, and O
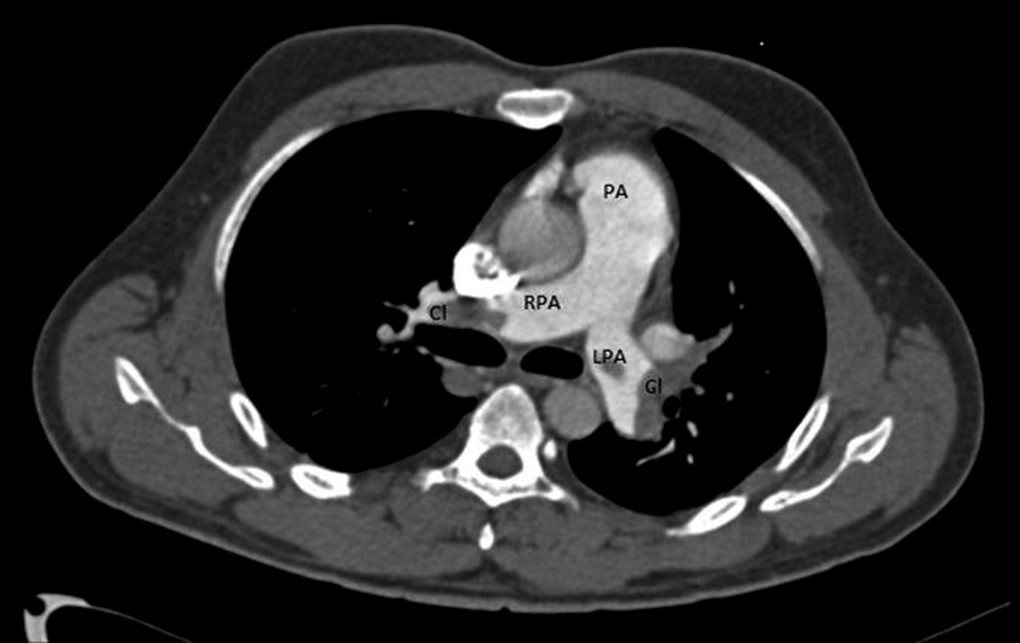
2 saturation: 94%. CT scan of thorax revealed bilateral pulmonary thromboembolism involving main pulmonary arteries, lobar, and segmental arteries (
Figure 2). Color Doppler studies of lower limbs showed normal arterial and venous blood flow on both sides. Prothrombin time was 12.9 sec; INR was 10.5 sec, with control being 10.5 sec. Anticardiolipin antibody titres IgG, Ig A, and IgM were within normal limits. Lupus anticoagulant screening was healthy. Screening for clotting factors and clozapine levels were not available. His blood picture showed normal RBC, WBC, and platelet counts. He was thrombolysed using streptokinase injection, maintained on heparin infusion, and later changed to low molecular-weight heparin injections and oral warfarin. There was no history suggestive of either similar complaints in the past or familial coagulopathies. He was non-diabetic, non-hypertensive, and was not a nicotine user. He was moderately built, had a body mass index (BMI) of 21 kg/m
2, and did not have history of having undergone any surgery recently.
A detailed interview revealed that he had been suffering from mental illness for the past 22 years. He initially complained that three of his neighbors were commenting on his actions, as he could hear their voices and felt that they were plotting against him. After about a month, he suddenly disappeared from his house and was found after 6 months in a place that was 250 km away from his hometown. When found, he was shabbily dressed, had grown a long beard, and had not maintained his personal hygiene, but he was able to identify his relatives immediately. He neither explained why he had suddenly absconded nor revealed any other details that might have happened during this period. Psychiatric help was sought; he was diagnosed with schizophrenia; and was put on trifluoperazine (TFP) 20 mg per day, along with trihexyphenedyl (THP) 4 mg per day, in divided doses. Routine blood tests were healthy, and EEG revealed no epileptic activity. Since there was minimal response, four ECTs were given, and the dose of TFP was increased to 30 mg per day. He showed partial improvement for 6 months and discontinued treatment later for about 2 years. He was taken to a psychiatrist again because he had relapsed. He received several antipsychotics, including trifluoperazine, risperidone, and olanzapine adequately at different times along with ECTs in between. He had waxing and waning of symptoms and never returned to his premorbid level of functioning. He was diagnosed with treatment-resistant schizophrenia. For 8 months, he was receiving clozapine 150 mg at night. With this treatment, his symptoms disappeared by 80%, and he was functioning adequately. He had no family history of psychiatric illness. His birth and childhood histories were not significant.
After admission, clozapine was discontinued immediately, and he was switched over to haloperidol 20 mg in divided doses. The patient recovered from PTE and was discharged from the cardiac unit on the 10th day. He has been coming to the psychiatry unit for regular follow-up for 6 months, and he is found to be well-maintained on haloperidol.
Discussion
The exact mechanism by which clozapine causes pulmonary embolism is poorly understood, but various hypotheses have been put forward to explain this, as mentioned subsequently. Clozapine has a high affinity for serotonin receptor 2A, which accelerates platelet aggregation and leads to thrombus formation. Clozapine is believed to elevate lupus coagulant levels and anticardiolipin antibody titers, which increase the risk of developing thrombosis. Clozapine therapy leads to dyslipidemia, insulin resistance, and obesity, thus causing metabolic syndrome, which may be associated with thromboembolic phenomenon.
13Despite the uncertain mechanisms of clozapine, several cases of venous thromboembolism have been reported. Hagg et al.,
4 in 2000, reported six cases of pulmonary embolism and six cases of venous thrombosis associated with clozapine use. Many spontaneous reports were submitted to the U.S. Food and Drug Administration’s (FDA’s) Adverse Event Reporting System database between February 1990 and December 1999.
14 The database mentioned 83 unduplicated reports of pulmonary embolism and 16 reports of deep vein thrombosis. There have been many cases of thromboembolism reported with varying doses and durations of clozapine therapy.
Table 1 shows case reports mentioning doses and durations of clozapine therapy.
In the case reported here, pulmonary embolism occurred in a physically healthy, middle-aged man who was on clozapine for 8 months. Risk factors
11,12 like substance abuse, obesity, recent major surgery, immobilization, multiple traumas, hip or leg fracture, congestive cardiac failure, myocardial infarction, stroke, and family history of coagulopathies were not present in this case. Most of the cases mentioned in the literature and the present one reveal that the pulmonary embolism is diagnosed during clozapine initiation, as well as during maintenance, suggesting that the embolic phenomenon may occur anytime during clozapine therapy.
15–21 In addition to this, the mean clozapine dose used in the case studies reported here was very much within the defined dose of 300 mg per day, except in one study by Maynes, where the dose was 400 mg per day.
16 This probably suggests that the embolic phenomenon was not dose-dependent.
Conclusion
In our case, clozapine was the only cause of pulmonary embolism. Further studies are needed for evaluation of the possible mechanism and risk factors for this potentially fatal adverse effect. This case is presented to alert healthcare providers of this rare adverse effect, to call attention to the risks associated with thromboembolism, and to enable prompt recognition of symptoms so that morbidity and mortality can be decreased in patients on clozapine therapy.