Case Report
A 70-year-old, right-handed woman with simple hypercholesterolemia and no personal or family history of psychiatric care visited her primary physician because of depressive and anxious symptoms, which were unsuccessfully treated with escitalopram (10 mg). Two months later, she came to the emergency room with selective mutism, incoherent responses, strange behaviors, and high anxiety. She repeatedly stated that she was a widow and that her children had disappeared and been replaced by impostors (although her husband and adult children were with her during this conversation).
The patient was admitted to the acute care mental health unit and underwent diagnostic tests (biochemistry, viral serology, ultrasonography, and urine toxicology). There were no pathologic findings.
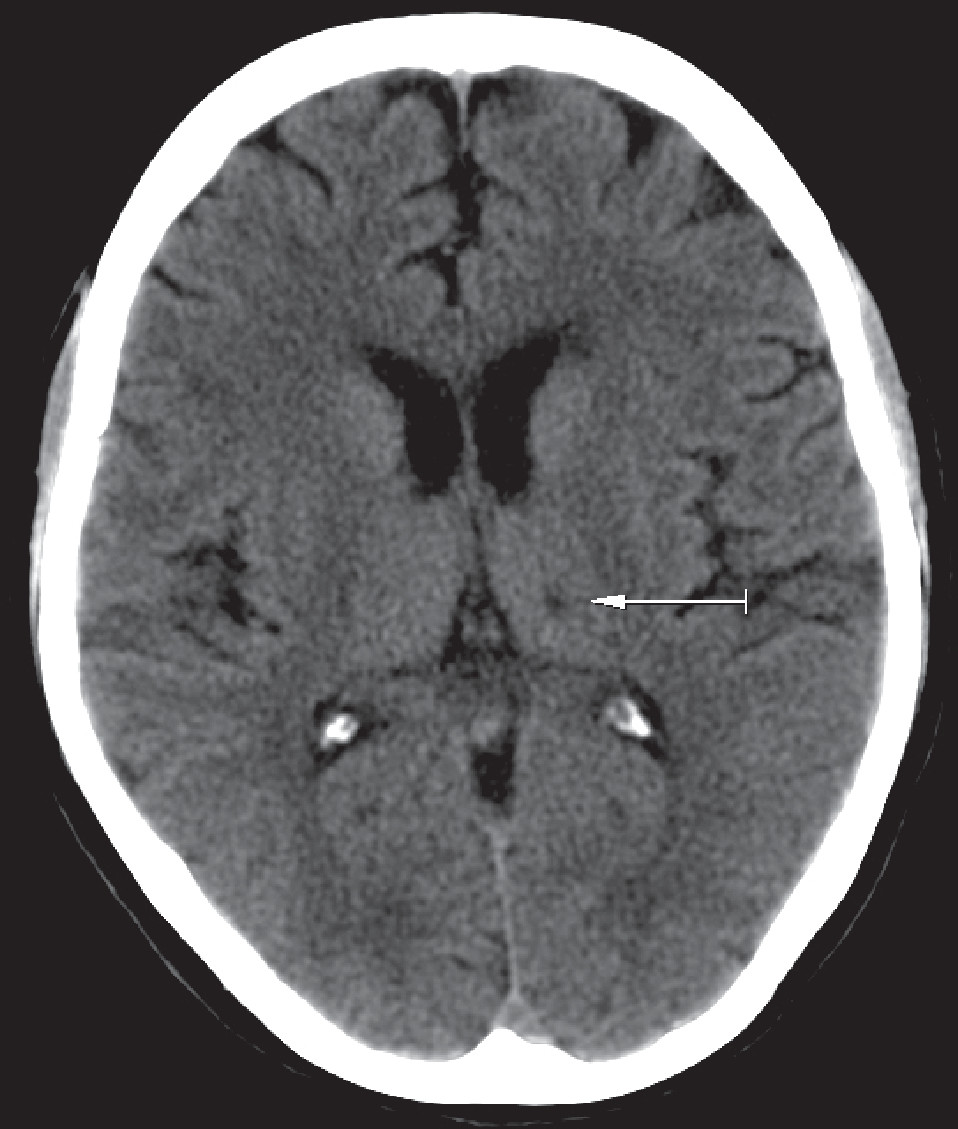
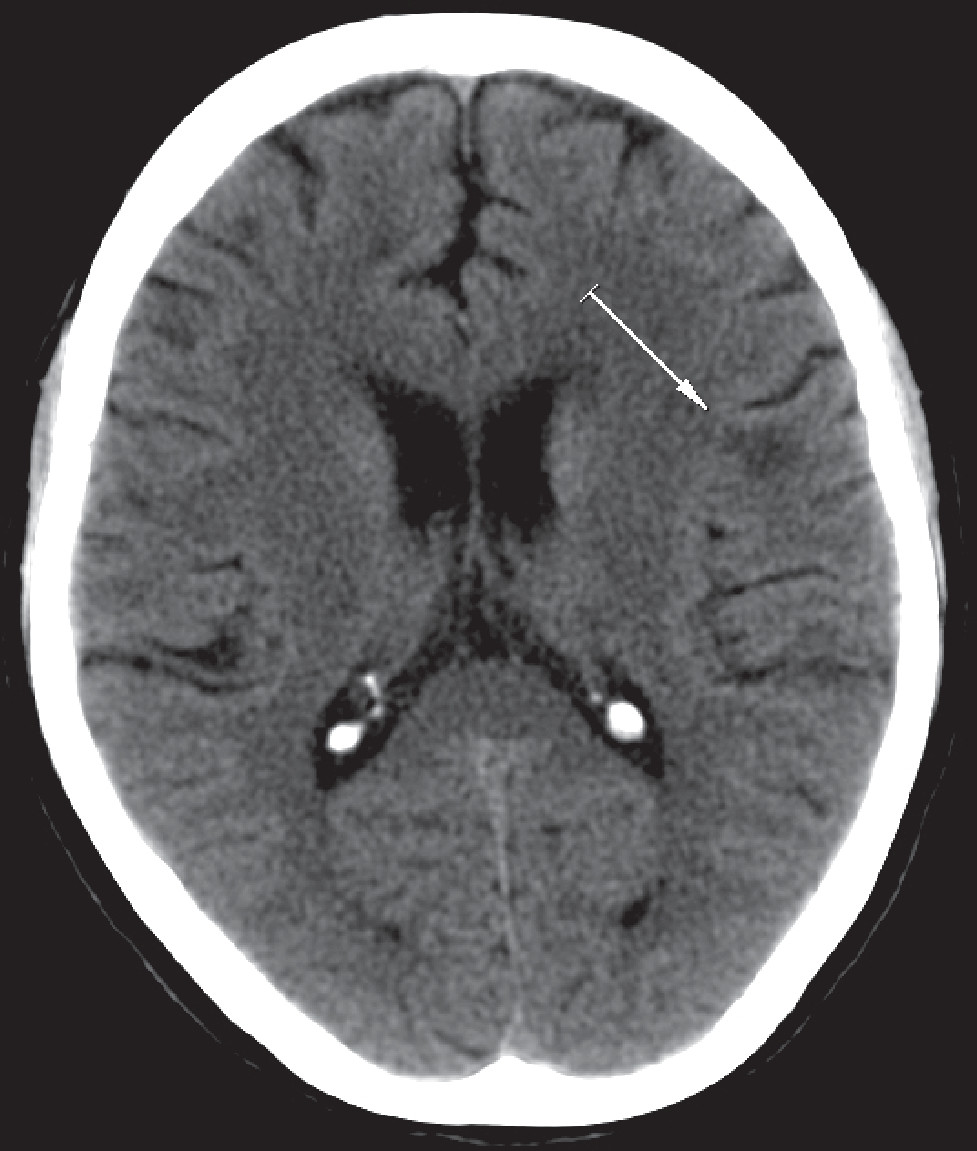
Cranial CT revealed discrete cortical atrophy, a small abnormal lacunar image in the left thalamus (
Figure 1), and left frontal subcortical hypodensity (
Figure 2). The observed cerebral damage was compatible with a cerebrovascular accident within the last 3–6 months, in accordance with the onset of the clinical presentation described.
Structural nuclear magnetic resonance showed pathologic areas in T2-weighted and fluid attenuated inversion recovery sequences in the left thalamus. Cranial SPECT indicated a hypofunction in the left thalamic region.
The patient responded favorably to antipsychotic (risperidone, 3 mg/day), antidepressant (sertraline, 100 mg/day), and anxiolytic (clonazepam, 6 mg/day) therapy. On day 5, decreased anxiety was observed, along with the disappearance of the patient’s hallucinations and insomnia. On day 10, the misidentification syndrome began to show partial improvement, and the patient began to accept her family members, which continued after discharge. In outpatient care, a neuropsychology examination was done; minor verbal and executive amnesia (at the planning level) was observed, compatible with slight cognitive deterioration.
Discussion
There have been many theories about the relationship between Capgras syndrome and an impact on the frontal, temporal, and right limbic regions. An exclusive relationship with cerebral damage to the left hemisphere is less frequently observed and tends to be limited to case studies of patients with Alzheimer’s disease,
1 Lewy body dementia,
2 or traumatic hemorrhagic lesions.
3Taking into consideration the lack of structural lesions and the theories based on the principles of cerebral laterality and disconnection, which relate right hemisphere neurological damage to preservation of the left hemisphere
4 to Capgras syndrome, cranial SPECT was used to discard the possibility of functional impact in this hemisphere. The absence of structural lesions from a functional impact in the right hemisphere and a neuropsychology exam compatible with slight cognitive deterioration led us to discard a right hemisphere effect that would be in accordance with cerebral laterality theories or with the explanation of the pattern within a dementia process. The clinical pattern could be partially explained by a disconnection between the frontal lobe and the temporal and limbic regions,
5 although the psychopathologic mechanisms have not been fully elucidated.