Huntington’s disease (HD) is a genetic neurodegenerative disease characterized by motor disturbance, cognitive decline, and psychiatric symptoms. HD is caused by an expansion of cytosine-adenine-guanine (CAG) repeats in the
Htt gene on the short arm of chromosome 4, resulting in production of the mutant protein huntingtin. The exact pathophysiological processes that occur in HD are not yet fully understood, although different mechanisms have been suggested.
1 The onset of the disease usually occurs in midadulthood, with considerable variation in clinical presentation. The disease is autosomal dominant, which means that those who carry the gene present a 50% risk of passing the disease to any of their children. The duration of the disease varies but is, on average, 20 years from the onset of motor signs to death.
2 As yet, no cure has been identified for HD, although treatments to manage different symptoms may help reduce distress and improve QoL.
So far, the clinical diagnosis of HD is dependent on the motor signs of the disease, involving problems with voluntary and involuntary movements. However, cognitive and psychiatric symptoms may be present many years before the onset of motor problems.
3–5 The psychiatric component of the disease can involve a number of different complaints including depression, irritability, anxiety, apathy, obsessive-compulsive behaviors (OCBs), and psychosis.
6,7 Although motor and cognitive symptoms worsen with time, psychiatric symptoms appear to have a more variable course,
8 with the exception of apathy, which is more prevalent in advanced disease stages.
A systematic review of psychopathology in HD identified that the prevalence of anxiety among manifest HD participants was between 34% and 61%, depending on the disease stage and the measure used.
7 Although anxiety symptoms are commonly reported in HD, this topic has received limited attention in the literature, with the exception of OCBs, which have been reported on more frequently.
9 However, it is questionable whether OCBs in HD may be construed as an anxiety condition, as there is evidence that they may be more closely associated with the cognitive changes in HD, particularly executive dysfunction.
10Because there is a lack of information about anxiety in HD, we systematically reviewed the literature on the epidemiology and phenomenology of anxiety in HD and identified areas for future study.
Methods
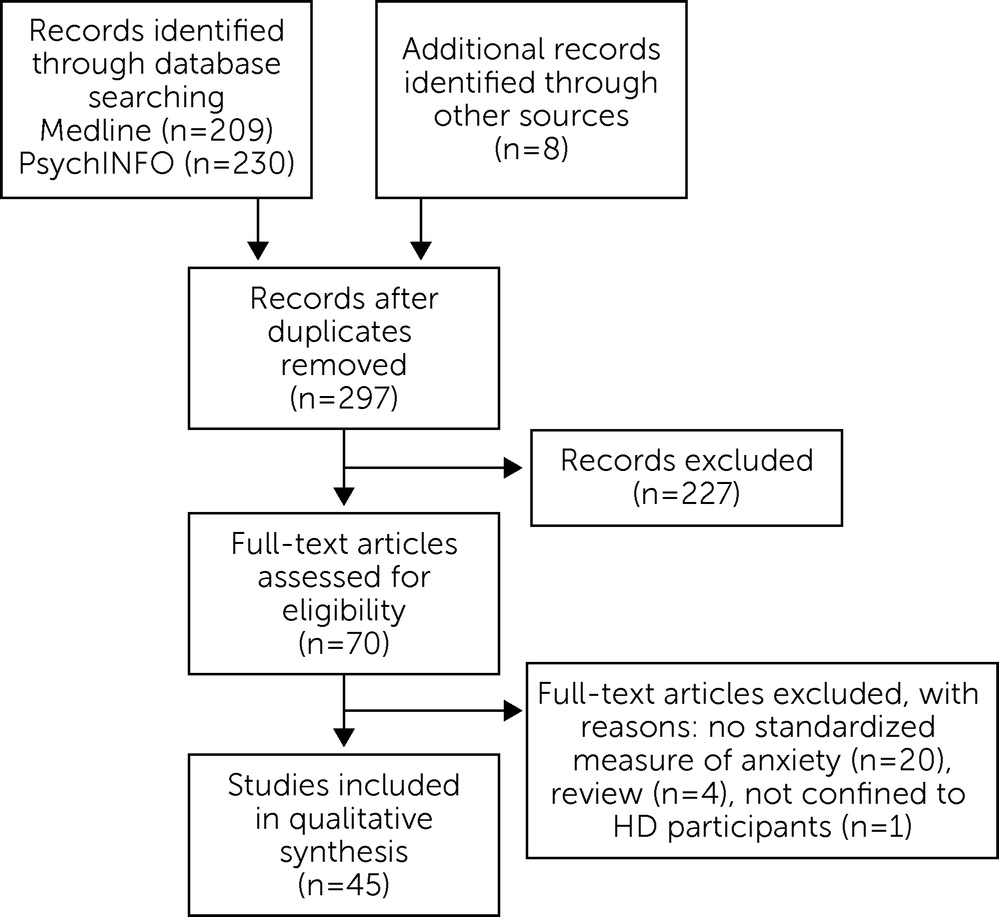
We carried out data searches using PsycINFO and MEDLINE to identify published articles from 1994–2014. The rationale for our exclusion of articles written before 1994 was due to predictive genetic testing only becoming available after the discovery of the HD gene in 1993. Searches were restricted to human studies that were written in English. The following search strings were used in February 2014: “Huntington*” combined with “anxiety*,” “psychiatric,” and “psychological.” The term “depression” was also combined with “Huntington*,” as we were aware that some studies of anxiety in HD are embedded within broader research of depression in HD and that some studies using measures of psychopathology, developed specifically for use within an HD population, combined factors for anxiety and depression.
From the database searches, we retrieved a total of 209 articles from MEDLINE and 230 from PsycINFO. An additional eight articles were identified from reference lists and consultation with researchers in the field. Duplicates were removed, resulting in 297 articles. We then conducted a manual search of titles and abstracts and excluded the following: case studies, conference abstracts, qualitative studies or studies with no standardized measure of anxiety, reviews, dissertation abstracts, juvenile HD studies, and studies not including verified HD expansion carriers (e.g., involving only at-risk or caregivers of HD). We also excluded articles that were confined only to obsessive-compulsive disorder (OCD) because it could be argued that these symptoms are more closely related to the cognitive symptoms of HD, rather than anxiety.
Following this, a total of 70 studies warranted manual full-text searches to assess eligibility. Reasons for article exclusion at this stage were that they did not include a standardized measure of anxiety (N=20), they were review articles (N=4), or the sample included participants with disorders other than HD (N=1). The total number of studies finally included was 45. See
Figure 1 for a summary of the review process.
Discussion
This is the first systematic attempt to review the status of research into anxiety in HD. Although anxiety is frequently reported in HD, none of the articles identified in this review examined anxiety as the central theme of the study, confirming that anxiety is a relatively neglected area of research within HD. Results of all studies in this review revealed a wider range of prevalence (13%−71%) among manifest HD participants, compared with the range reported in a previous review of psychopathology in HD undertaken in 2007.
7 This finding was partly due to one study that examined a cumulative prevalence for 3 years resulting in higher anxiety levels (71%) among manifest HD carriers.
15 Also, since 2007, studies using DSM-IV criteria have been published resulting in lower prevalence rates of anxiety.
Although prevalence studies of premanifest HD expansion carriers showed a lower range of anxiety (0%−15%), this outcome appeared to be the result of nearly all of the studies using tight diagnostic criteria and some studies having very small sample sizes.
28,29,31 When studies of premanifest HD carriers with the largest samples available were compared with the manifest group using a formal diagnosis, there was limited difference in prevalence between the groups. This finding is supported by studies that have compared anxiety across manifest and premanifest HD expansion carriers and have found no difference in symptomology and diagnosis.
4,23,25 These findings would appear to indicate that psychiatric problems precede the development of the motor aspect of the disease,
3,5 although the extent to which anxiety is more prevalent in HD carriers compared with the general (non-HD) population is still unclear. The range of total anxiety diagnoses in the larger studies of HD mutation carriers was 12.5%−16.5% for point prevalence to 12-month prevalence. These results may be compared with rates of the general (non-HD) population, as determined by a systematic review of 41 prevalence studies,
50 where a best estimate of 10.6% was given (with a 95% confidence interval of 7.5%−14.3%) for total anxiety disorders, across a 1-year period. Hence, although anxiety disorders appear to be more prevalent in HD compared with the general population, this cannot be a definitive conclusion without studies involving greater numbers of HD participants. Specific formal anxiety disorders that appear more prevalent in HD are GAD (3.8%−9%) and PD (3.6%−7.7%), with prevalence rates that are higher than in the general population.
50The factors that make comparisons of anxiety prevalence difficult across studies are the different measures used, different disease stages of participants, and rather small sample sizes. Many studies of anxiety in HD have used measures that were designed specifically to assess the range of behavioral symptoms in HD, like the PBA-HD, but have limited items for the assessment of anxiety. Hence, the full range of symptoms associated with anxiety problems may not be captured, along with the different anxiety disorders. Some of the measures used cover a range of anxiety symptoms (e.g., STAI, HADS), but their psychometric properties have not been fully explored for use in HD. DSM criteria may be the gold standard used to assess psychiatric diagnoses,
7 but there may also be limitations due to the co-occurrence of somatic and cognitive problems and reduced insight into HD, particularly in the more advanced stages of the disease.
51 Results from this review would indicate a requirement for more comprehensive measures of anxiety that are both valid and reliable for use within HD.
The results of this review indicate that it is still unclear whether HD expansion carriers experience more anxiety than verified noncarriers with an a priori 50% risk, which is an interesting area of research, as it assists in our understanding of whether the psychosocial factors of being in an HD family and being at risk for HD contribute to the development of anxiety. However, two recent studies with larger sample sizes than previous studies indicated that premanifest carriers reported more anxiety symptoms than noncarriers,
3,4 suggesting that there may be factors specific to having the disease that underlie anxiety in HD. Many noncarriers may be anxious about their future before they have taken the predictive test, but it would appear from the research to date that even when they have received a negative test result, there is no difference in anxiety among those with a positive and negative result up to 5 years after testing.
45 The possibility exists that as HD expansion carriers become closer to the onset of motor symptoms, anxiety increases, but so far the evidence does not support this.
4,30 More research is required with larger sample sizes.
A number of variables have been examined in relationship to anxiety in HD. Anxiety is associated with depression in HD, although this relationship requires further elucidation because frequently both conditions have been examined together as a cluster of symptoms. Studies of temporal patterns of anxiety and depression in the general population have revealed that although there is evidence of a bidirectional relationship, anxiety disorders often predate depression.
52 Importantly, anxiety has been found to have an independent association with suicidal ideation in HD, although it was not found to be a predictor across a 4-year longitudinal study.
43 However, given that suicide is strongly related to depression and that anxiety may be a risk factor for depression, it is crucial that anxiety be identified and treated effectively within this population. Despite limited evidence, anxiety also appears to be related to QoL
34 and aspects of functional ability,
35 which would further confirm that this is an important area to address within HD.
Anxiety is also associated with irritability and agitation. This may be due to a number of different explanations such as anxiety arising in response to interpersonal difficulties created by irritability, that both conditions arise as a result of pathological changes associated with HD, or that anxiety arises from cognitive overload and leads to irritability in a person who lacks social cognition or who is impulsive. It would be useful to explore these relationships further.
In contrast, no relationships between anxiety and apathy, CAG repeat length, cognitive ability, motor performance, or disease progression were found. These findings indicate that anxiety does not follow the trajectory of the disease.
8,15 It has been postulated that the peak of anxiety symptoms at around stage 2 of the disease may be indicative of changes that are occurring in the patient’s life associated with increasing loss of independence and/or an increase in pathological changes in the basal ganglia.
8 Pain was found to independently predict anxiety in HD, and this area is worthy of further exploration in future studies. So far, there is limited research into the sociodemographic factors that might be associated with anxiety in HD, but no relationship with gender or age has been found.
Regarding the literature on interventions for anxiety in HD, this review identified little evidence of well-designed studies that demonstrated an improvement in anxiety in HD after a medical or psychological intervention. Three interventions have yielded promising results: 1) olanzapine; 2) a psychological intervention; and 3) an intensive multidisciplinary program, but none of these methods were controlled or randomized. All of these interventions were not specifically addressing anxiety but were wider studies examining a number of HD symptoms. There is a need for more robust intervention studies that are randomized, controlled, and blinded with a larger number of participants. A single case study of cognitive-behavioral therapy for a premanifest HD carrier revealed significant relief of anxiety,
53 and wider trials of this approach could be undertaken among this group, which may enable carriers to develop coping strategies before significant cognitive deficits arise. As relationships between anxiety, illness perceptions, and coping styles are apparent in HD,
21 more research in this area could help inform psychosocial interventions for HD.
This review had several limitations. First, our review was limited to articles published in English only and the studies included were relatively heterogeneous, which makes comparisons difficult. Some of the studies included in this review did not explicitly state how they determined whether or not participants were anxious. Most studies in this review excluded HD patients with severe dysarthria, dementia, and advanced-stage disease. The experience of anxiety in these groups requires further research, and suitable assessment methods will be needed. The use of caregiver report appears to show good usefulness in assessing psychopathology in advanced-stage HD.
51 Many of the studies included had small sample sizes; hence, larger-scale studies are required. A variety of assessment tools were used in the studies, with many studies using tools limited to just one item on anxiety. The majority of studies included in this review did not report whether the sample was receiving treatment of anxiety or had done so in the past. Of the studies that did report medication use, there was variation in how such use was reported making comparisons difficult. Furthermore, there is also the possibility that anxiety may have resulted as a side effect of psychotropic medication or that medication-induced akathisia may have been erroneously labeled as anxiety.
54The majority of studies of anxiety in HD have been restricted to psychometric measures. Future studies may wish to pursue other paradigms such as physiological or neuroimaging measures. The extent to which various (epi)genetic, organic, and environmental factors contribute to anxiety in HD is still unknown. Further research may help determine whether the symptoms are associated with the pathology of the disease itself or whether familial and other psychosocial factors contribute to the development of anxiety. Research examining the onset of anxiety in HD would enable a better understanding of critical points of risk for patients and also premanifest HD expansion carriers. Given the extent of anxiety symptomology found among HD expansion carriers, it is important that an evidence base is established regarding interventions that can be used to treat anxiety in HD. We hope that this review will provide a basis from which future studies may increase our understanding of this often debilitating, but neglected aspect of HD.