To the Editor: Case studies suggest that temporal brain degeneration and lesions may lead to pedophilic behavior in previously nonpedophilic men.
1 In contrast, the localization of neural alterations in genuine pedophilia is less straightforward, and treatment options are limited.
2 We report on a patient with lifelong pedophilia who also exhibited symptoms of schizotypal disorder and temporal epileptiform brain activity and responded to treatment with valproate.
Case Report
The patient, a 45-year-old, well-educated, highly functioning professional and father of a family, had sought therapeutic help in a program that provides confidential treatment free of charge for individuals who have a sexual preference for children. He insisted that he had never assaulted a child, despite having recurring fantasies that included aggressive sexual content. He consumed child pornography obsessively, and as a result was also afflicted with self-deprecating ruminations. His relationship with his wife seemed lacking in emotional attachment, and he reported that the couple had engaged in sexual activity solely for the purpose of conceiving children. Regarding his pedosexual interest and concomitant distress, he experienced an increasing desire for a supervisory body to control his child pornography consumption and even chemical castration. Previously, he had been prescribed fluoxetine 40 mg/day to treat a depressive syndrome. After a thorough diagnostic assessment, he was diagnosed with heterosexual pedophilia and scheduled for cognitive-behavioral therapy.
Several months after enrollment in group psychotherapy for pedophilia, the patient was referred for inpatient admission because of a deterioration of his depressive symptoms, including apathy and disturbed sleep. On the ward, he made himself conspicuous by circumlocutions, avoiding eye contact, an odd and aloof appearance, having poor personal hygiene, and exhibiting magical thinking without evidence of delusions or hallucinations. Psychodiagnostic testing revealed a far-above-average intelligence and high scores on scales for social introversion, femininity, depression, paranoia, and psychopathic deviation but no cognitive distortions pointing to schizophrenia. Considering his clinical presentation and psychodiagnostic assessment, the clinical syndrome most closely matched schizotypal disorder and fulfilled the corresponding criteria of both DSM-IV and ICD-10.
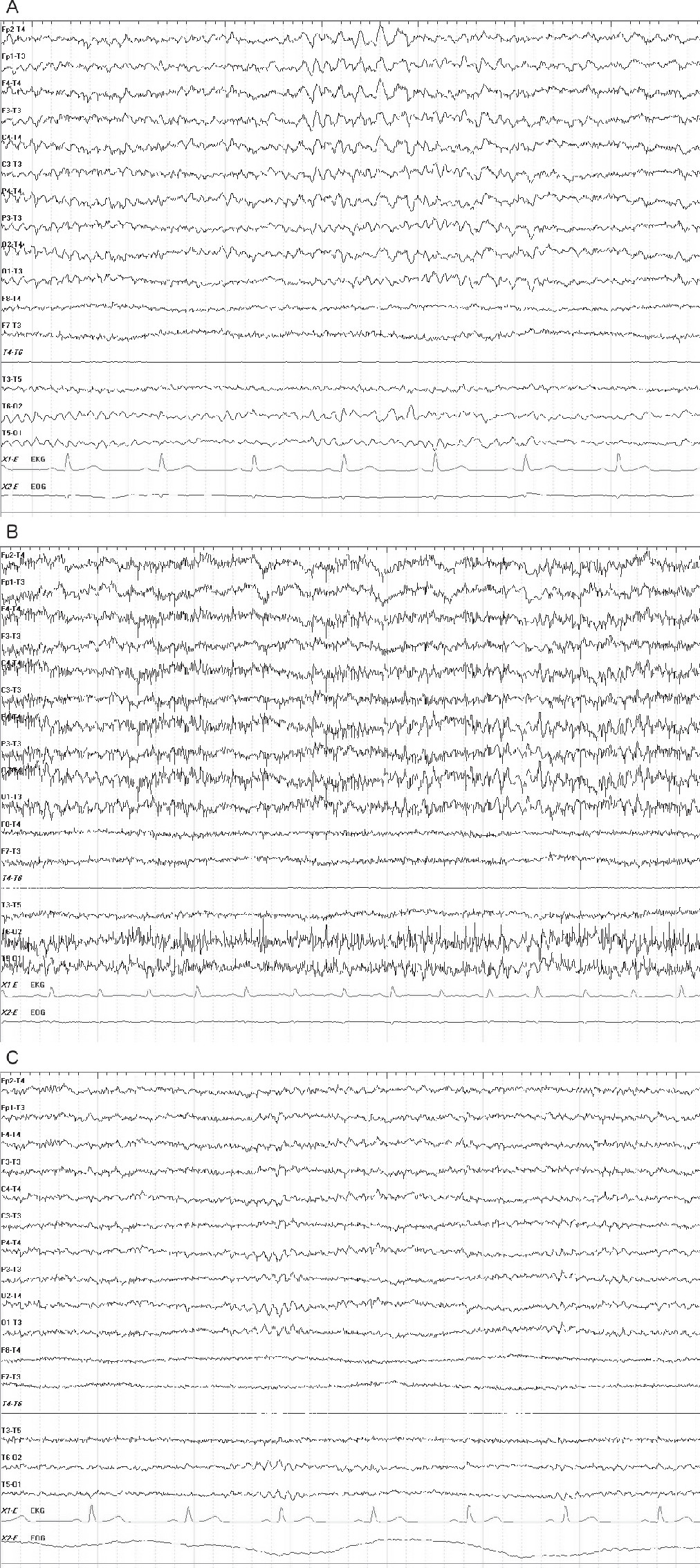
The patient reported no history of somatic disease. A physical examination and MRI examination revealed no abnormalities. However, a routine electroencephalographic examination revealed bilateral frontotemporal theta dysrhythmia with singular and grouped sharp waves (
Figure 1A). Hyperventilation provoked a tendency toward generalization of the epileptiform pattern (
Figure 1B). A third-party anamnesis provided by the patient’s wife disclosed repeated absence-like states. Subsequent administration of valproate (up to 1200 mg/day) normalized the epileptiform activity (
Figure 1C), improved the schizotypal symptoms (particularly with respect to circumlocution and affect), and reduced the patient’s obsessive desire to consume child pornography considerably. Discontinuation of the medication on the patient’s own initiative resulted in a recurrence of symptoms, while subsequent reintake led to notable relief again.
Discussion
The reproducible improvement of schizotypal and pedophilic symptoms following anticonvulsant treatment with valproate suggests a causal relationship between the epileptiform temporal activity and the clinical symptomatology, even if we cannot distinguish whether the epileptic activity in the temporal lobe was related to pedophilia per se or to the obsessive character of pedophilic desire. We also cannot exclude that valproate had an effect on pedophilia irrespective of its effect on epileptiform activity. However, our finding fits well with the notion that neurodevelopmental abnormalities in temporal regions may contribute to the etiology of pedophilia.
3MRI studies have revealed both structural and functional alterations in the temporal cortex of pedophiles. More specifically, voxel-based morphometric studies indicated reduced amygdalar, parahippocampal, and temporopolar gray matter as well as a decrease in global temporal white matter volume.
4–7 Functional abnormalities during processing of sexual stimuli were observed in the hippocampus as well as in the lateral and medial temporal cortices.
8,9 The present case extends these findings by demonstrating a relationship between epileptiform temporal activity and pedophilic behavior, which in turn could explain the near-complete resolution of pedosexual interest after anticonvulsant administration in a previous case.
10 While such a relationship is novel for genuine pedophilia, it has been shown that schizotypal symptoms correlate with early onset of seizures and a diagnosis of temporal lobe epilepsy.
11 Notably, schizotypal traits occur in pedophilic individuals with above-average frequency.
12 Taken together, these interrelations underline the contribution of temporal lobe dysfunction to the pathophysiology of pedophilic behavior.
Apart from etiological considerations, this case admonishes the clinician that in the face of “zebra diseases” such as pedophilia, the risk of overlooking additional pathology may be increased. The confirmed diagnosis of an exceptional psychiatric disorder must never replace further thorough physical examination and psychiatric assessment. Otherwise, appropriate treatment might be withheld from the patient inadvertently, causing unnecessary harm.