The construct of intolerance of uncertainty was originally identified as a key factor for the development and maintenance of generalized anxiety disorder.
5 However, since then, many studies have also confirmed the importance of intolerance of uncertainty for other anxiety disorders such as obsessive-compulsive disorder (OCD),
6–8 social phobia,
9 and posttraumatic stress disorder.
10 More recently, studies have demonstrated that elevated intolerance of uncertainty may play a role in a wider range of psychological disorders such as major depressive disorder,
11,12 eating disorders,
13–15 and psychosis.
16 These findings indicate that intolerance of uncertainty is not a ubiquitous characteristic specific to generalized anxiety disorder or other anxiety-related disorders; rather, it is a transdiagnostic cognitive vulnerability factor underlying various psychiatric disorders and general psychopathology.
Indeed, independent of the disorder, elevated intolerance of uncertainty has been associated with dysfunctional behaviors such as perseverative information seeking, impaired decision making, and poor (social) problem solving.
17 However, it is important to keep in mind that intolerance of uncertainty, when not severely elevated, is not necessarily harmful. From an evolutionary perspective, anxiety, as a consequence of intolerance of uncertainty, can have beneficial effects (e.g., on future decisions).
18 It remains unknown, however, as to what mechanisms cause some individuals with high intolerance of uncertainty to function well, whereas others experience intolerance of uncertainty–related cognitive, emotional, and behavioral problems.
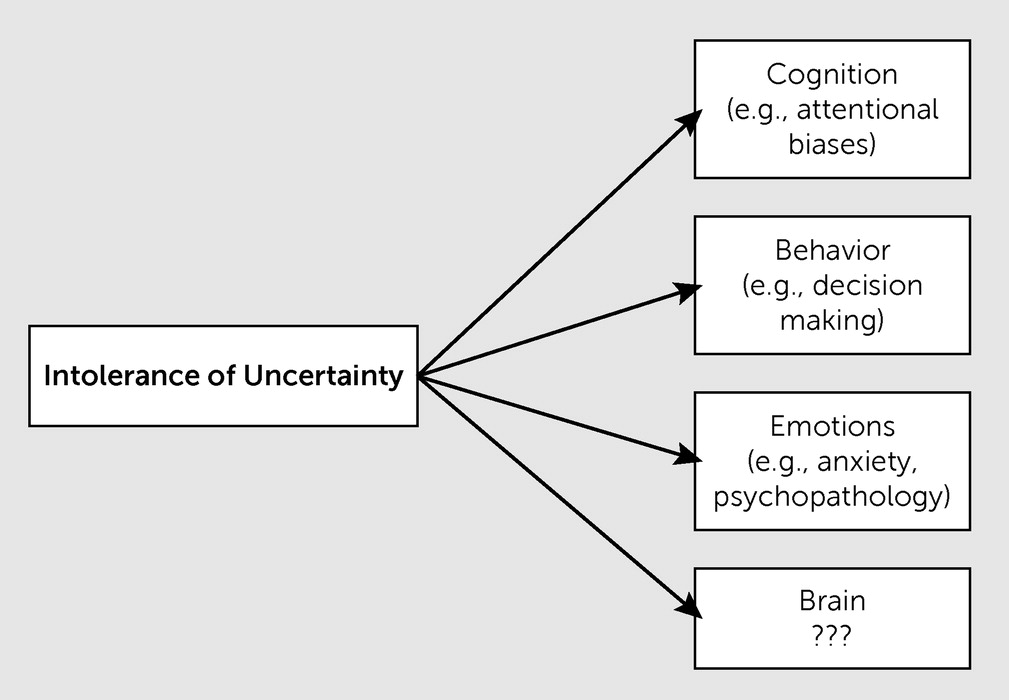
In order to unravel the processes through which intolerance of uncertainty contributes to disturbed psychological functioning, it might be beneficial to elucidate the biological mechanisms associated with intolerance of uncertainty. In particular, examining neural pathways will increase our understanding of intolerance of uncertainty and will help determine whether it is a shared vulnerability factor for psychopathology (like neuroticism) or whether intolerance of uncertainty–associated processes are disorder dependent. Understanding the neural mechanisms of intolerance of uncertainty in relationship to psychopathology may contribute to the development of more appropriate (pharmacological) treatment opportunities in the future.
Although there is limited knowledge about neural pathways for intolerance of uncertainty, we propose a potential neural circuitry underlying the intolerance of uncertainty based on the literature on anxiety. As explained earlier, cognitive and behavioral models of anxiety place intolerance of uncertainty at the heart of anxiety
5 and regard intolerance of uncertainty as a key predictor for anxiety-related behaviors. In these models, it is assumed that for those with high intolerance of uncertainty, uncertainty is related to a negative emotion (e.g., worry or anxiety) and associated behavioral processes such as avoidance. This suggests that intolerance of uncertainty–related brain activity will be most prominent in the core limbic system. The amygdala in particular plays an important role in registering emotional stimuli and has been implicated in anxiety, among other disorders, by neuroimaging studies on emotion processing.
19 For those individuals with high intolerance of uncertainty, this will include stimuli that elicit uncertainty. Furthermore, this review concludes that the dorsomedial prefrontal cortex may be implicated in the evaluation of these uncertain (and thus emotional) stimuli, whereas the ventromedial prefrontal cortex (vmPFC) may play a role in subsequent regulation of emotions that follow from experiencing uncertainty. Moreover, given the evidence that intolerance of uncertainty (like anxiety) affects decision-making processes,
20 it is very possible that the medial and dorsolateral prefrontal cortex (DLPFC) is activated during decision making in uncertain situations in individuals with high intolerance of uncertainty. In particular, one would expect altered activation in the dorsal anterior cingulate cortex and vmPFC in individuals with high intolerance of uncertainty compared with those with low intolerance of uncertainty.
This review aims to provide an overview of the current literature on the neural correlates of intolerance of uncertainty by 1) reviewing studies investigating neural pathways related to uncertainty and intolerance of uncertainty and their associated cognitive and behavioral processes in nonclinical samples, and 2) examining intolerance of uncertainty–related neural correlates in clinical samples. In addition, we establish the overlap in intolerance of uncertainty–related brain regions between clinical disorders characterized by elevated intolerance of uncertainty.
Neural Correlates of Uncertainty and Intolerance of Uncertainty
To provide better understanding of the underlying brain mechanisms of intolerance of uncertainty, we first discuss how uncertainty in general is processed in the human brain, building on human functional neuroimaging studies using functional magnetic resonance imaging that focus on how anticipation to uncertainty is represented in the brain. The concept of uncertainty that we refer to in this review includes anticipation to future-related uncertainty. Therefore, it is important to note that the studies in healthy individuals discussed in this review make use of functional magnetic resonance imaging paradigms that focus on the induction of sustained uncertainty to measure the neural correlates of uncertainty during anticipation of future events. Important brain areas that have been identified in such studies are the insula, amygdala, anterior cingulate cortex, vmPFC, DLPFC, and posterior frontomedian cortex.
21–25Substantial evidence has been accumulated supporting strong reciprocal connections among the insula, amygdala, anterior cingulate cortex, and vmPFC. Activation in these brain areas increases in response to anticipation to uncertainty, resulting in an imbalance in this circuit. The insula plays an important role in the representation of subjective emotional awareness and interoception in the present, as well as in the prediction of our future subjective feelings about events that might happen in the future.
26 Increased insula activation during anticipation to uncertainty can be interpreted as the brain making predictions about how one is going to feel in response to a possible outcome. The amygdala is strongly involved in emotional responses and the focus of attention to possibly threatening situations, and the anterior cingulate cortex plays an important role during conflict situations in the brain as well as in anticipation of (aversive) future events.
22,26,27The vmPFC plays an important role in inhibiting the amygdala and insula, which protects these brain areas from becoming hyperactive.
22,26,28 As a result, healthy individuals with heightened levels of intolerance of uncertainty do not have to suffer from negative effects induced by uncertain situations. How the vmPFC contributes to this tolerance of uncertainty in healthy individuals is twofold. First, the vmPFC plays an important role in the activation of a coping mechanism to deal with the experienced uncertainty. Thus, an increase in activation in this area means that the brain is trying to cope with the uncertainty. Second, the vmPFC is important in learning about and responding to safety cues in potentially threatening uncertain situations. Increased vmPFC activation reflects searching for environmental information that can diminish the threatening feeling of uncertainty by increasing the probability that negative events are prevented.
26 Thus, vmPFC activation suppresses emotional responses as a reaction to threatening situations.
In addition, research in healthy individuals proposed that there is a difference between brain areas responding to phasic uncertainty (short term) and brain areas responding to sustained uncertainty (long term). Phasic uncertainty activates the central nucleus of the amygdala, whereas sustained uncertainty activates the bed nucleus of the stria terminalis.
29Neural Correlates of Uncertainty and Intolerance of Uncertainty in Clinical Disorders
In addition to the determination of the neural correlates of uncertainty in healthy individuals, it is of interest to investigate the brain areas that may underlie intolerance of uncertainty in clinical disorders and how those brain areas relate to the dysfunctional cognitive and behavioral responses resulting from intolerance of uncertainty. Although the literature on the neural correlates of intolerance of uncertainty in clinical samples is sparse, several interesting studies have been conducted in patients with generalized anxiety disorder and OCD.
30–32 Although the same brain areas are activated during anticipation to uncertainty in patients and controls (i.e., the amygdala, vmPFC, DLPFC, anterior cingulate cortex, and orbitofrontal cortex [OFC]), the extent to which these regions are activated and the connectivity among these areas differ between both samples.
Interestingly, many brain areas that are activated during the anticipation to uncertainty in healthy individuals show hyperactivation in clinical samples. One such region is the amygdala. A dysfunctional behavior that results from hyperactivation of the amygdala is hypervigilance, which is characterized by a biased attention to threatening and negative stimuli (i.e., uncertainty) and an altered information-processing style biased toward threatening and negative stimuli instead of safety cues (signals that can solve the uncertainty).
26 Several studies in patients with generalized anxiety disorder and social phobia identified hyperactivity of the amygdala as responsible for the increased vigilance toward threat cues, which is specific for patients with these pathologies.
33–35 Moreover, Krain et al.
30 reported that bilateral amygdala activity correlates positively with Intolerance of Uncertainty Scale scores in anxiety disorders.
In addition to the amygdala, hyperactivation in the DLPFC might also play a role in the hypervigilant state of patients with high intolerance of uncertainty. The DLPFC is involved in updating information on environmental stimuli to predict certain outcomes and thus contributes to the state of facilitated threat detection. Rotge et al.
31 reported enhanced DLPFC activation in patients with OCD, a clinical sample prone to reside in a vigilant state. In that study, patients with OCD and healthy controls were asked to decide whether two pictures were different or identical, after which they had the opportunity to check their decision to provoke checking behavior. Although the correlation between intolerance-of-uncertainty scores and checking behavior did not differ significantly between the groups, only the intolerance-of-uncertainty scores of patients with OCD correlated positively with DLPFC activation.
31 This may be explained by enhanced DLPFC activation in patients with OCD after the feeling of uncertainty, which leads to a constant update of the available information concerning the decision they made. As a consequence, these individuals show increased vigilance toward uncertain situations, resulting in the maintenance of their checking behavior.
The OFC is another part of the prefrontal cortex in which hyperactivation induced by intolerance of uncertainty might be associated with dysfunctional behavior. Previous research in healthy individuals established that the OFC detects the valence of rewards. Furthermore, it has been proposed that, similar to the DLPFC, this information is used to bias future decisions. Hsu et al.
33 were among the first to study the association between uncertainty and the OFC. They identified a positive correlation between OFC activation and uncertainty during experimental manipulation of (or intolerance of) uncertainty in healthy individuals. Accordingly, this part of the OFC has been linked to the pathology of intolerance of uncertainty; patients with anxiety disorder and OCD show a positive correlation between OFC activation and the degree of manipulated uncertainty.
30–32 Although it was initially expected that the severity of the clinical disorders was related to this enhanced OFC activation, these findings suggest an important role for heightened intolerance of uncertainty.
Heightened intolerance of uncertainty is not limited to clinical populations. The study by Krain et al.
30 found that anxious individuals with low intolerance of uncertainty show deactivation of several frontal and limbic areas, including the OFC, whereas anxious individuals with high intolerance of uncertainty show hyperactivation in these areas. The healthy control group showed no change in OFC activation. Krain et al.
30 explained this finding by speculating about a possible coping mechanism that protects anxious individuals with low intolerance of uncertainty from stress and anxiety by the deactivation of several frontal and limbic areas, which probably serves as an emotion regulation strategy. This explanation sounds plausible knowing that the amygdala, which is strongly involved in emotion regulation, was also deactivated in this study. As a consequence, this allows healthy controls to manage uncertain situations better than anxious individuals with high intolerance of uncertainty in which these emotionally related brain areas were hyperactive.
30 Although there was a significant difference in intolerance of uncertainty between the anxiety group and the control group, it is noteworthy that this was a study in adolescents.
30 This observation hampers direct comparisons with studies in adults.
Rotge et al.
31 found that intolerance of uncertainty–related OFC activity in patients with OCD during checking was not influenced by an error or by their checking behavior. By contrast, intolerance of uncertainty–related OFC activity in the healthy control group increased after an error and decreased after checking behavior. This means that in patients with OCD, the stress induced by uncertainty was not enhanced by an error or diminished by their compulsive checking behavior.
Increased anterior cingulate cortex activation has been related to intolerance of uncertainty in anxiety disorder as well as in OCD.
30,32 In the study by Krain et al.,
30 intolerance-of-uncertainty scores of patients with anxiety disorder correlated positively with greater activation in the rostral and subgenual portions of the anterior cingulate cortex during a decision-making task, in which patients had to choose whether the value of the subsequent card was higher or lower than the presented card. Furthermore, the anterior cingulate cortex was also part of the regions that were hyperactivated in the group with anxiety and high intolerance of uncertainty and were deactivated in the group with anxiety with low intolerance of uncertainty, whereas the control group showed no change in activation during task-induced uncertainty.
Stern et al.
32 found that increased activation in the subgenual cingulate cortex, which is the anterior continuation of the anterior cingulate cortex, during decision making was negatively associated with the amount of uncertainty that patients with OCD experienced. The more evidence was accumulated, the more certain the decision was, and the greater the activation observed in the subgenual cingulate cortex. Thus, patients with OCD showed hyperactivation in this area during uncertain situations because of evidence accumulation. Remarkably, no significant differences were found between the patients with OCD and healthy controls, which again supports the idea that intolerance of uncertainty is not specific to a certain clinical disorder but instead might be a broader aspect of the etiology of uncertainty.
The involvement of the subgenual cingulate cortex in the processing of uncertainty is an interesting finding for several reasons. Previous research in patients with major depressive disorder indicated a prominent role of the subgenual cingulate cortex in its pathogenesis. Thus, the potential role of the subgenual cingulate cortex in the etiology of intolerance of uncertainty provides further evidence for the hypothesis that intolerance of uncertainty is a key feature of major depressive disorder as well.
36,37 Furthermore, imaging data have indicated that patients with both OCD and generalized negative affect show excessive resting-state activity in this brain area.
32,36,37There is accumulating evidence indicating a relationship between intolerance of uncertainty and increased activation in brain regions that are involved in the default mode network. An important characteristic of the default mode network is that it becomes active when individuals are not focused on the external environment but are involved in self-focused internal thought processes such as imagining and predicting the future, autobiographical memory, and scenario construction. The most prominent brain structures involved in the default mode network are the vmPFC, dorsomedial prefrontal cortex, lateral temporal cortex, hippocampus, parahippocampus, and inferior parietal cortex.
32,38–40 Task execution commonly caused deactivation in the default mode network.
41,42 However, in the study by Stern et al.,
32 patients with OCD showed greater activation in several nodes of the default mode network and some brain regions closely linked to these nodes during the execution of a decision-making task in which uncertainty was experimentally manipulated, in contrast with healthy controls. The activated areas included the vmPFC, parahippocampus, middle temporal cortex, and temporal pole. Stern et al.
32 proposed that a possible explanation for the overlap between these brain regions and brain regions involved in the default mode network might be an overengagement of internally focused mental processes during the execution of these external task demands. This may be specific to imagining and predicting the future and the construction of associated future scenarios in patients with elevated intolerance of uncertainty.
32 However, to our knowledge, the literature on the relationship between intolerance of uncertainty and the default mode network is limited to the study by Stern et al.
32 and has thus far only been investigated in a sample of patients with OCD. Therefore, further research is needed to examine in more detail how intolerance of uncertainty modulates the default mode network in health and disease.
Although all of the above-mentioned brain regions showed hyperactivation in clinical disorders in contrast with healthy individuals during task-induced uncertainty, the underlying cause of this hyperactivation remains a matter of debate. Keeping in mind the key role of the vmPFC in the circuit involved in anticipation to uncertainty in healthy individuals, several possible functions of the hyperactivation are associated with intolerance of uncertainty. On the one hand, hyperactivation of the amygdala and the anterior cingulate cortex, which are both reciprocally connected with the vmPFC, might be the result of a lack of inhibitory input from the vmPFC, which may lead to the observed hyperactivation. On the other hand, there are studies in clinical samples with intolerance of uncertainty in which an increase in vmPFC activation was observed during anticipation to uncertain situations. Krain et al.
30 reported that intolerance-of-uncertainty scores correlated positively with hyperactivation in the medial frontal gyrus, which is part of the medial frontal cortex. Although Krain et al.
30 did not find a difference in activation of this area between the group with anxiety and the control group, a positive association between activation in the medial frontal gyrus and intolerance-of-uncertainty scores was found when both groups were pooled. On the one hand, this might suggest that hyperactivation in the medial frontal cortex is not specifically linked to the pathology of anxiety disorders but might be a ubiquitous trait of intolerance of uncertainty. On the other hand, it could also be a result of an increase in statistical power because of the increased sample after pooling the groups. More specifically, Stern et al.
32 reported that induced intolerance of uncertainty has been associated with hyperactivation of a brain network including the vmPFC. In this study, intolerance of uncertainty was experimentally manipulated such that some decisions were associated with no objective uncertainty, whereas other decisions contained varying levels of objective uncertainty based on displayed probabilities. By increasing the experimentally induced objective uncertainty within the task, patients with OCD showed increasing activation of the vmPFC compared with healthy individuals.
These studies suggest that a lack of inhibition from the vmPFC to the amygdala and anterior cingulate cortex is unlikely and that alterations in the connection between the vmPFC and the amygdala and anterior cingulate cortex lead to hyperactivation of the vmPFC, although these alterations are yet to be identified. This finding is supported by microstructural alterations found in the uncinate fasciculus, which is a white matter fiber bundle that connects ventral portions of the prefrontal cortex with the anterior cingulate cortex and amygdala and ends in the insular cortex in patients with generalized anxiety disorder, social phobia, and high-trait anxiety.
43–45 Thus far, we can only speculate about the role of hyperactivation observed in individuals with heightened intolerance of uncertainty, and further research is required in this area.
Homogeneity of the Neural Correlates of Intolerance of Uncertainty Across Different Clinical Disorders
The literature suggests that many clinical disorders—such as generalized anxiety disorder, social phobia, OCD, depression, posttraumatic stress disorder, psychosis, and eating disorders—share a deficit in coping with uncertainty. Unfortunately, we cannot conclude from current findings that these disorders also share common neural correlates associated with the construct of intolerance of uncertainty. The main reason for this is that there are no studies directly comparing neural correlates of intolerance of uncertainty across distinct clinical disorders. Furthermore, the studies included in this review have too many methodological differences to be comparable. Further research is needed to investigate the relevant intolerance-of-uncertainty brain regions identified in this review across disorders.
Of note, a recently made clinically related distinction differentiates prospective intolerance of uncertainty and inhibitory intolerance of uncertainty.
4,6,46–48 Prospective intolerance of uncertainty is referred to as anxiety in anticipation of future uncertainty, whereas inhibitory intolerance of uncertainty is referred to as inaction in the face of uncertainty. Both domains of intolerance of uncertainty seem to be differentially associated with distinct clinical disorders. Birrell et al.
46 and McEvoy and Mahoney
48 demonstrated that prospective intolerance of uncertainty is mainly associated with worry and obsessions, which are symptoms of disorders such as generalized anxiety disorder and OCD, whereas inhibitory intolerance of uncertainty is more related to inactivity and withdrawal, which are symptoms of disorders such as social phobia, panic disorders, and depression. Although it might be conceivable from a theoretical perspective that the neural correlates of prospective intolerance of uncertainty and inhibitory intolerance of uncertainty differ, there is currently no evidence supporting this. Further research is needed to clarify this bifurcation in neural correlates of intolerance of uncertainty in distinct clinical disorders.
A further point that should be made here is that the brain regions implicated in intolerance of uncertainty have also been linked to other problems associated with psychopathology. For example, altered DLPFC activation has been associated with cognitive inflexibility.
19 There is increasing interest in cognitive inflexibility in anxiety disorders such as panic disorder
49 and OCD as well as in unipolar depressive disorder
50 and eating disorders.
51 Moreover, the involvement of the limbic system confirms that emotion regulation processes may underlie various clinical disorders, including mood disorders, anxiety disorders, and eating disorders.
52Discussion
We discussed the current knowledge of the neural correlates underlying intolerance of uncertainty and their associated cognitive and behavioral processes in clinical and nonclinical samples. Furthermore, we aimed to determine whether clinical disorders with intolerance of uncertainty share common neural correlates associated with the construct of intolerance of uncertainty. First, we concluded that although the clinical presentation of intolerance of uncertainty has been studied extensively, studies relating to the neurobiological correlates of the construct are sparse and the majority of studies involve healthy individuals rather than clinical samples. Second, clinical studies suggest that elevated intolerance of uncertainty is related to hyperactivation in several frontal and limbic brain areas in response to experimentally manipulated levels of uncertainty. These results are in line with findings in healthy individuals, in which this hyperactivation is observed in similar brain areas involved in anticipation to uncertainty, namely the DLPFC, vmPFC, OFC, anterior cingulate cortex, and amygdala. However, for the clinical samples, although some brain areas were reported in multiple studies, some brain areas were only reported once. Furthermore, even within one clinical disorder, different brain areas were reported in association with intolerance of uncertainty.
There are a number of possible explanations for these findings. First, the broad variety in brain areas related to intolerance of uncertainty may be the result of many differences in methodology among studies. For example, of the three studies that focused on the neural correlates of intolerance of uncertainty as extensively discussed in this review, only Krain et al.
30 made use of the validated Intolerance of Uncertainty Scale, whereas the other two studies used self-developed 9- or 10-point scale self-reports to quantify experienced uncertainty. Moreover, the three included studies all used different paradigms to assess brain-related processes when making decisions under conditions of uncertainty.
A second explanation for the diversity of results lies with the variety of included samples. It is possible that distinct disorders and subtypes of disorders have distinct neural correlates of intolerance of uncertainty (e.g., different OCD subtypes such as washing, checking, and hoarding). For example, studies have shown that the relationship between the symptoms of patients with OCD with a checking and/or doubting subtype of the disorder and intolerance of uncertainty is stronger than the relationship between the symptoms of other OCD subtypes (e.g., washing and hoarding).
6,8,53,54 In addition, it is important to be aware of the broad variety in age ranges within the included clinical samples, which hampers direct comparison because of developmental differences. Krain et al.
55 previously identified evidence for these developmental differences in the processing of uncertainty, showing that similar paradigms can result in differential study outcomes for adolescents and adults because of differential stages of brain development. Third, almost all patients in the discussed studies were receiving pharmacologic treatment. Therefore, we cannot rule out the influence of such treatment on the results of these studies. A fourth and important explanation for variability in findings may lie with the concept of intolerance of uncertainty itself. Some tasks may tap more into uncertainty about a current situation (or uncertain stimuli) versus future-related uncertainty, and it remains unknown whether intolerance of ambiguity is associated with different neural circuits than intolerance of future-related uncertainty. Moreover, theoretical and clinical studies are starting to distinguish between prospective and inhibited related intolerance of uncertainty, whereby prospective intolerance of uncertainty seems to be linked more with cognitive-related processes and inhibited related intolerance of uncertainty refers to behavioral stagnation.
Future Research Directions
Despite its clinical importance, research into the neural pathways of intolerance of uncertainty is scarce. Understanding the neural processes underlying uncertainty in those with high intolerance of uncertainty may help to understand the cognitive and behavioral processes clinicians target in treatments and may thereby help inform treatment strategies for individuals with high intolerance of uncertainty. We suggest a number of potential steps. First, it is important that studies use uniform measures and paradigms and validated questionnaires. It is important to focus on the induction of future-related uncertainty rather than creating ambiguous situations in the present. Developing a uniform paradigm to experimentally induce future-oriented uncertainty in future participants contributes to a better comparability among the studies and will best mimic the natural response of people with high intolerance of uncertainty. We recommend using both functional magnetic resonance imaging to examine task-related activation and functional connectivity as well as resting-state functional magnetic resonance imaging, ideally combined with diffusion tensor imaging, to assess structural connectivity.
Future research should also try to establish whether neural correlates of intolerance of uncertainty are similar in different clinical groups and are associated with different symptoms. This would corroborate the transdiagnostic value of intolerance of uncertainty. The intolerance-of-uncertainty treatment model by Dugas et al.
56 may serve as a starting point for investigating different intolerance of uncertainty–related cognitions and behaviors. In addition, future studies should include both adolescents and adults to allow for conclusions regarding the developmental course of intolerance of uncertainty. Moreover, this review highlights the need to further investigate intolerance of uncertainty and its neural pathways in other clinical populations that have high anxiety. For example, high anxiety is the norm in eating disorders such as anorexia nervosa and bulimia nervosa. A need for control and certainty is key, particularly for individuals with anorexia nervosa; indeed, the first studies confirmed elevated levels of intolerance of uncertainty in patients with anorexia nervosa.
13,14 Current psychological treatments for anorexia are suboptimal at best, and understanding the neural circuit of intolerance of uncertainty may offer a different way to treat anorexia.
In summary, increasing evidence demonstrates the existence of specific neural correlates of intolerance of uncertainty. However, the neural correlates found thus far might be specific to ambiguity, rather than to future-oriented intolerance of uncertainty. Furthermore, there is no conclusive evidence on whether the neural correlates of intolerance of uncertainty differ among distinct patient groups with high intolerance of uncertainty, and studies in clinical samples other than individuals with anxiety disorders and OCD are especially lacking.
Thus, with the knowledge that intolerance of uncertainty is related not only to anxiety disorders but also to a variety of clinical disorders, it is extremely relevant to gain more knowledge about this topic. This will pave the way for the development of appropriate treatment methods for patients suffering from pathological intolerance of uncertainty. The application of neurofeedback or real-time functional magnetic resonance imaging is one example of a possible treatment method based on findings of functional magnetic resonance imaging studies. This sophisticated technique allows participants to monitor and alter their own brain activity in specific brain areas.
57 This is beneficial because participants can directly experience the consequences of their behavior on their brain activity and can learn to downregulate the hyperactivation in the brain areas responsible for intolerance of uncertainty. This may help to relieve their stress and anxiety-related behavioral responses during uncertain situations. In addition, understanding the neural correlates underlying intolerance of uncertainty may improve techniques such as deep brain stimulation and transcranial magnetic stimulation.
In conclusion, to pave the way for new treatment approaches for anorexia nervosa by targeting intolerance of uncertainty and the associated psychopathology, future research should focus on the development of a uniform methodology to study the neural correlates of intolerance of uncertainty and should include different neuroimaging methods. Moreover, it is of special interest to incorporate distinct clinical groups to corroborate the transdiagnostic value of intolerance of uncertainty.