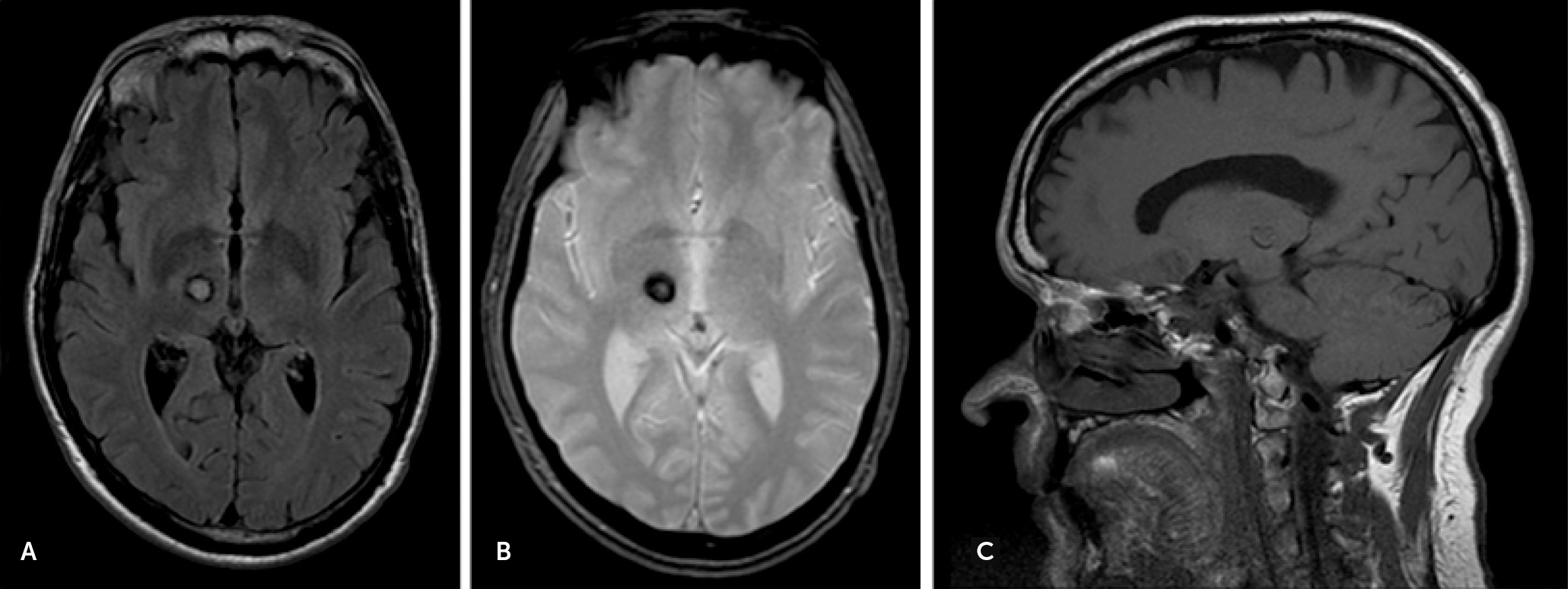
Behavioral Disconnection Syndrome Manifesting as Combined Mania and Visual-Auditory Hallucinations Secondary to Isolated Right Thalamic Hemorrhage
Case Report
Discussion
Mania
| Study | Sex | Age (Years) | Locations | Hemisphere | Onset | Etiologies | Manic Symptoms | Associated Symptoms | Treatment |
|---|---|---|---|---|---|---|---|---|---|
| Cummings et al.13 | Two cases | NA | Unspecified | Right | Acute | Ischemic stroke | Case 1: euphoria, talkativeness, hypersexuality, euphoric, irritable, and poor judgement | Hemisensory loss, amnesia, denial of illness, and depression (case 2) | Lithium in one case with improvement; no medication in one case |
| Case 2: euphoric, decreased need for sleep, and preoccupied with religion | |||||||||
| Gentilini et al.14 | Male | 66 | Paramedian | Right and Left | Acute | Ischemic Stroke | Hypersexuality, grandiosity, and cheerfulness | Amnesia, somnolence, and delusion | Not reported |
| Female | 47 | Paramedian | Right and Left | Acute | Ischemic stroke | Hyperphagia, euphoria, and childish behaviors | Hypersomnolence, abnormal eye movement, and depression | Not reported | |
| Male | 35 | Paramedian | Right and Left | Acute | Ischemic stroke | Hyperphagia and irritability | Amnesia | Not reported | |
| Bogousslavsky et al.6 | Female | 72 | Paramedian, dorsomedial and ventral lateral | Right | Acute | Ischemic stroke | Smiling and inappropriate laughing and jokes, logorrhea, rapid switching of ideas, lack of spontaneity, and disinhibition | Hypersomnolence, disorientation, | Not reported |
| Starkstein et al.15 | Three cases | NA | Unspecified | Right | NA | Hemorrhage and ischemic stroke | Mania (unspecified symptoms in each case) | NA | NA |
| Kulisevsky et al.16 | Female | 81 | Ventral lateral and ventromedial | Right | Acute | Ischemic stroke | Euphoria, talkativeness, grandiosity, flight of ideas, inappropriate jokes, and decreased need for sleep | Left hemichorea | Haloperidol with improvement after 4 weeks |
| McGilchrist et al.17 | Male | 43 | Paramedian | Right and Left | Acute | Ischemic stroke | Cyclic elation, hypersexuality, hyperphagia, flight of ideas, and decreased need for sleep | Hypersomnolence, cyclical apathy and depression | Not reported |
| Daum et al.18 | NA | 64 | Anterior | Right | Acute | Ischemic Stroke | Hypersexuality, talkativeness, irritability, mood fluctuation, and verbal aggression | Amnesia | Not reported |
| Vuilleumier et al.19 | Male | 63 | Unspecified | Right | Acute | Ischemic stroke | Mania episode followed by hypomania | Prosopoaffective agnosia | Not reported |
| Leibson20 | Male | 53 | Unspecified | Right | Acute | Hemorrhage | Talkativeness, cheerfulness, hypersexuality, and increased energy | Anosognosia, headache and left-sided numbness and weakness, gaze problem, and hemineglect, | Resolved 10 weeks after the stroke |
| Inzelberg et al.21 | Male | 61 | Pulvinar | Right | Acute | Ischemic stroke | Euphoria, talkativeness, disinhibition, flight of ideas, hypersexuality, decreased need for sleep, and increased goal-directed activity | Left hemichorea | Haloperidol with improvement after 8 weeks |
| Benke et al.7 | Male | 38 | Dorsomedial, intralaminar and anterior | Right and Left | 4 weeks | Ischemic stroke | Logorrhea, restlessness, mood elevation, inflated self-esteem, reduced need for food and sleep, and hypersexuality | Amnesia, vertical gaze paralysis, and dysarthria | Low-dose neuroleptic with improvement after 8 weeks |
| Lopez et al8 | Male | 63 | Unspecified | Right | 5 months | Ischemic stroke | Cyclic mania | Bipolar symptoms with cyclic depression, and melancholic stupor | Risperidone, valproic acid, and quetiapine for mania |
| Routh and Hill22 | Male | 83 | Posterior | Right | 2 weeks | Hemorrhage | Aggressiveness, speech disinhibition, talkativeness, flight of ideas, and inflated self-esteem | Paranoid delusions | Olanzapine |
| Julayanont et al. (current case) | Male | 55 | Dorsomedial and pulvinar | Right | Acute | Hemorrhage | Irritability, grandiosity, combative speech, high-energy levels, decreased need for sleep, pressurized speech, euphoria, and inappropriate cheerfulness | Paranoid delusions and amnesia | Risperidone with improvement after 4 weeks |
Peduncular Hallucinosis
| Study | Sex | Age (Years) | Locations | Hemisphere | Etiologies | Onset | Hallucination Features | Associated Symptoms | Treatment | |
|---|---|---|---|---|---|---|---|---|---|---|
| Visual | Auditory | |||||||||
| Feinberg and Rapcsak23 | Male | 83 | Dorsomedial | Right | Ischemic stroke | Acute | Animals in his house (flying birds and dogs), military marching, girls in an examination room | No | Vertigo, ataxic gait | Resolved in 1 week |
| Serra et al.24 | Male | 68 | Posterior | Right | Ischemic stroke | Acute | Animals and men’s head | No | Left hemiparesis, paraesthesias | Not reported |
| Inzelberg et al.25 | Female | 75 | Unspecified | Left | Ischemic stroke | 2–3 days | No | Musical hallucination of popular songs from her youth | Right hemiparesis and dysphasia | Improved with no reported treatment |
| Noda et al.26 | Male | 72 | Dorsomedial | Right | Ischemic stroke | 3 days | Vivid recollection of his old job, dish of sweet potatoes and cigarette between his fingers | No | Hypersomnolence and nocturnal insomnia | Resolved over 2 weeks with no reported treatment |
| Female | 46 | Anterior | Left | Ischemic stroke | 4 days | Parents who passed away 10 years ago, teapot and teacups on a table | Commanding voice: “Don’t eat” | Memory impairment, right upper limb weakness | Resolved over 2 weeks with no reported treatment | |
| Manford and Anderson27 | Male | 58 | Pulvinar | Right | Ischemic stroke | 10 days | Ball of light, a man in a suit, a black butterfly, dwarves, striped fish swimming | No | No | Not reported |
| Yoshida et al.28 | Female | 73 | Dorsomedial | Left | Ischemic stroke | 2 months | No | Voices telling her about misfortunes, voices of threats and commands, | Anterograde and retrograde amnesia | Risperidone and olanzapine |
| Mollet et al.29 | Female | 61 | Lateral | Right | Ischemic stroke | Acute | College-age boys in colorful Hawaiian shirts, men in black religious clothes | Conversation between college boys | Pain and numbness at the left hemibody | Not reported |
| Güzelcan et al.30 | Male | 46 | Unspecified | right | Tumor | Not reported | Parades of people, seeing spiders, mice running | No | No | Risperidone |
| Mittal and Khan31 | Female | 19 | Ventroanterior | Left | Ischemic stroke | Acute | No | Commanding Voices | Confusion, flat affect, imaginary boyfriend, and paranoid delusion | Risperidone |
| Lee et al.32 | Male | 20 | Anterior | left | Ischemic stroke | Acute | Dangerous hands and snakes | No | Amnesia, anomia, and depersonalization | Not reported |
| Fornazzari et al.12 | Male | 45 | Lateral and posterior | Left | Hemorrhage | 9 months | Sound-tactile, sound-color, and grapheme-gustatory synesthesias | No | Not reported | |
| Delgado and Bogousslavsky33 | Male | 61 | Dorsomedial | Left | Ischemic stroke | Acute | Body distortion above the waist, lights and mice running down the wall | No | Transient perioral and left paresthesias | Disappeared without treatment |
| Female | 48 | Paramedian | Right and Left (right >left) | Ischemic stroke | Acute | No | Voice and noise distortion made by “dinosaurs” | Disorientation | Disappeared without treatment | |
| Julayanont et al. (current case) | Male | 55 | Dorsomedial and pulvinar | Right | Hemorrhage | 12 months | Transient texts on his phone, unknown people and colorful airplanes | Musical hallucination | Paranoid delusions and amnesia | Risperidone |
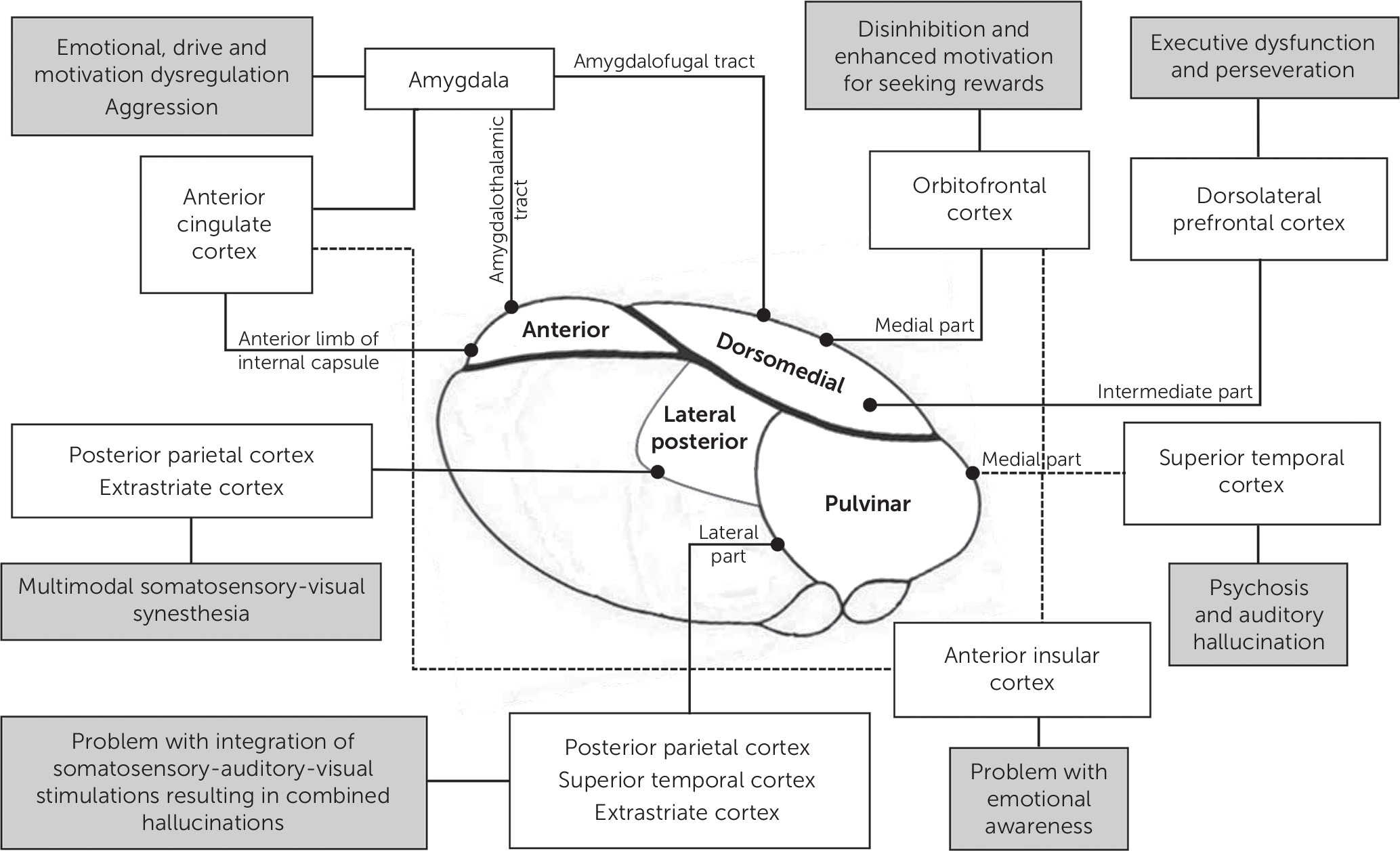
Network Model of Mania and Hallucinations Secondary to Thalamic Insults
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).