A Neuropsychiatric Analysis of the Cotard Delusion
Abstract
Methods
Results
| Patient | Sex and Age at Onset of Cotard Delusions | Description of Cotard Delusions | Cotard Delusions Occurring in the Context of the Following Signs/Symptoms/Diagnoses | Other Delusions or Psychoses | Other Unusual Behaviors | Treatments Tried and Response |
|---|---|---|---|---|---|---|
| 1 | 44 M | Described feeling as though he was no longer alive and that he did not think that anyone could kill him because he was not alive anyway. | Worsening of his mood symptoms, hallucinations, delusional thinking, and self-injurious behaviors over the last few weeks; PMH of bipolar disorder, borderline personality disorder, polysubstance dependence (alcohol and opiates) in full sustained remission, and cluster headaches. | Visual hallucinations of rats running across the baseboard, spiders on the wall, and people’s faces melting. | None described | Dialectical-behavioral therapy plus buspirone (30 mg t.i.d.) plus lithium (900 mg b.i.d.) plus lamotrigine (200 mg b.i.d.) plus quetiapine (500 mg q.d.) plus clonazepam (1.5 mg q.d. for 5 days) resulted in complete resolution of symptoms. |
| 2 | 85 F | Became increasingly preoccupied with morbid thoughts about her own life and was convinced she was not alive and her life “was a lie.” | Subacute onset of depressive symptoms, including fragmented sleep; decreased energy; decreased interest in eating; depressed mood; and positive helplessness, hopelessness, and worthlessness. | Felt that people were trying to confiscate money from her and to steal her identity. | None described | Eight treatments of ECT plus quetiapine (titrated from 25 mg to 100 mg q.d.) plus lorazepam (0.5 mg PRN) plus citalopram (20 mg q.d.) resulted in resolution of symptoms within 21 days of presentation. |
| 3 | 74 M | Reported that he had been stabbed and killed at his nursing home. Referred to his bed as his “casket.” | Altered mental status with concern for psychosis and/or delirium. | Noted hearing the voice of “almighty God” telling him that people are dying on the hospital unit. | None described | Risperidone (1.5 mg q.d.) for 10 days resulted in complete resolution of symptoms. |
| Also convinced that wife was an imposter and an alien (Capgras syndrome). | ||||||
| Claimed that he was being fed cat food for dinner and that once they put “pins in the hamburgers,” because somebody “sabotaged them.” | ||||||
| 4 | 66 M | Believed he died in the hospital and had risen again on Easter Sunday; continued to have a fixed delusion over his “death” for several days until treated. | Steroid-induced psychosis | None described | None described | Removal of corticosteroid treatment resulted in complete resolution of symptoms after 20 days. |
| 5 | 65 M | Believed he died on the operating table during surgery. His proof was that the television screen light “keeps fading” and that this was the afterlife and he was being tested. | Encephalopathy and seizures in the postoperative setting after sedation in the ICU and without sleep for at least 48 hours | Hallucinating that other people were in the room | “Swatting” at staff members | Lacosamide (150 mg) for 4 days resulted in resolution of symptoms. |
| 6 | 35 F | Believed that her brain was rotting and that there were worms in her brain that she could feel. | Dehydration-induced psychosis in the setting of pyelonephritis, chronic paranoid schizophrenia, delusional parasitosis, and a history of opiate and benzodiazepam addiction. | Auditory hallucinations | None described | Fluid resuscitation and hydration resulted in alleviation of symptoms and return to baseline at 2 weeks. |
| 7 | 39 F | Insisted that she had died from an overdose given by the hospital staff; noted that she wants to sleep “in my coffin.” | Seizures, mild hyponatremia; PMH of paranoid schizophrenia, schizoaffective disorder, bipolar I disorder, and cluster B personality traits. | Paranoia | Intense eye contact | Lorazepam (2 mg q.d.) plus valproic acid (1000 mg q.d.) plus risperidone (8 mg q.d.) plus milieu therapy resulted in resolution of symptoms after 1 month. |
| 8 | 50 M | Believed that his arm had been cut off and his fingers were being ground up and that he was dying. | Medication-resistant psychotic disorder not otherwise specified, with history of polysubstance abuse and narcissistic personality traits. | Believed that the television was talking to him and this was when “the voices are the clearest.” | None described | One treatment of ECT drastically improved symptoms. |
| 9 | 30 M | Believed that he had died and was now in an in-between world, between the living and the dead. | Frontal lobe dysfunction and cognitive impairment (confirmed by neuropsychometric testing) and polysubstance abuse (marijuana and alcohol). | Paranoid behavior; for example, he would put on socks and ask, “Who put these on me?” | None described | Escitalopram (20 mg b.i.d.) plus risperidone (varying doses going as high as 4 mg q.h.s.) plus lurasidone (80 mg q.d.) for 1 month resulted in improvement of symptoms. |
| 10 | 39 F | Despite reassurance that she was not dead, she perseverated over the idea that she was not alive. | Sagittal sinus thrombosis; PMH of depression. | None described | Breath-holding spells (“Dead people don't breathe”), repetitive tongue protrusion-retraction movements for 1–2 hours, and mutism (possibly caused by suggestions told to her that dead people would not speak). | Lorazepam (2 mg cumulative) plus clonazepam (1.5 mg q.d.) for 22 days resulted in symptom resolution. |
| 11 | 67 M | Thought that there were bugs in his eyes, in his stomach, and in his bottom. Wanted to go to the doctor to have these removed, as he thought that the bugs were “killing him.” | Amantadine-induced psychosis in the setting supranuclear palsy diagnosis; PMH of depression. | None described | Standing in front of the mirror to brush his teeth and not doing anything for an hour. | Removal of amantadine resulted in slight improvement of symptoms, although follow-up data are limited. |
| 12 | 30 M | Believed that his internal body organs were being eaten by a virus and that he was going to die soon because of it. | No associated psychological or neurological diagnoses, but complaints of autonomic dysfunction and muscle twitching of undetermined etiology. | None described | None described | No treatments were pursued, and no follow-up data are available. |
| Patient | Imaging Type | Neuroimaging Findings | EEG Available | EEG Findings |
|---|---|---|---|---|
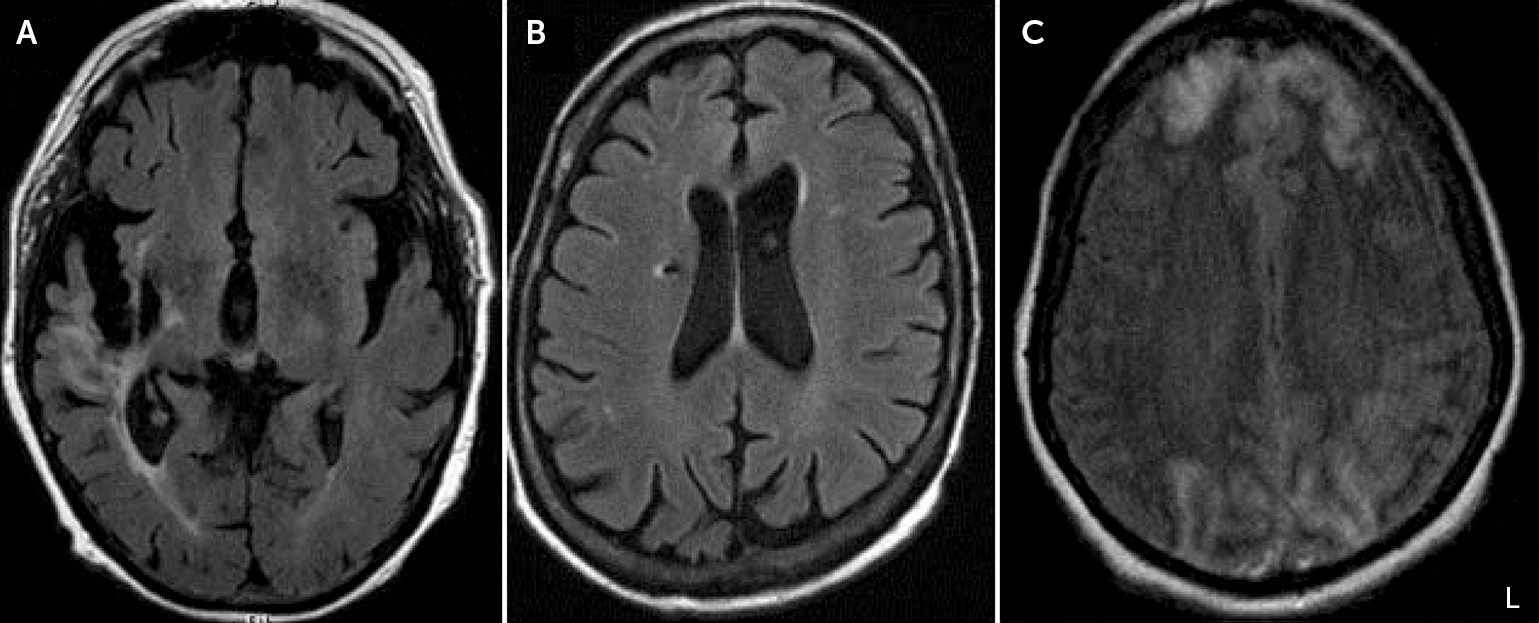
| 1 | MRI head | Few scattered foci of increased T2 signal in the white matter of the right frontal lobe. | No | N/A |
| 2 | MRI head | Moderate diffuse leukoaraiosis and parenchymal volume loss, more pronounced in both frontal lobes. | No | N/A |
| 3 | MRI and CT head | Chronic right MCA territory infarction with frontal-temporal lobe encephalomalacia and gliosis and Wallerian degeneration of the brainstem. Small amounts of associated blood products in the region of chronic infarct. Mild scattered leukoaraiosis. Moderate-prominent cerebral parenchymal volume loss. Right subinsular encephalomalacia periventricular hypoattenuation and dystrophic calcification. | Yes | EEG shows mild diffuse nonspecific background slowing (grade 1 dysrhythmia). No potentially epileptogenic activity was present during the recording. |
| 4 | MRI head | Negative | Yes | EEG shows some mild diffuse nonspecific slowing of the background and excessive beta. No potentially epileptogenic activity was present during the awake or sleep recordings. Dysrhythmia grade 1 generalized. The recording during wakefulness contains 9 Hz alpha activity over the posterior head regions. Some mild generalized slowing and increase in beta is seen. No abnormal activity occurred during photic stimulation. |
| 5 | MRI head | Chronic right corona radiata lacunar infarct with associated hemosiderin. Mild leukoaraiosis. Mild generalized cerebral and cerebellar volume loss with commensurate dilatation of the ventricular system. | Yes | EEG shows some mild diffuse nonspecific slowing of the background. Although the patient was intermittently drowsy throughout the recording, the mild slowing was also present during times of relative alertness. No potentially epileptogenic activity was present during the awake or sleep recordings. |
| 6 | MRI head | 2–3 small foci of T2 signal within the subcortical white matter of both cerebral hemispheres, likely ischemic or degenerative. | No | N/A |
| 7 | CT head | Negative | No | N/A |
| 8 | None | N/A | No | N/A |
| 9 | CT head | Negative | No | N/A |
| 10 | MRI head | Progression of previous bilateral cerebral hemisphere infarcts involving both frontal lobes anteriorly, both occipital lobes, and the right posterior frontal-anterior parietal lobes. Complete thrombosis of the superior sagittal sinus. MRI also demonstrates irregularity of both transverse sinuses, left greater than right, which may represent extension of the thrombus into the transverse and perhaps sigmoid sinuses. New cortical enhancement in a gyriform pattern present in the frontal and occipital lobes bilaterally and in both parietal lobes. | Yes | The portable EEG shows a moderate degree of nonspecific slowing over the bitemporal head regions. These findings are consistent with a focal disturbance of cerebral function or focal lesion involving these regions. |
| 11 | MRI head | Ischemic small-vessel disease in both cerebral hemispheres, without focal restricted diffusion, nor intracranial paramagnetic susceptibility effect. Generalized cerebral and cerebellar volume loss. | No | N/A |
| 12 | MRI head | Normal mild lateral ventricular asymmetry. | No | N/A |
Discussion
References
Information & Authors
Information
Published In
History
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).