Phineas Gage
It is due to science, that a case so grave, and succeeded by such remarkable results, should not be lost sight of; that its subsequent history, termination, and pathological evidences, in detail, should have a permanent record. —John M. Harlow
1
In 1848, Dr. John Martyn Harlow, a 29-year-old country doctor who had recently graduated from Jefferson Medical College in Philadelphia, wrote a letter to the
Boston Medical and Surgical Journal that would influence the future of neuropsychiatry. Harlow’s letter
2 and a brief follow-up note in January 1849
3 reported the case of Phineas Gage, whose survival and recovery after a severe, penetrating brain injury seemed so improbable that eminent physicians of the day dismissed it as a falsehood. The surgeon, Dr. Henry J. Bigelow, even financed Gage’s travel to Boston in 1850 in order to examine the patient and ascertain whether the story was true.
4 Though often misrepresented, one would be hard-pressed to find an introductory psychology textbook that does not make reference to this seminal case.
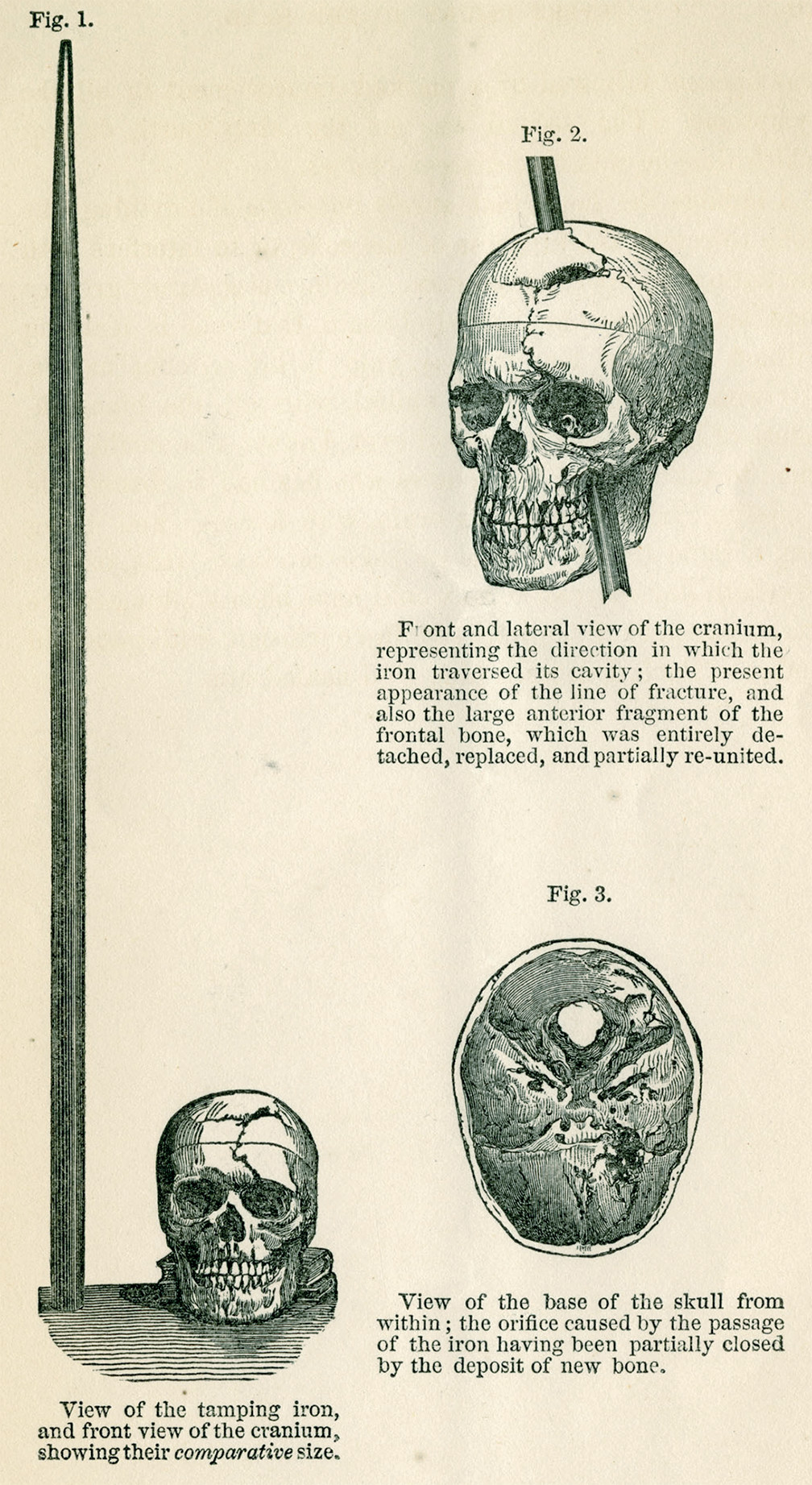
5At 4:30 p.m. on September 13, 1848, a premature blast at a railroad construction site in Cavendish, Vermont propelled a 43-inch long, 13.5-pound iron rod through the skull of Phineas Gage, a 25-year-old foreman. Before this accident, Gage was described as being of “vigorous physical organization, temperate habits, and possessed of considerable energy of character.”
2 The 1.25-inch diameter, smooth, tamping iron entered Gage’s skull beneath the left zygomatic arch, passed through the left orbit and left frontal lobe, and exited the top of his skull “in the median line, at the juncture of the coronal and sagittal sutures.”
2 (
Figure 1). The rod landed yards behind Gage and was “afterwards picked up by his men, smeared with blood and brain.”
1 Whether or not Gage sustained a brief loss of consciousness is unclear; observers noted a few impact convulsive movements of his upper extremities and that he spoke within minutes. “A great favorite” to his men, they drove Gage, sitting erect in an ox cart, for three-quarters of a mile to the Adams Hotel in Cavendish, Vt.
2 While sitting on the hotel porch, Gage told Dr. Edward Williams who first attended him, “Doctor, here is business enough for you.”
4 He then walked up the stairs with the doctor.
At 6:00 p.m., about 90 minutes after the accident, Dr. Harlow took over Gage’s care and attended him for months, making careful notes about his physical condition and fluctuating mental state. Initially lucid, Gage became transiently delirious 2 days later. Harlow noted that at times Gage was childish, but his orientation to time was good, and his memory for the accident was excellent.
2 Against all odds, Gage returned home 74 days after the accident. Harlow commented that aside from loss of vision in the left eye and partial paralysis of the left side of his face, Gage was in good physical health after recovery.
It was only in a follow-up paper 20 years later that Harlow described Gage’s behavioral changes after recovery. Gage had not been rehired as foreman because he had become disinhibited, with the “animal passions of a strong man,” “impatient of restraint or advice” and, “indulging at times in the grossest profanity (which was not previously his custom).”
1 Having formerly been regarded as smart, efficient and capable, Gage’s friends famously stated that after the accident he was “no longer Gage.”
1Gage traveled to Valparaiso, Chile in the late 1850s where he worked as a stagecoach driver. Dr. Henry Trevitt, who was well acquainted with Gage in Valparaiso, reported that Gage had no impairment of mental faculties.
6 Given the cognitive and motor skills needed to manage a six-horse stagecoach and deal with paying passengers, it can be assumed that Gage did experience additional recovery during the years after his accident. Gage later rejoined his family in California and worked as a farmhand at a succession of farms, “finding something that did not suit him in every place he tried.”
1 He died in February 1860, 12½ years after his accident, apparently from status epilepticus.
After learning of Gage’s death, Dr. Harlow obtained permission from Gage’s family to have the body exhumed and Gage’s skull sent to him along with the tamping iron that had been Gage’s “constant companion” after the accident.
1 The skull and tamping iron were donated by Harlow to the Museum of the Medical Department of Harvard University.
Importance
Gage is remembered as the index case of frontal lobe damage causing personality change, though the story that is told typically stops with the acute changes described by Harlow. Gage’s story teaches about behaviors associated with acute prefrontal injury as well as about the possibility of recovery from serious frontal damage in adulthood. That Gage later enjoyed some degree of functional recovery is perhaps as striking as his having survived the accident itself.
The case of Phineas Gage also added evidence for localization of mental functions. Dr. Harlow’s two reports bracketed in time Paul Broca’s report of “Tan” and the localization of language. We can assume Harlow had become aware of Broca’s work before writing his second paper about Gage. Thus, Drs. Harlow and Bigelow’s interest in Gage was part of a larger medical discussion regarding localization of mental functions.
Harlow’s descriptions of Gage were of great scientific value. He carefully described the circumstances of the accident, distinguishing his own observations from information that was derived from other sources. Harlow’s work was also exemplary in that he documented the anatomy of the injury as well as Gage’s mental status, then preserved the skull for study by future scientists.
In contrast to Harlow’s careful scientific reporting, other authors have distorted and embellished Gage’s story over the years. The extent of Gage’s personality change has been grossly overestimated, leaving the impression that he had become a sociopath.
5,7 Other authors have adhered to the myth that the iron rod was still lodged in his brain when he was brought to the doctor in Cavendish.
8 The case of Gage reminds us of the importance of detailed, accurate reporting of clinical encounters and of consulting primary sources when looking to the past.
Louis Victor Leborgne (“Tan”)
We speak with the left hemisphere. —Pierre Paul Broca
9
In 1861, French physician Pierre Paul Broca published his classic case of expressive aphasia: the patient was Louis Victor Leborgne, a 50-year-old man, now famously known as “Tan.” On April 11, 1861, Leborgne was transferred to the surgical ward at the Bicêtre Hospital in Paris because he had developed gangrene of his right leg; Broca was called to see him.
Broca made note of the patient’s history, including that he had been a long-term patient at Bicêtre and that he had been admitted because he had “lost the ability to speak.” On admission, it had been noted that Leborgne “differed from a sane man only in the loss of articulated speech.” According to Broca, Leborgne “understood almost everything that was said to him,” “but regardless of the question addressed to him, he always responded: ‘tan, tan.’” This verbal stereotype was “accompanied by a gesture of his left hand.”
10 At the hospital, apparently the patient was commonly called Tan.
11Ten years after Leborgne’s initial loss of expressive language and admission to Bicêtre, he gradually developed complete paralysis of his right arm followed by paralysis of his right leg. Leborgne was bedridden during the last 7 years of his life, finally succumbing to gangrenous bed sores.
11Broca reasoned from the evolution of Leborgne’s symptoms that “[the] probable diagnosis was therefore: original lesion in the left anterior lobe, propagated to the striate body of the same side.”
11 Broca deduced that Leborgne’s expanding hemiparesis had been an extension of the original lesion that had produced his expressive language deficit. From what was known at the time about motor control, Broca reasoned that the seat of expressive language had to be in the left hemisphere.
Leborgne died 6 days after Broca first saw him. When Broca had the opportunity to examine Leborgne’s brain at autopsy, he observed “a loss of substance of the cerebral mass” in the left anterior frontal lobe to which he attributed the loss of expressive language. A “softening extended well beyond the limits of the cavity” and these, presumably newer lesions, extended to the parietal lobe, the “temporal-sphenoidal” lobe, the insula and extraventricular nucleus of the striate body, the last of which caused paralysis of Leborgne’s right limbs.
10 150 years after the publication of Broca’s famous paper, medical historians located Leborgne’s death certificate and medical records which allowed access to more complete information about the patient and the course of his disease.
Leborgne, born on July 21, 1809, was one of six children in a middle class family. Like his educated siblings, Leborgne was likely somewhat educated himself.
12 It is known that Leborgne suffered from epileptic attacks beginning about age 24, but he was able to work. He was employed as a formier, an individual who creates wooden molds for hat or shoe manufacture.
11 In 1833, Leborgne was admitted for 6 days to the Hôtel-Dieu with headaches, diagnosed as “inflammation of blood vessels.”
13In the years after this first brief hospitalization, he eventually became unable to work, and his family declined to support him. Leborgne lost his expressive language ability; it is not known precisely when this occurred nor whether the loss was sudden or gradual. It is known that Louis-Maurice de Belleyme, the Prefect of Police of Paris, arranged for Leborgne’s residence at Bicêtre Hospital in Paris; Leborgne resided there from December 1834 until his death in 1861.
13There is now evidence that Leborgne “voluntarily transferred to the psychiatric ward” at Bicêtre and resided there from November 1852 to August 1853.
13 Broca did not discuss this transfer, and the details of any behavior that might have led to it are unknown. However, in 1861 Broca did describe Leborgne as “egoistic, vindictive and mean.”
13 Broca did not attempt to connect these observations with the area of Leborgne’s brain damage. The association of Broca aphasia with catastrophic reactions would not occur for nearly one hundred years.
14One hundred and forty-six years after Broca’s report, an MRI of Leborgne’s preserved brain revealed that the left hemisphere lesion extended more medially than had been appreciated by Broca.
15 The cause of Leborgne’s malady remains uncertain, although an inflammatory vascular etiology, possibly meningovascular syphilis, could explain the late progression of deficits in the same vascular territory as the initial deficits.
Importance
Broca’s presentation of Leborgne and, later that same year, another patient named Lelong, supported the concept of cerebral lateralization of language. Although “
it is customary to speak of Broca’s discovery as if it came like a clap of thunder from a clear sky,”16 Broca was not the first to suggest asymmetry in localization of cognitive functions. Marc Dax had argued 25 years earlier that certain brain functions were asymmetric, presenting cases of “aphemia” associated with left-sided brain damage, albeit without autopsy confirmation.
17 Broca also was not the first to associate language deficits with right hemiparesis; Hippocratic writers of 400 BC first made that observation.
In 1825 Jean Baptiste Bouillaud suggested the anterior localization of language.
18 On April 4, 1861, just one week before Broca first examined Leborgne, he had attended a meeting of the Anthropological Society of Paris and had heard Bouillaud’s son-in-law, Ernest Auburtin, argue for the frontal localization of language. Auburtin described his examination of a Mr. Coulerier whose failed suicide-by-gunshot had exposed the left frontal region of the patient’s brain. When Auburtin compressed Mr. Coulerier’s left frontal lobe with a spatula, he observed a speech arrest; release of the spatula allowed the return of language.
18When Broca presented Tan, he did not initially argue for the lateralization of language but rather for consideration of the cerebral convolutions in groups or functional regions. Broca’s main achievement was that he published a total of seven additional cases of aphasia after that of Leborgne, with careful autopsy correlation that ultimately provided evidence for the left inferior frontal gyrus as the seat of language.
9 Broca’s application of the clinico-anatomic method stands as a paradigmatic example of how to establish functional localization. In addition, the important role of history-taking in clinical reasoning is an often-overlooked feature of Broca’s work. He also anticipated the concept of neuroplasticity by suggesting that other brain regions might take on language functions during recovery from aphasia.
19In Leborgne’s postmortem examination, Broca took care to incise only the pia mater, noting: “as for the deep parts, I abstained from studying them so as not to destroy the specimen.”
10 Broca had the foresight to save this historically important brain for future study; by depositing Leborgne’s brain, along with fragments of dura mater and skull, in the anatomical museum in Paris,
12 he enabled the further elucidation of cerebral language networks that became possible when modern science developed advanced imaging probes.
Auguste Deter
Considering everything, it seems we are dealing here with a special illness…. There are certainly more psychiatric illnesses than are listed in our textbooks. —Alois Alzheimer
20
On November 3, 1906, at a meeting of Southwest German psychiatrists in Tübingen, a psychiatrist and neuropathologist named Alois Alzheimer presented the case of Auguste Deter. Alzheimer’s paper, entitled “On an Unusual Malady of the Cerebral Cortex,” described the clinical manifestations of this new syndrome and also “anatomical characteristics [found in the brain on autopsy] which set it apart from all recognized cases.”
20 Eighty-eight individuals attended the talk; no questions were asked at its conclusion.
21 Alzheimer’s 1907 publication of the Auguste Deter case also received little attention.
In 1901, Auguste Deter, a 51-year-old woman, was admitted to the Asylum for the Insane and Epileptic in Frankfurt am Main. She had been brought to the doctor by her husband for evaluation of pathological jealousy that had progressed to rapid memory loss. In addition, she had become disoriented in her home and had a fixed delusion that someone was trying to kill her. In the asylum, she was examined by Alzheimer and found to be confused and disoriented to time and place
22 with reduplicative paramnesia (acting as if the hospital was her home), intermittent auditory hallucinations, and lengthy bouts of screaming that worsened when anyone approached.
20 She alternated between believing that her attending physician was trying to harm her and then being overly familiar with him. Her short-term memory deficits were profound, forgetting objects shown to her almost immediately. Her language functioning was characterized by fluent, paraphasic, somewhat empty speech, with poor comprehension, impaired reading, and dysgraphia containing repeated or omitted syllables. She also was agnosic and apraxic.
20Four and a half years after admission to the asylum, Auguste Deter died at age 56, following a steady, downhill course. Alzheimer received Deter’s brain for analysis from the asylum’s director. He found “an evenly atrophic brain without macroscopic focal degeneration.”
20 After preparing over 250 histological slides and utilizing silver staining methods, he identified extracellular plaques and, for the first time, intracellular neurofibrillary tangles. Alzheimer prophetically noted, “A histological examination...will gradually lead to a clinical distinction of specific illnesses from the more general categories of our textbooks and it will enable us to define them clinically in greater detail.”
20For decades, the histological slides of Deter’s brain were lost. Then, in 1997, a year after psychiatrists at the University of Frankfurt discovered her original hospital records, a team of researchers located a trove of slides, each labeled “Deter,” in the basement of the Institute of Neuropathology of the University of Munich.
23 Microscopic review revealed that Auguste Deter indeed had the classical plaques and tangles that we now associate with Alzheimer’s disease. Even more remarkable was the genetic analysis of DNA retrieved from these slides and published in 1998.
24 Auguste Deter’s APO-E genotype was found to be E3/E3. Advances in genetic analysis of historical specimens may yet reveal more specific information about contributions to Deter’s dementia.
25,26Importance
Franz Nissl wrote of Alzheimer that he “was first and foremost a psychiatrist who strove to advance psychiatry by using a microscope.”
22 At the time of Alzheimer’s case report, Alzheimer’s disease had not been differentiated from other forms of mental illness. As recently as 1975, Medline indexed only 40 papers in which “Alzheimer’s disease” was a keyword.
27Auguste Deter was the first of several cases Alzheimer would investigate using the clinico-anatomic method, establishing the core elements of the clinical description and pathology of Alzheimer’s disease that remain valid today. Auguste Deter’s disease was almost certainly an aggressive, familial, early-onset variety. Its importance derives not only from Alzheimer’s description of the pathology but also from the fact that-Auguste Deter as well as Alzheimer’s second index case (Johann F. Taglohner) presented with psychiatric symptoms, an aspect of the disease that is often omitted from textbook descriptions.
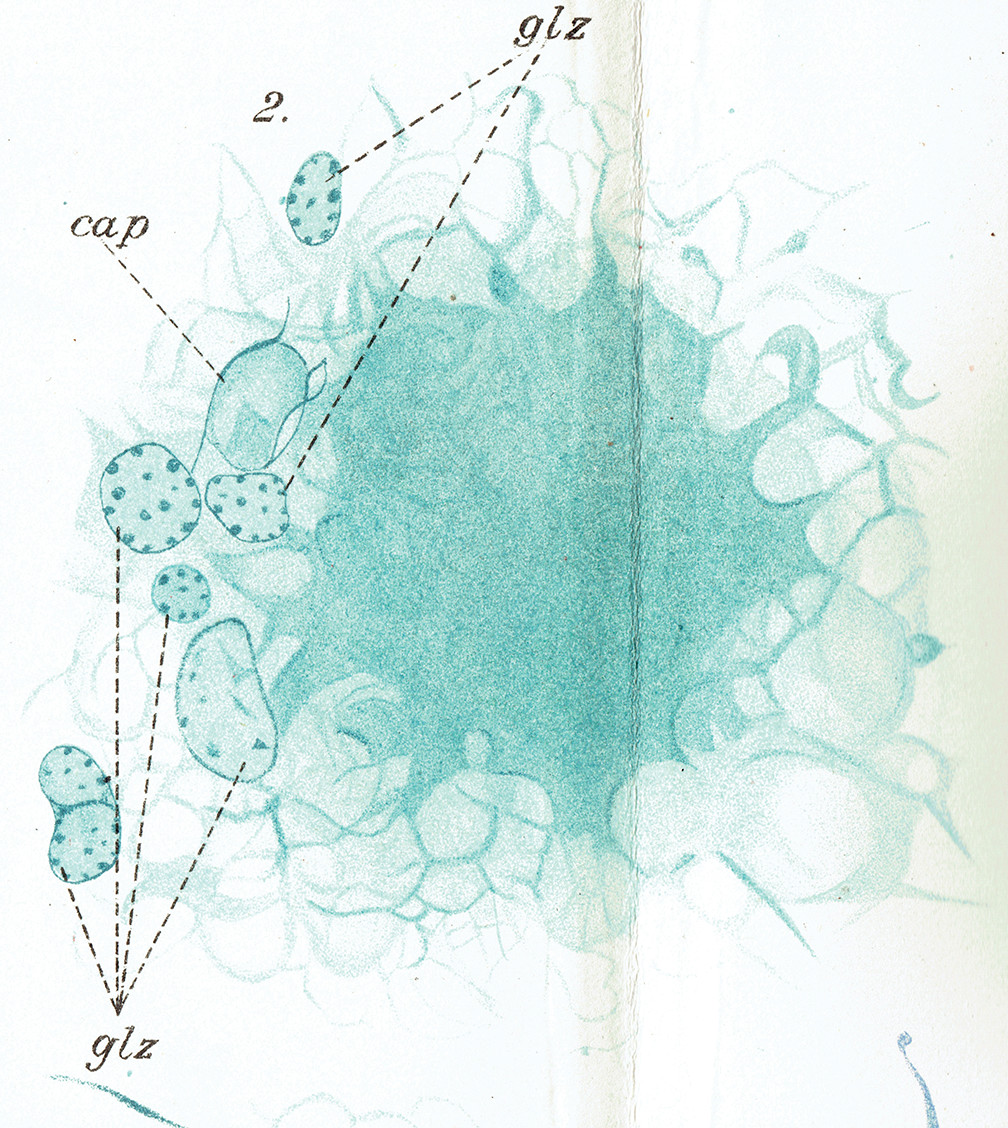
28Alzheimer’s case report built on the work of scientists, including those who created innovative fixation and staining techniques, advancements in microscopy, and a scientific climate that fostered curiosity. Alzheimer also asked Gaetano Perusini to examine the clinical reports and necropsy specimens of Auguste Deter and three additional patients. Perusini published detailed findings (
Figure 2) that cemented Alzheimer’s description of presenile dementia.
29,30In 1910, Emil Kraepelin introduced the term “Alzheimer’s presenile dementia” in his 8th edition of the
Handbook of Psychiatry. Kraepelin, who headed the Munich Royal Psychiatric Clinic in which Alzheimer was chief of neuropathology, may have named the disease for Alzheimer to differentiate it from the more common senile-onset dementias and to promulgate the idea of biological causes of mental illness. He also may have named this disease after Alois Alzheimer so as to assert his own department’s accomplishments over those of competing laboratories, such as that of Arnold Pick in Prague.
21 It would take decades for Alzheimer’s “unusual malady”
20 to become recognized as a common dementia.
Solomon Shereshevsky (S)
[I]t appeared that there was no limit either to the
capacity of S.’s memory or to the
durability of the traces he retained. —Alexander Luria
31
As a young scientist, Alexander Romanovitch Luria documented the exceptional memory and unusual personality of Solomon Shereshevsky in his 1968 publication,
The Mind of a Mnemonist: A Little Book about a Vast Memory.
31 This book was soon translated widely from the original Russian. The story of S. (as Luria called him), prompted renewed interest in the study of memory and also inspired journalists, filmmakers, and playwrights.
Solomon Veniaminovich Shereshevsky was born in the Russian village of Torzhok in 1896. At his father’s urging, Shereshevsky briefly attended music school with the goal of becoming a violinist, but a hearing impairment impeded his musical progress. Later, he worked as a newspaper reporter in Moscow.
Each morning the editor would meet with the staff and hand out assignments for the day.... The list of addresses and instructions was usually fairly long, and the editor noted with some surprise that S. never took notes. He was about to reproach the reporter for being inattentive when, at his urging, S. repeated the entire assignment word for word.
31
The editor suggested that Shereshevsky undergo psychological testing, and thus, at age 29, Shereshevsky met Luria who was 24 years old and just embarking upon his career in psychology. The two would work together for almost 30 years.
Luria’s initial impression was that Shereshevsky was “a rather disorganized and dull-witted person.”
31 Shereshevsky was puzzled as to why he had been sent for testing and had no awareness that his memory was different from anyone else’s. In fact, Shereshevsky’s memory proved exceptional. According to Luria, Shereshevsky could “easily remember any number of words and digits” and “equally easily he memorizes whole pages from books on any subject and in any language.”
32 He could accurately quote information from a decade earlier, including tables of numbers and strings of nonsense words. Luria turned from measuring S.’s memory capacity to studying how the presence of such a remarkably developed memory affected S.’s personality, behavior, and inner world. He devoted himself to “the study of
one man,” to learn all that he could from this “experiment of nature.”
31What Luria learned was that Shereshevsky’s memory differed from that of the vast majority of individuals; time did not erode his memories. Neither did a new stimulus affect his memory of an earlier one. In addition, his recall for the first item or the last item in a series was no better than his memory for other items on the list.
For memory tasks, Shershevsky relied primarily on visual imagery, augmented by synesthetic experiences. Anything Shereshevsky saw or heard reacted simultaneously with all of his senses… “to him any sound or thing has its own color, temperature, weight, shape and so on.”
32 For Shereshevsky, “there was no distinct line, as there is for others of us, separating vision from hearing, or hearing from a sense of touch or taste.”
31 Luria surmised that synesthetic perceptions were “a background for each recollection, furnishing him with additional, ‘extra’ information that would guarantee accurate recall.”
31If Shereshevsky were given a few moments between items he was to remember, each item would summon a vivid image. He could then mentally distribute these images along a street conjured in his mind. Later, even years later, he need only return to the route, beginning at either end, to find the images where he had left them. Shereshevsky’s performance at recall was not perfect, but his errors were, invariably because he had initially placed the image “in an area that was poorly lit or in a spot where he would have trouble distinguishing the object from the background against which it had been set…”
31 Thus, Luria noted that any omissions were errors of perception rather than of memory.
Shereshevsky’s visualizations allowed him to readily solve certain kinds of problems that others found difficult. However, his mode of experiencing the world also had its drawbacks. For example, Luria noted that “none of us have to deal with the problem of how to forget. In S.’s case, however, precisely the reverse was true.”
31 Also, if given a table of numbers that was generated by a simple rule, Shereshevsky would not notice the underlying principle, although, for others, this was what made memory of the numbers possible. Because each word conjured a unique and vivid set of sensations, Shershevsky was especially troubled by synonyms, double-entendres, or metaphors. Abstract ideas such as “infinity” or “nothing” perplexed him. “In order for me to grasp the meaning of a thing,” Shereshevsky said, “I have to see it.”
31Shereshevsky also became confused reading or listening to a story if he did not have sufficient time to register each word; the flood of synesthetic associations would obscure the storyline. He had to work at avoiding verbosity and sticking to the point in communicating the complexity of his experiences. He also had a poor memory for faces, as each expression would give rise to a multitude of sensory experiences.
Luria also noted that Shereshevsky’s experiences were so vivid that the line between imagination and reality was blurred. He could speed his pulse by picturing himself running to catch a train; he could raise the temperature in one hand while imagining touching a hot stove and simultaneously lower the temperature in the other hand by imagining holding an ice cube. Shereshevsky would feel confused when something did not turn out the way he had expected, so real had been his envisioning. Luria noted that Shereshevsky “gave himself up to dreaming... far more than to functioning in life.”
31Shereshevsky married, had one son, and worked in a variety of jobs, including: reporter, broker, vaudeville actor, efficiency expert, taxi driver, herbal therapist. He is best known for delighting public audiences with demonstrations of his remarkable memory and for being the subject of Luria’s important book. Solomon Shereshevsky died in Moscow in 1958 at the age of 62.
Importance
Shereshevsky’s exceptional mental capabilities stimulated interest in the neurobiology of memory and also in synesthesia. Luria’s description of S. is a reminder that superb cognitive abilities in one domain may come at the expense of another.
Luria applied the scientific method over an extended period of time. He asked colleagues to examine Shereshevsky independently; he preserved voluminous notes for examination by future scientists. Luria’s work was facilitated by his relationship to the Vygotsky school, an environment that supported careful inquiry.
Luria’s approach to the case method was itself a paradigm shift by virtue of the depth and length of his scientific study of Shereshevsky, the collaborative nature of their relationship, and the fact that Luria wrote his book for an audience that included nonprofessionals. In addition to cataloguing S.’s cognitive abilities, Luria looked at the human dimensions of his patient’s life and how S.’s exceptional visual memory and synesthesia affected his whole personality.
JP
[M]an cannot elaborate his social sense so that it can become part of his total self without “the great nerve net” of his frontal lobes. —Spafford Ackerly and Arthur Benton
33
In 1933, Spafford Ackerly, M.D., a psychiatrist at the University of Louisville, evaluated a 19-year-old boy (JP) who had been arrested for car theft. JP’s parents and lawyer were hoping that Dr. Ackerly could find mitigating circumstances that might keep the patient out of prison. JP had had a long history of stealing cars, but in a most peculiar fashion. Seeing keys in the ignition, he would take a car and drive in whichever direction it happened to be facing until it ran out of gasoline. Then he would abandon the car, find a telephone, and call his parents to pick him up.
JP was born in December of 1912, the 11.5-pound product of a normal pregnancy and gestation, followed by a 22-hour labor and a difficult delivery requiring instrumentation.
33 He developed normally through age 2. At 2 1/2, JP developed a tendency to wander blocks from home, entirely without fear. Often, he was returned to his parents by police. This behavior was undeterred by his father’s scolding or corporal punishment. JP’s wandering continued. During young adulthood he would travel thousands of miles, ascribing his meanderings to impulse.
34At age 4, JP fell off a bed and struck his head on the floor. About an hour later, he began to “say queer things,” and talk “like a smart alec.”
33 He then lost consciousness and, simultaneously, developed left-sided convulsive movements that abated spontaneously several hours later at the hospital just before he was to have had an exploratory craniotomy. By the next morning, reportedly, he was fully recovered.
33JP’s intelligence appeared normal. When he applied himself, JP apparently learned his school-work rapidly, though his reading skills far exceeded his arithmetic skills. However, his behavior in school was incorrigible. In second grade “he took a classmate’s glove and rubber, defecated in them, and replaced the glove in the child’s coat pocket.”
33 That same year, upon being caught after exposing himself to two little girls in the class, JP “denied it vigorously, saying haughtily, ‘I
beg your pardon, Sir!’” JP’s manners were described as “Chesterfieldian,” “distinguished by an over-politeness and a smooth ingratiating manner toward adults.” Even as a preschooler he appeared shallow and superficial.
33 JP was boastful, bossy, and unphased by the disdain in which he was held by his classmates.
33At age 13, after stealing money from a little girl and repeated episodes of masturbating in school, JP was transferred to the Day School for Defective Children which referred him to the Louisville Mental Hygiene Clinic for evaluation. His intake note included the following observations: “he has no friends; lies; steals; and is known in his neighborhood as having bad sex habits.”
33 JP attributed his social isolation to the malevolence of others. His IQ was measured at 92 on the Stanford-Binet, without inter-test scatter; his mother described his excellent memory for facts in the stories he’d read and the movies he’d seen. However, “his planning ability and capacity to modify behavior by experience” were described as “not equal to that of the average 7-year-old child.”
33During the ensuing 6 years JP was transferred to private, public and parochial schools, and finally to an out-of-state military school. There he stole a teacher’s car and served 2 years in reform school.
33 After his release, JP continued to wander widely and steal cars, his father making good on any damages and thereby helping him to avoid arrest. In 1933, at age 19, JP was arrested for yet another car theft.
32 This time he faced the possibility of prison, and the family lawyer arranged for him to see Dr. Ackerly.
The physicians who had previously evaluated JP believed that he was sociopathic. Ackerly, working with the neuropsychologist, Arthur Benton, noted that JP had a well-developed sense of right and wrong in the abstract or with regard to the actions of others, although JP’s own moral judgment was impaired and his behavior antisocial. Ackerly and Benton found JP to be irresponsible, impulsive, a spendthrift, completely free of anxiety, and unable to hold a job for more than a few months.
33He never holds a grudge nor speaks ill of anyone, never picks a fight, never tricks anyone….One is struck with the childish simplicity and superficiality of his petty lying and stealing and sex experiences which are unpremeditated. Yet these acts are never the result of pure impulse dissociated from their settings. Of all patients encountered he is by far the most stimulus bound….Everybody knows there is something radically wrong, but no one can put his finger on it.
35
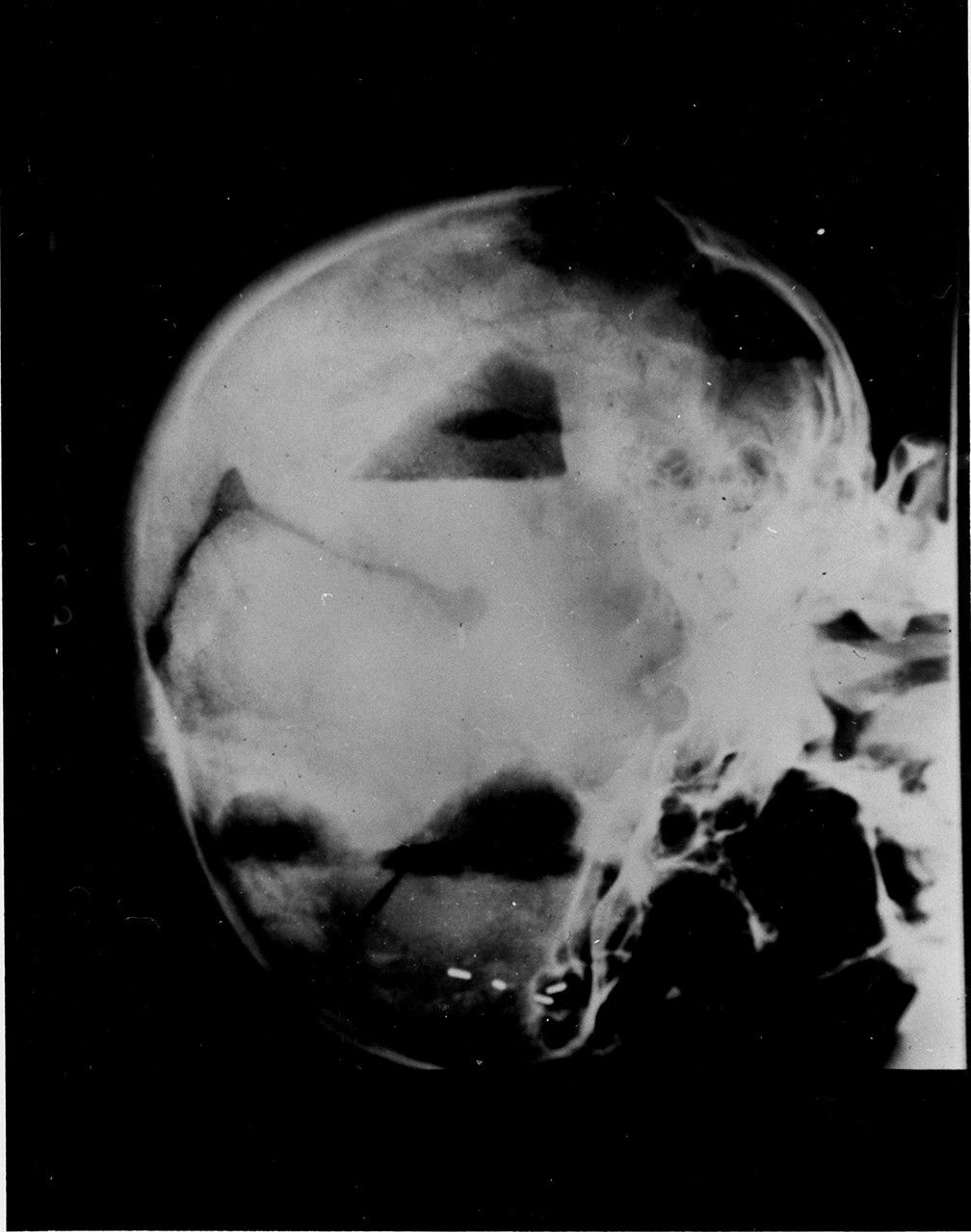
Ackerly’s evaluation of JP included a pneumoencephalogram in October 1933 (
Figure 3) that revealed severe bifrontal damage, thought to be consistent with an old brain abscess. Exploratory surgery confirmed that in the place of JP’s atrophic right prefrontal lobe there was a large arachnoid cyst and that bands of chronic arachnoiditis were compressing his left prefrontal cortex.
33 Although it was impossible to tell with certainty, Ackerly believed this damage to have been present from birth.
Ackerly continued to follow JP and published a follow-up report in 1964. He describes 50-year old JP as “the same refreshingly simple, uncomplicated, straightforward, outrageously boastful or indignant little boy.”
34 However, JP had gradually become unable to recall events as recently as five minutes in the past, the only exception being that he could retain anything having to do with automobiles, driving, and highway distances up to at least a day later. JP’s father had died 5 years earlier; JP remained at home, “lording it over his mother and taking no responsibility for helping out.”
34 He appears to have ceased his incessant wandering by that time.
Henry Gustav Molaison (HM)
Henry Gustav Molaison... left no survivors. He left a legacy in science that cannot be erased. —B.H.M. Carey
40
“HM” is arguably the single most intensively studied and best-described patient in the history of neuroscience. Henry Gustav Molaison unexpectedly developed a severe impairment in his ability to form new memories following bilateral medial temporal lobe surgical resection for intractable seizures in 1953, when he was 29 years old. Postoperatively, HM’s “loss was immediately apparent. … [T]his young man could no longer recognize the hospital staff nor find his way to the bathroom, and he seemed to recall nothing of the day-to-day events of his hospital life…. His early memories were apparently vivid and intact.
41HM, a high school graduate who worked as a motor winder, was hit by a bicycle as a child, sustaining a 5-minute loss of consciousness. There was a history of epilepsy in 3 paternal cousins.
41 At age 10, HM began to experience “minor” seizures; after age 16, “major” seizures developed. By 1953, despite escalating doses of anticonvulsants, HM was having up to 10 seizures daily, affecting his interictal mental functioning and his ability to work. In an effort to ameliorate HM’s epilepsy, William Beecher Scoville, a Hartford Connecticut neurosurgeon with a faculty position at Yale, bilaterally resected HM’s medial temporal lobes using a procedure he had developed, called “fractional undercutting.” This involved suctioning the medial temporal tissue extending 8–9 cm caudally from the temporal tips through bilateral supraorbital burr holes. Scoville, who later became the founding president of the International Society for Psychiatric Surgery,
42 had developed this procedure as a less destructive alternative to transorbital lobotomy.
43 Unilateral medial temporal resection for treatment of intractable epilepsy had been pioneered by Wilder Penfield at the Montreal Neurological Institute (MNI) in 1928.
44 However, applying bilateral “fractional undercutting” to the treatment of HM’s seizures in 1953 was, according to Scoville, “frankly experimental.”
41Although HM’s epilepsy did improve and his postoperative neurological examination was reportedly normal, Scoville noted “one striking and totally unexpected behavioural result”—HM’s remarkable loss of ability to form new memories.
41 Scoville first reported this surgical result in April 1953 in a speech at the Harvey Cushing Society. His talk was published in 1954 as “The Limbic Lobe in Man” and included mention of
“a very grave, recent memory loss” in two patients “undergoing bilateral resection of the entire [limbic lobe] complex including the hippocampal gyrus extending posteriorly for a length of 8–9 cm from the tips of the temporal lobes.”
45 One of these patients was HM.
Around this time, Penfield noted two of his patients had become severely amnestic following
unilateral, left medial partial temporal lobectomy for refractory epilepsy.
46 These two patients were presented at the 1955 meeting of the American Neurological Association. Their surgical outcome had been entirely unexpected as it was in contradistinction to at least eighty other similar procedures that did not result in memory loss. After the meeting, Scoville called Penfield to tell him about HM. Penfield consulted with MNI neuropsychologist Brenda Milner, who began a career-long study of HM beginning 2 years after HM’s surgery.
47In April 1955, when Milner first examined HM, he still believed the year to be 1953 (the year of his operation), and he had no recollection of the conversation he had had with Milner immediately prior to entering the interview room. Milner found that HM’s IQ had actually increased by eight points to 112 on the Wechsler-Bellevue scale in comparison to postoperative testing; this improvement was thought to have been a consequence of HM being “less drowsy” because he was having fewer seizures. HM displayed a complete loss of memory for events since his surgery, partial retrograde amnesia for the 3 years before the procedure, and remarkably intact early memories.
41In their seminal paper, Scoville and Milner reported 10 temporal lobectomy patients one year after surgery, one of whom was HM. Two of their patients had no demonstrable memory impairment, five had moderate memory loss, and three, including HM, exhibited severe anterograde amnesia.
41 All but one of the patients had undergone bilateral surgery, eight for treatment of psychotic conditions. The other two patients in the severe category had the surgery performed for treatment of paranoid schizophrenia and manic depressive disorder. What made HM unique was that his mental status findings were “restricted to his inability to remember new episodic, autobiographical events and not confounded by other neurological or psychological disorders.”
48In light of earlier reports that unilateral lesions had no impact on memory, Scoville and Milner concluded that bilateral lesions produce “persistent impairment of recent memory whenever the removal is carried far enough posteriorly to damage portions of the anterior hippocampus and hippocampal gyrus.” “The degree of memory loss appears to depend on the extent of hippocampal removal.” The authors added the caveat that, since the uncus and the amygdala were always removed along with the hippocampal complex, they could not rule out the contributions of these areas to “retention of current experience.”
41In 1958, a little more than a year after the Scoville and Milner paper, Penfield and Milner published the two cases of unilateral left partial temporal lobectomy they had presented in 1955. Both patients had developed severe anterograde amnesia similar to that of HM. Penfield and Milner postulated that these two patients were unique in having had unrecognized, pre-existing, right-sided hippocampal lesions, causing the severe anterograde amnesia produced by bilateral hippocampectomy.
46 Postmortem examination of one of their patients in 1964 confirmed the presence of right hippocampal sclerosis that had been unrecognized prior to the left-sided surgery.
49Importance
Prior to studies of HM, memory was believed to be a widely distributed function, associated with, rather than separate from, other cognitive and perceptual abilities. The function of the hippocampal formation was unclear, having been suspected of having roles in motor, olfactory or emotional function.
50 HM’s case illustrated the importance of the medial temporal lobes for memory. Contrary to popular interpretation, HM’s case alone did not prove that bilateral hippocampectomy resulted in complete anterograde amnesia, since the amygdalae were also removed. However, when HM was considered with their two aforementioned unilateral hippocampectomy cases, Penfield and Milner were able to conclude that removal of the hippocampi bilaterally does, in fact, result in anterograde amnesia.
46HM was the most important patient in modern memory research. As many as 100 investigators examined and tested him, first at the MNI, and later at the Massachusetts Institute of Technology laboratory of Suzanne Corkin. Corkin, a student of Milner, had met HM in Milner’s laboratory in 1962. HM’s willingness to participate in innumerable studies during the 55 years between his surgery and his death in 2008, confirmed the role of the hippocampus in memory formation and revealed that memory is not a unitary function.
Despite having no recall of having learned a motor task, nevertheless his performance of complex motor skills improved with repetition, establishing that procedural memory relied on different brain networks than did declarative memory. In addition, HM could retain information as long as his attention to a task was sustained by continual mental rehearsal, establishing that working memory involved extrahippocampal areas.
HM also agreed to have his brain preserved for further study after his death. An extremely detailed postmortem examination of HM’s brain showed that he had approximately 2 cm
3 of retained hippocampal tissue bilaterally, so the surgical resections were not complete.
51 At the time of this writing, research projects using tissue from HM’s brain are being coordinated by David Amaral at the UC Davis MIND Institute.
52