Up to one-third of people who sustain a mild traumatic brain injury (mTBI) develop persistent symptoms, such as fatigue, headaches, and memory or concentration problems (
1–
5). Persistent symptoms after mTBI are not likely caused by mTBI alone (
6). Risk factors for persistent symptoms include preinjury or comorbid psychiatric disorders as well as maladaptive psychological coping (
7–
11). Interpersonal factors, such as the quantity and quality of relationships and the positive and negative aspects of these relationships, may also influence mTBI outcomes (
11,
12).
Attachment theory suggests that early experiences with caregivers predict how people feel and interact in close relationships across the lifespan (
13–
15). Insecure attachment is characterized by high attachment anxiety (i.e., discomfort separating from an attachment figure), high attachment avoidance (i.e., discomfort being too dependent on that figure), or both. Interpersonal challenges may arise throughout the lifespan because of insecure attachment, especially in stressful or threatening circumstances (
16). After mTBI, individuals with high attachment anxiety may be overly reliant on others and experience emotional distress when their attachment needs cannot be met. Individuals with high attachment avoidance may become increasingly self-reliant, preventing them from receiving the support and care they need as they recover.
Although mTBI is often experienced as distressing and threatening (
17), it has been scarcely studied as a potential trigger of insecure attachment strategies. Only one prior study has investigated the relationship between persistent symptoms and attachment after mTBI, through a cross-sectional survey (N=973) of Danish people 3–9 months after mTBI (
18). The authors found that attachment anxiety was associated with persistent symptom severity among people with high attachment avoidance and that attachment avoidance was associated with persistent symptom severity, regardless of attachment anxiety levels. Severity of persistent symptoms was highest among participants with high scores on both attachment dimensions (i.e., paradoxically, being afraid of both dependence and autonomy) (
18). Limitations of this study included a low survey response rate (39%), restricted age range (ages 15–30), and consideration of a single clinical outcome—reported persistent symptoms (
18).
Attachment strategies have been studied in relation to health conditions that share clinical features with persistent symptoms after mTBI. In individuals with functional neurological disorder, higher scores for both insecure attachment dimensions were associated with greater symptom severity, depression, and anxiety, whereas secure attachment style was associated with better symptom improvements after treatment (
19,
20). In individuals with chronic pain, a condition with clinical features that resemble persistent symptoms after mTBI (
21), both insecure attachment strategies were associated with the presence and severity of chronic pain and with worse depression (
22–
24). In summary, evidence from studies of related health conditions suggests that attachment may possibly be related not only to persistent symptoms after mTBI but also to a range of other outcomes, including psychological functioning, health-related quality of life (HRQOL), and treatment response among people with mTBI. The aim of the present study was to directly test this hypothesis.
Based on attachment theory and prior research, we hypothesized that insecure attachment strategies (higher level of attachment anxiety or avoidance) would be associated with more severe persistent symptoms, worse HRQOL, and worse psychological functioning (i.e., higher levels of depression and anxiety) after mTBI. Moreover, we hypothesized that insecure attachment strategies would be associated with worse treatment responses (i.e., smaller reductions in persistent symptoms and mental health symptoms and less improvement in HRQOL over a preceding course of treatment).
Results
Table 1 displays the sample characteristics and descriptive statistics for the predictor and outcome measures. Generalized linear modeling results are presented in
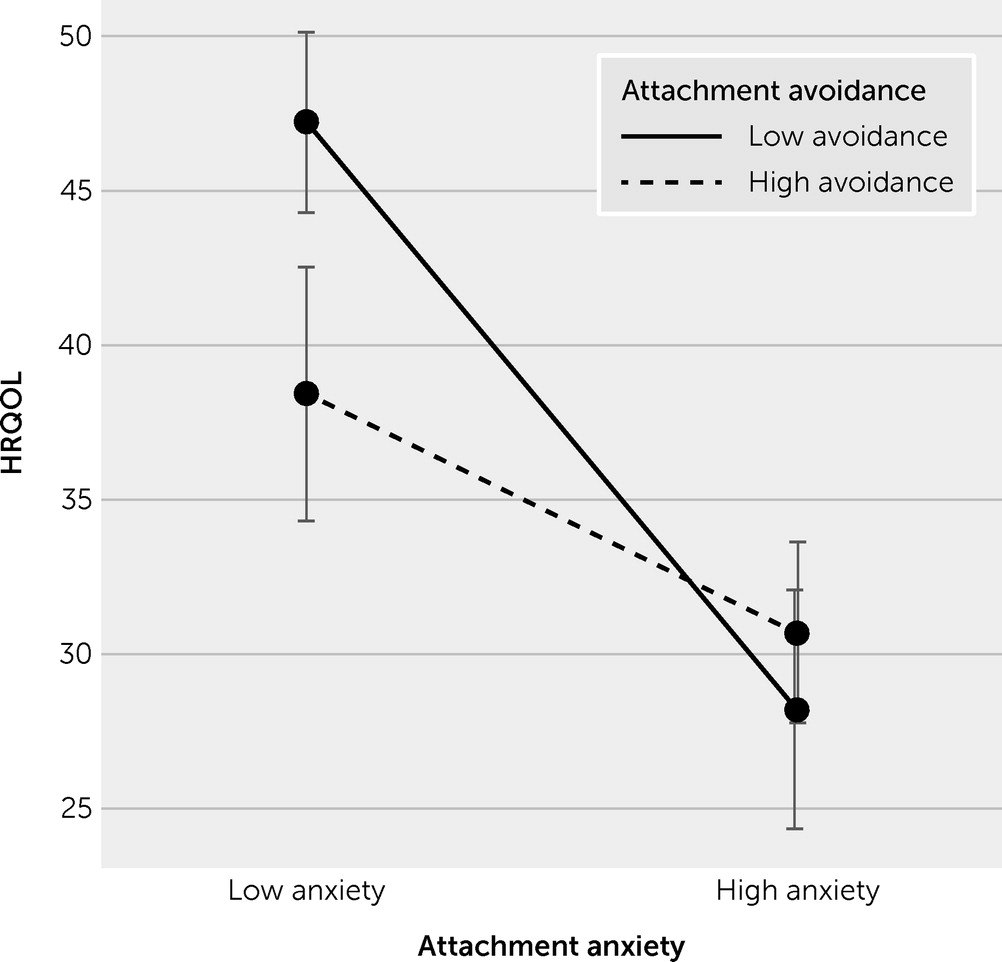
Table 2. Higher attachment anxiety was associated with greater persistent symptom severity (B=3.65, 95% CI=0.66 to 6.64, p=0.017), greater symptoms of depression and anxiety (B=0.36, 95% CI=0.11 to 0.61, p=0.004; B=0.38, 95% CI=0.09 to 0.68, p=0.011), and worse HRQOL (B=−9.49, 95% CI=−14.22 to −4.75, p<0.001) at follow-up. Higher attachment anxiety was also associated with less improvement in depression (B=−1.12, 95% CI=−2.30 to −0.09, p=0.033) and HRQOL (B=−6.37, 95% CI=−10.27 to −2.47, p=0.001) from clinic intake to follow-up. In contrast, attachment avoidance was not significantly related to any of the clinical outcomes. Interaction effects between attachment anxiety and avoidance were nonsignificant, except for HRQOL (B=5.50, 95% CI=0.98 to 10.02, p=0.017), in which high attachment avoidance was associated with lower HRQOL among participants with low attachment anxiety (
Figure 1). No significant changes were found in the results after we included gender and group conditions as covariates.
Discussion
The current study investigated the relationship between attachment and a range of clinical outcomes among treatment-seeking adults with mTBI. We hypothesized that participants with insecure attachment strategies (higher level of attachment anxiety, attachment avoidance, or both) would report more severe persistent symptoms, lower HRQOL, lower psychological functioning, and worse treatment outcomes (i.e., less improvement on all outcome measures over the preceding months) after mTBI. Our findings partially supported these hypotheses. We found significant associations between attachment anxiety and persistent symptoms, depression and anxiety symptoms, and HRQOL 4–5 months after mTBI. Higher attachment anxiety was also associated with less improvement in depression and HRQOL during the active treatment phase, from clinic intake to follow-up. Attachment avoidance was largely unrelated to clinical outcomes from mTBI in this study. The one exception was that high attachment avoidance was associated with lower HRQOL among participants with low attachment anxiety, whereas those with high attachment anxiety had lower HRQOL regardless of attachment avoidance levels. Our results suggest that attachment anxiety, the fear that a significant other will not be available in stressful circumstances, has a greater association with clinical outcomes and recovery among adults with persistent symptoms after mTBI than does attachment avoidance.
Theoretical frameworks have proposed that insecure attachment leads to interpersonal dysfunction and poor health (
12,
22), but the present study design did not allow us to draw causal conclusions. The mechanisms through which insecure attachment might interfere with recovery from mTBI were also not clear. Hyperactivation of the attachment system among individuals with high attachment anxiety may be associated with affect regulation difficulties (
22,
37). Psychological distress can amplify the severity of persistent symptoms, in part because physical symptoms of sympathetic nervous arousal overlap with persistent symptoms and can be misattributed to mTBI (
38,
39). In other words, psychological distress may be both an outcome of insecure attachment and a mediator through which insecure attachment worsens persistent symptoms after mTBI. Being overly reliant on others may also prevent opportunities for people with mTBI to resume their preinjury responsibilities and experience success, updating their beliefs about their capabilities as they recover. In contrast, attachment avoidance, the discomfort of being too dependent on others, may manifest as an underreporting of symptoms (
22). The capacity of attachment avoidance to provoke the repetitive cycle of enduring activity-related exacerbations of persistent symptoms and then “crashing” with prolonged rest may disrupt daily functioning and HRQOL after mTBI (
9). Further research is needed to evaluate this tentative model.
Our findings add to the literature linking insecure attachment to adverse health outcomes (
22,
40–
43) by demonstrating this association in the context of mTBI. Our findings add nuance to the only prior study of attachment in the context of mTBI (
18), which similarly found that insecure attachment was associated with persistent symptoms after mTBI, but the pattern and relative strength of attachment anxiety and avoidance dimensions differed. That study was large but cross-sectional, included only participants ages 15–30, and considered only severity of persistent symptoms (
18). The present study extends Tuborgh et al. (
18) by assessing a range of different clinical outcomes, including persistent symptoms, depression, anxiety, and HRQOL as well as changes in these measures during the active treatment phase after mTBI across adulthood. Compared with participants in the Tuborgh et al. study, our participants were older, more symptomatic, and seeking specialty outpatient treatment for mTBI. These sampling differences may have contributed to the subtle between-study discrepancies.
This study had several limitations. First, although attachment strategies are quite stable across the lifespan (
14), it remains possible that the experience of mTBI with protracted recovery increased insecure attachment. For example, a recent study suggested that greater mTBI symptoms were related to decreases in relationship satisfaction 1 month postinjury (
44). We tested this assumption in exploratory analyses and found that participants with greater injury severity (indexed by the presence of witnessed loss of consciousness) reported significantly higher attachment avoidance (M±SD=2.60±0.87) than those with no loss of consciousness (M±SD=2.03±0.79; t=2.27, df=81, p=0.026, d=0.71). Associations of the presence or absence of loss of consciousness with attachment anxiety and persistent symptom severity were not statistically significant, but the effect sizes were not trivial. These post-hoc analyses suggest that the attachment system, particularly avoidance strategies, might be influenced by mTBI. Thus, it is tenuous to assume that the RSQ measured only “premorbid” attachment strategies in this study. Second, we measured attachment strategies with a self-report measure (RSQ) that queries about relationships in general. Attachment is dyadic and may be specific to relationships with certain people (
45). Evidence of weak correlations between self-report attachment strategies and dyadic assessment of attachment (i.e., narrative interviews or coding of observations) has also been reported. Third, self-reported outcome measures such as the RPQ are clinically meaningful but cannot provide a complete picture of recovery from mTBI. A multimodal outcome assessment that included objective measures of cognition and vestibular-oculomotor function, for example, would have been preferable. Fourth, we had a relatively small sample size that may have resulted in insufficient power to detect additional interaction effects and associations with changes over time. Fifth, our participants may have had more clinical care than is typical at other mTBI clinics. This discrepancy may influence the generalizability of the results, especially our analyses involving change during the study observation period. However, the usual care and experimental interventions our participants received are not outside the wide range of offerings at other mTBI clinics with regard to the number and types of providers involved as well as the content and aims of the intervention (
46–
48). Despite these limitations, the current study was the first to assess the relationships between attachment strategies and a comprehensive set of clinical outcomes (i.e., persistent symptoms, depression and anxiety symptoms, and HRQOL) after mTBI and over a period of outpatient treatment.