The COVID-19 pandemic taught us many lessons, including the interconnection between physical and mental health. This observation is not new, however; the intersection of physical and mental health is discussed in early medical writings. At the origins of modern-day psychiatry and neurology, there was great interest in the condition now called functional neurological disorder (FND) (
1,
2). Nonetheless, FND has a complex history, including its evolution from “hysteria” to “conversion” to “psychogenic illness” to “FND”; unfortunately, the condition is also stigmatized and erroneously confused with malingering (
3). The recognition that FND is common, an emphasis on a rule-in diagnosis, an improved understanding of mechanisms and etiologies, and an expanding therapeutic toolkit have revitalized the field of FND (
4). However, disagreements remain, such as the multiplicity of terms used for the seizure subtype of FND (e.g., psychogenic nonepileptic vs. functional vs. dissociative vs. nonepileptic attacks) (
5); to unambiguously connect all functional neurological subtypes to FND, we support use of the term “functional seizures.”
In other specialties, similar transformations have moved away from “medically unexplained” framings. Although certain disciplines have used the qualifier “functional” and this term is well received by some patients and advocacy groups, challenges to a “functional disorders” diagnostic category remain (
6). The term “functional gastrointestinal disorders” was changed to “disorders of gut-brain interaction,” in part because “functional” was thought to be too nonspecific (
7). The somatic symptom disorder diagnosis has received mixed reviews, and competing terms, such as bodily distress disorders, have arisen (
8). These developments have weakened the DSM-5’s “Somatic Symptom and Related Disorders” category. In parallel, the medical literature has codified functional somatic syndromes (e.g., fibromyalgia) with their own diagnostic criteria. Some conditions have been reframed to potentially distance them from a biopsychosocial-informed therapeutic framework (e.g., myalgic encephalomyelitis or chronic fatigue syndrome); conversely, there have been calls to reconceptualize persistent symptoms after mild traumatic brain injury (also known as postconcussive symptoms or postconcussion syndrome) as an “interface disorder of neurology, psychiatry, and psychology” (
9).
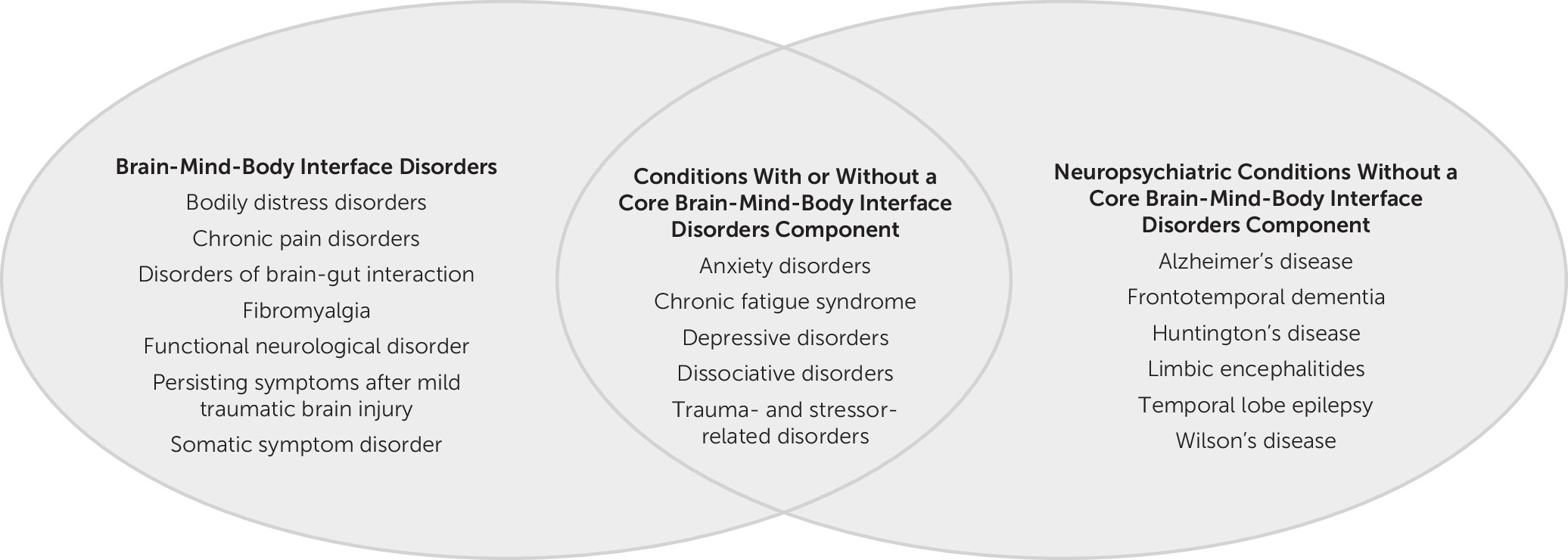
Here, we make the case for a “brain-mind-body interface disorders” diagnostic category spanning medical specialties; this category represents conditions with physical symptoms where there is likely a therapeutic benefit to factor in psychological processes (e.g., biased attention, fear avoidance, somatic hypervigilance, illness beliefs, alexithymia, catastrophizing, impaired self-agency, and dissociation) as core to the development or maintenance of symptoms (
Figure 1) (
10,
11).
Helping Patients Understand the Diagnosis and Engage With Treatments
Communication of and a general receptiveness to the diagnosis of a condition in this category by patients and family members are critical steps in treatment. For a conversation about the diagnosis to be comprehensive, in our opinion, the intersection of brain, mind, and physical symptoms should be addressed—a “functional disorder” framework without further clarification does not explicitly identify this relationship. With a given diagnosis falling into the brain-mind-body interface disorders category, providers can introduce the notion that a particular condition sits at the interface of brain, mind, and body—a concept that challenges sociocultural norms of health and disease. It is important to validate the patient’s symptoms as genuine and common while facilitating a transition to a repertoire of complementary physical (e.g., physiotherapy) and mental health (e.g., psychotherapy) treatments. Recognizing that brain-mind-body interface disorders exist on a spectrum is essential to understanding why some patients will improve with treatments primarily targeting physical health, whereas others may benefit from mental health interventions. Importantly, physical health interventions, such as physiotherapy, are psychologically informed when applied to patients with brain-mind-body interface disorders (
12).
Increasing Access to Care
Brain-mind-body interface disorders lack a medical home, with disagreements among clinicians and patients alike regarding whether the condition is “physical,” “psychological,” or both. Although the relevance of medical and neurological, psychiatric and psychological, and sociocultural-spiritual factors varies across individuals based on their biopsychosocial-informed “personal equation” for the development and maintenance of their condition, a defining characteristic of brain-mind-body interface disorders is a nuanced, and at times overt, interplay between one’s physical and mental health. As such, a diagnostic category that goes across specialities should facilitate team-based (multidisciplinary and interdisciplinary) care in this patient population. Also, a term that helps eradicate dualistic thinking (e.g., “organic” vs. “nonorganic”) offers advantages in promoting a patient-centered approach from the start (
13). Neuroscientifically, structure-function relationships are closely coupled, suggesting that functional disorders are essentially also structural disorders, with the distinction being one of scale (macro vs. micro).
Connecting to the Broader Diagnostic Category
The naming of a condition—fraught with a multiplicity of considerations—occurs through an interplay between scientific advances, professional and patient advocacy organizations, and funding bodies. The brain-mind-body interface disorders framework allows inclusion of a range of conditions cared for across specialties (e.g., noncardiac chest pain) whether or not those conditions are explicitly identified with the qualifier “functional.” The identity of each disorder can be preserved, along with the acknowledgment of a connection with other brain-mind-body interface disorders. This approach also offers the advantage of bringing together different organizations for shared advocacy (e.g., interdisciplinary research and programmatic funding). Furthermore, the term “functional disorders” is not universally synonymous with brain-mind-body interface disorders (e.g., functional disorders of the gallbladder). Similarly, functional medicine is a medical specialty that is not specifically related to the care of functional disorders.
Cohesively Framing Incompletely Understood Mechanisms and Etiologies
Brain-mind-body interface disorders are etiologically and mechanistically heterogeneous. For example, childhood maltreatment is a risk factor for FND and somatic symptom disorders, yet not all individuals with these conditions endorse adverse life experiences (
14). For others, risk factors or triggers for these disorders may relate to perfectionistic traits, physical injury (drawing attention to the body), pathological health anxiety, sensory processing difficulties, autism spectrum disorder, or intellectual disability, among other possibilities (
15).
Reducing Iatrogenic Harm
Another challenge is to identify a diagnostic category that proves validating and therapeutically helpful while providing the health care system with an understanding of the scope of a given patient’s symptom complex. For individuals with a brain-mind-body interface disorder, the symptoms attached to a specific diagnostic label must be clearly specified. Excessive (or premature) diagnostic anchoring of new symptoms without an appropriate workup is fraught with potential medical errors. This issue is likely relevant to whatever term is reached through consensus, underscoring the need for more education.
Conclusion
In summary, we call for operationalizing a brain-mind-body interface disorders diagnostic category, given its transparency in highlighting the interplay between the brain, mind, and body that is likely therapeutically (and mechanistically) foundational to these conditions. Surveying a range of stakeholders will be important because such terminological considerations have important medical and societal implications.