Learning about neuroanatomy is a prerequisite in medical curricula (
3). Digital forms of neuroanatomy education, including three-dimensional (3D) image reconstruction of the human brain with artificial intelligence (AI) and 3D printing, are often incorporated to approach the challenges of studying the human brain and other complex anatomical organs (
3–
6). The rapid development of digital technologies in medical education opens new opportunities, facilitating advances to overcome ethical limitations, technological variations, and geographic or diversity barriers (
5,
7). Some medical schools are experiencing limited accessibility to fresh cadaveric specimens and prosections (i.e., plastinates) due to economic, religious, and legal issues (
8). In current medical curricula, clinical training in anatomy is shifting toward a digital focus, adopting metaverse technologies and innovative teaching and learning strategies (
4,
7,
9). The new technology-assisted methods can increase interactions among users (e.g., teachers and learners) in varied learning modes (e.g., synchronous or asynchronous and live or remote). These methods can enhance educational context and engagement, thereby resulting in greater benefits for educators and learners (
7).
Although many metaverse educational platforms (e.g., virtual and augmented realities) have been available for more than a decade, some educators may be unaware of how these disruptive technologies are using imaging to transform medical education pedagogies and clinical training (
7,
10,
11). However, during the COVID-19 pandemic and thereafter, the use of technology to deliver clinical training in anatomy has significantly increased (
7). In addition, the use of metaverse innovations has expanded within health care settings, including neurology and neuropsychiatry (
12–
14). Virtual health care platforms (i.e., where health practitioners and patients interact digitally in real time) are anticipated to become a quarter-trillion-dollar industry, with neurology and psychiatry at the vanguard of care delivery (
15).
Processing of 3D Clinical Images and 3D Printing
The use of two-dimensional image data sets (e.g., data from computed tomography and MRI) viewed on flat computer screens to study anatomy and its subdisciplines has limitations (
2). In traditional medical curricula, a comprehensive understanding of human body structure requires many hours of laboratory training with cadaveric specimens and anatomically relevant 3D plastic models (
16). The expected outcome is that trainees will develop core competencies and further enhance their skills in performing effective physical (i.e., neurological) examinations and in applying other clinical and diagnostic skills in patient care (
1,
17).
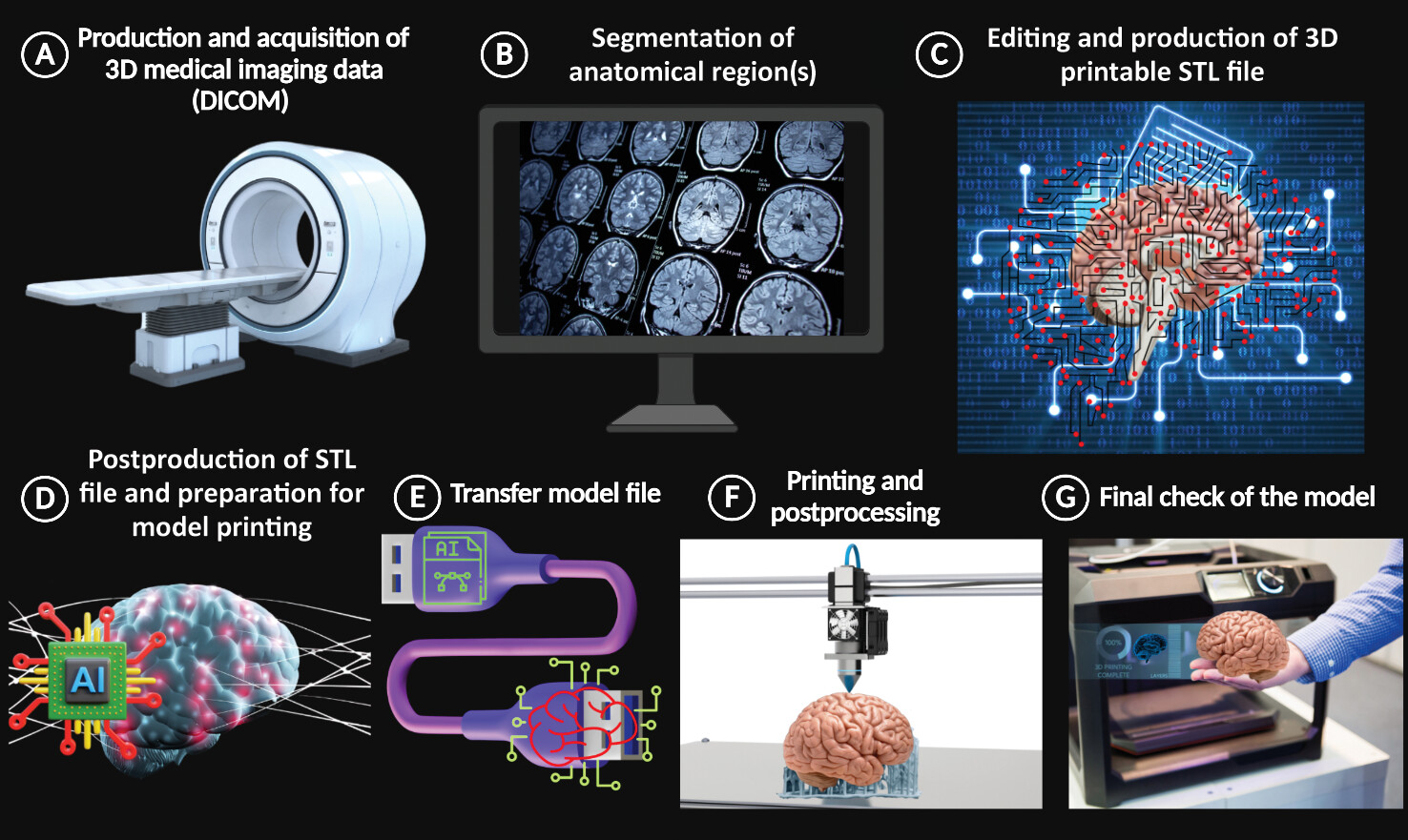
Three-dimensional computer-assisted design reconstructions of digital images allow virtual 3D reconstruction of medical images of any anatomical region (
18). In 2018, the Radiological Society of North America 3D Printing Special Interest Group recommended important regulatory guidelines and suggested relevant imaging parameters (
19). Digital images can be processed for segmentation and rendering of anatomical details, and then the data can be transferred to a 3D printing format by using artificial intelligence (AI) software to produce anatomical replicas (
Figure 1) (
1,
6,
20). Recent developments in AI indicate its potential for improving education regarding clinical anatomy. In particular, these innovations can foster allocation of specific technological resources to individual learners and trainees, adapted to match their personal skills and learning needs (i.e., precision education) (
11).
The first 3D printing technology (also known as additive manufacturing) was introduced by Charles Hull in 1986 (
6). This technology describes the process by which a computer-generated 3D model is rendered into a physical object (
21). There are many applications of 3D printing in medical education and training, clinical research, and health care. Nevertheless, some legal and safety guidelines should be considered regarding the intended use of 3D-printed models, specifically if they are classified as medical products (e.g., surgical instruments, clinical devices, and medical implants) (
22). Because 3D-printed anatomical models for medical education are not classified as medical products, they are not regulated (
1,
23).
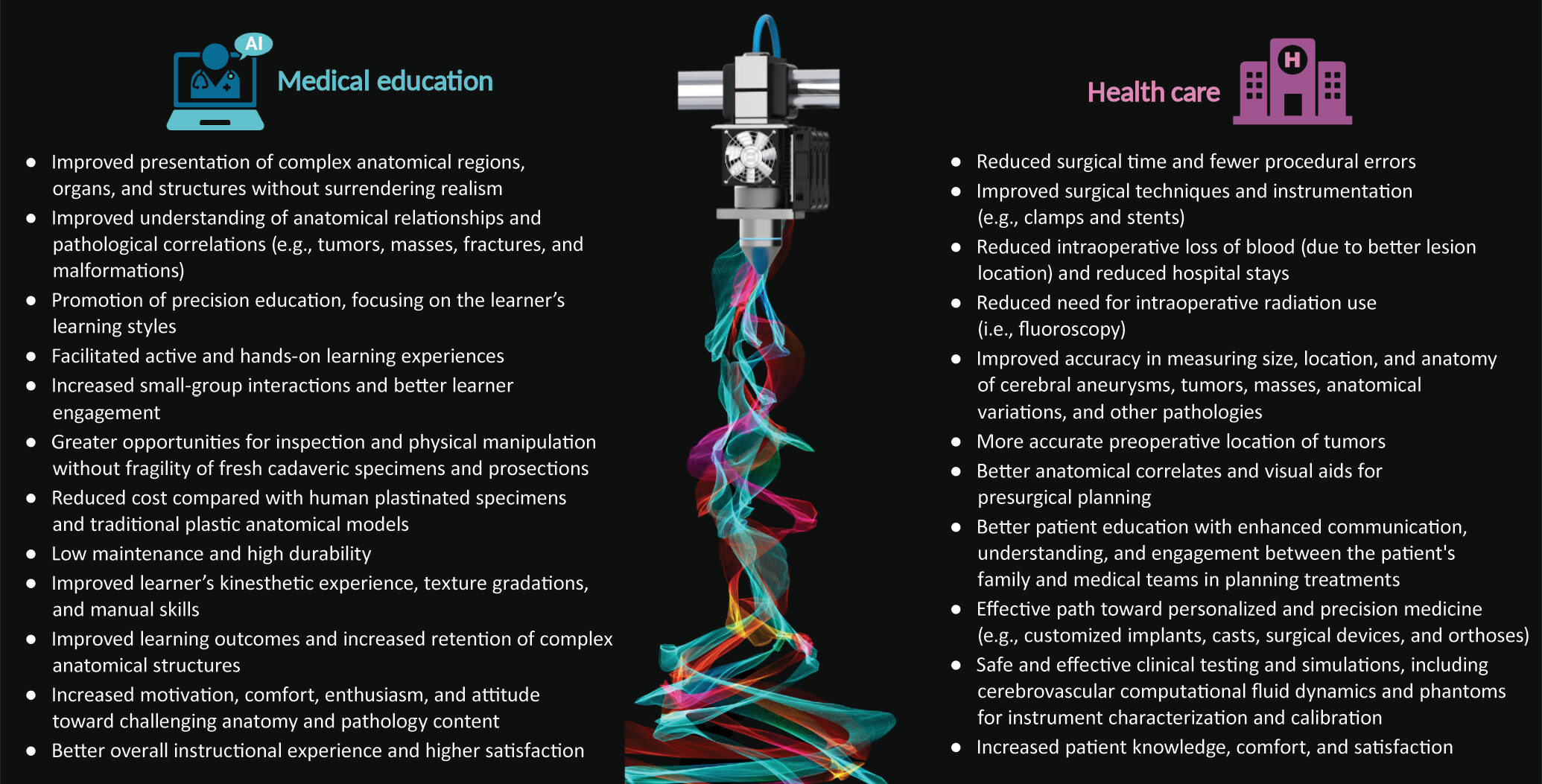
The use of 3D human replicas can enhance teaching clinical anatomy and facilitate understanding of complex anatomic structures (
1,
8,
24). For example, these replicas are useful in the assessment of anatomical and pathological relationships (e.g., masses, tumors, fractures, and malformations). In addition, such replicas have great potential for hands-on clinical training (i.e., individualized simulation of interventions) and precision education (
1,
8,
11,
25).
The challenges of training students with fresh specimens and cadaveric prosections include the fragility of these materials. Learners often refrain from performing examinations that require further physical manipulation to avoid damaging the highly detailed prosections (
8). The use of 3D-printed models eliminates such concerns, thereby improving learners’ kinesthetic experience, interaction, and overall engagement. Methods incorporating 3D-printed models eventually result in better learning outcomes, improving students’ retention of anatomical concepts (
Figure 2) (
1,
8).
In health care settings, 3D imaging and 3D-printed surgical models for diagnosis and procedure planning have transformed the surgeon’s decision-making process regarding the use of specific techniques (
6). These 3D-printed devices can also be useful as surgical guides for arthroplasty procedures and customized casts and for patient education, development of medical devices (e.g., clamps and stents), and presurgical pressure testing of intracerebral blood vessels (
1).
In the context of neurosurgery and clinical neuroscience, 3D-printed replicas of cerebral arteriovenous malformations can be used for preoperative education of patients, clinical staff training, and improved surgical planning (
8). Phantom models of the brain vasculature printed from medical images can provide valuable information regarding the flow properties of the intracerebral vascular system. These replicas open up new opportunities in clinical research for assessing cerebrovascular computational fluid dynamics and designing suitable simulations (
20). Overall, 3D-printed models have increased the efficacy of medical procedures, provided new opportunities for precision medicine, and improved comfort and satisfaction of patients (
Figure 2) (
1,
2,
20,
25,
26).
Despite the advantages of medical 3D printing, there are important challenges and considerations associated with this technology. For example, the cost of high-quality 3D printers is important to consider (
1). In 2019, the American Medical Association and the U.S. Food and Drug Administration issued temporary approval for 3D-printed models in current procedural terminology (CPT) codes (i.e., category III CPT codes), permitting the reimbursement for use of 3D-printed anatomical models and surgical implants for an introductory period of 5 years (
23,
27). In addition, onsite 3D printing is becoming affordable for research, education, treatment planning, and medical simulations (
1). A recent study by Nilsson et al. demonstrated that developing a full-scale 3D phantom model from a patient’s computed tomography scan was efficient and low cost (
20).
Other important considerations are the type of printer and printing materials (e.g., plastic polymers, metals, and resin). There is an extensive selection of 3D printing devices and alloys to suit specific needs and purposes. Thus, users should choose the 3D printers and printing materials that best suit their needs (
1). Users must also realize that there are specific occupational health and environmental safety considerations for storage, handling, and proper disposal of toxic printing materials (
28). Some of the chemicals in these materials (or their vapors) may be harmful for personnel and the environment (
1,
28).
Finally, 3D printing requires trained personnel. Printing specialists with in-depth knowledge of this technique may be essential for onsite printing and external consultation services (
1).
Conclusions and Future Directions
Three-dimensional printing is an AI-potentiated technology that is rapidly emerging along with other metaverse innovations. This technology provides substantial advances in medical education, clinical training, and health care, promising significant benefits for precision medical education and personalized medicine. Therefore, the demand for better 3D printers, printing materials, and expertise is anticipated to increase accordingly.
In medical curricula, there is an imminent digital technology–based transformation (e.g., AI and digital imaging). Digital technologies improve learning by allowing a focus on the specific learning styles and needs of learners (i.e., precision education). Currently, 3D printing alone cannot replace the use of cadaveric specimens during medical training. However, this emerging technology is rapidly becoming an innovative supplemental component for teaching clinical neuroscience and other medical disciplines.
Importantly, 3D printing can be integrated into current forms of medical pedagogy. For example, learners (i.e., small groups) could engage in a highly dynamic and creative learning activity, such as designing an original 3D printing project (e.g., a localized intracerebral aneurysm). This project could be part of a module where the learners would be actively involved from the initiation of digital imaging and communications (DICOM) image acquisition throughout the 3D printing process (
Figure 1). This would be a step forward for precision education in medical curricula. Contemporary medical education programs could foster advanced skills in anatomy that learners and trainees can extrapolate to clinical imaging relevant to different specialties, resulting in more accurate diagnoses.
In health care, 3D-printed models of patient anatomy seem to increase certainty in clinical decision making, improve the efficacy of medical procedures, and allow the fabrication of patient-specific implants that create anatomically correct and aesthetically pleasing artificial body structures. However, it is imperative to standardize the practice of 3D printing in terms of accuracy, reproducibility, and intellectual property protection and to create appropriate guidelines, regulations, and specific quality-control criteria by regulatory agencies. In addition, standardized guidelines are needed regarding 3D printing practices, AI and hardware systems, and other resources to improve overall accessibility to this new, emerging medical technology.