Program Development
Developing local capacity to address the neurological, psychiatric, and psychosocial problems of the postwar Somaliland population and to help victims regain their ability to be productive members of their society is crucial (
10). The fact that brain health is essential for general health underscores the absolute necessity to train physicians to become neurologists and psychiatrists in Somaliland. In addition, there is a strong economic and educational benefit from improved mental health in society (
11).
With this background, we set out to build a dual residency program in neurology and psychiatry with the University of Hargeisa in Somaliland (
12). Somaliland is a self-proclaimed state in East Africa, internationally considered as an autonomous region of Somalia. It has approximately 3.5 million people, 82% of whom live below the poverty line. Building a dual residency program in Somaliland was fraught with challenges, including geological and ethnic conflicts.
While health services are delivered by public, private, and nongovernmental organizations, there is no comprehensive database providing an accurate view of health needs or emerging diseases in the region. Although the educational institutions in Somaliland have recently expanded to provide specialty services in the areas of internal medicine and obstetrics, they have had few resources with which to recruit or train qualified brain clinicians. As a result, health care institutions have faced a shortage of providers to address the neurologic and psychiatric needs of the population. Public ministries lacked trained personnel capable of effectively designing, implementing, managing, and evaluating programs that target brain health care needs of vulnerable populations.
The Minister of Health of Somaliland, his Honor Dr. Sulaiman Essa Ahmed, as well as the government, academic, and clinical leaders in the country, outlined to our team the brain health and training needs of Somaliland, and they were iterated in the National Mental Health Policy drafted in 2012 and in the goals of the Ministry of Health. It was clear from the information transmitted to our team that the leadership in Somaliland was enlightened regarding the short- and long-term mental health needs of their population. Accordingly, and at their request and with their support, our strategic plan was developed in close partnership with our Somaliland counterparts.
These counterparts to our team included Abdi H. Gass, M.D., the president of the University of Hargeisa, and Deria Ismall Ereg, M.D., the Dean of the university’s medical school, Alima Mohamed, PhD, Director of Public Health at the University of Hargeisa, and Essa Kayd, CEO of Hargeisa Neurology Hospital, who initially sought out two members of our team (G.F., D.C.H.) at Brigham and Women’s Hospital in 2012. Our Boston-based group conducted a field study in Hargeisa by examining the mental health challenges and capacity for care for the region and meeting with key stakeholders. Following agreements between the involved institutions, a generous grant from the Al Zamil Charity Fund in 2015 enabled us to develop and establish the proposed dual residency program in psychiatry and neurology at the University of Hargeisa.
In order to develop the curriculum for this dual residency program, one of the authors of the present study (Z.C.), a neurologist-psychiatrist public health expert, was engaged by the development team and installed part-time as director of this new residency program at the University of Hargeisa. In collaboration with a public health intern (Rebecca Hock, Ph.D., from the Chester M. Pierce Division of Global Psychiatry at Massachusetts General Hospital [MGH]), we worked toward the development of that curriculum. A cognitive-behavioral therapy (CBT)-trained psychologist (Kristina Korte, Ph.D., also with the Chester M. Piece Division of Global Psychiatry at MGH) was recruited to develop a culturally sensitive training module on this psychological intervention for inclusion in this curriculum. We opted for a CBT program given its fast and practical delivery within the community and in a hospital-based setting where goals of treatment and follow-up are easily defined and targeted. In addition, one of our residents had plans to spearhead a therapy center based on cognitive-behavioral approaches in his hometown away from the capital. The faculty at the university and the residents stressed the fact that CBT is the best cultural and acceptable weighed approach
Curriculum Development and Implementation
The Somaliland Neurology and Psychiatry Residency Training curriculum was based on the progressive accomplishment of core competency training over 36 months, consisting of a carefully balanced series of rotations through clinical subspecialties of neurology and psychiatry. Throughout the 3 year-training, the innovative curriculum emphasized community-based education, rural-based education, problem-based learning, and multidisciplinary team-based learning. The program employed a philosophy of integrated, longitudinal training. This approach enabled residents not just to meet minimum requirements but rather to experience a progressive exposure to all major topics in neurology and psychiatry over the course of 3 years. The aim of the dual residency program was to produce specialists with appropriate levels of knowledge of causation, manifestation, and prognosis of neurological and psychiatric disorders. A concurrent aim was to foster among these physicians the skills needed to lead a multidisciplinary team, provide effective teaching to all categories of workers and laymen, plan and carry out research on mental health issues, and communicate effectively with other members of mental and behavioral brain health groups.
The program was conducted in primary and collaborating institutions in general health, community, inpatient, outpatient, and emergency settings (Hargeisa University Hospital, Hargeisa Neurology Hospital for neurology, St. Paul Millennial Medical College Hospital, and Amanuel Hospital and Amanuel Hospital for psychiatry, both in Addis Ababa, Ethiopia) to provide the resident the depth of experience. It was imperative that the program accessed adequate patient populations for each mode of required education and included organized clinical services in inpatient, outpatient, emergency, consultation-liaison, and child and adolescent and adult neurology and psychiatry.
Prior to entry into the program, each resident was notified in writing of the required length of education to achieve competency and credentialing in psychiatry and neurology. The required length of education for a resident could not be changed during his or her program without mutual agreement. Exceptions for a necessary break in education or the need for remedial education were explained.
In their clinical work, each resident previewed and evaluated cases independently, after which findings and impressions were reviewed with a supervising neurology and psychiatry attending or senior staff member. Patients ranged from pediatric age to older adults, although given the African population, the bulk of the patients were in the range of young to middle-aged adults, with almost equal gender distribution. Additionally, close supervision and faculty coevaluation were always required for patients at high risk of adverse clinical outcomes (e.g., status epilepticus, acute trauma, stroke, and suicidality). Invasive and interventional procedures, such as lumbar puncture or electromyography, were carried out by residents under supervision by staff members and/or clinical fellows.
All faculty at the Department of Psychiatry at St. Paul were involved with the training of residents with direct supervisory experience. The faculty consisted of African board-certified psychiatrists with a ratio of five psychiatrists to three residents. Once in Somaliland, the residents were typically supervised by two board-certified neurologists and one neurophysiologist, with a ratio of two faculty to three residents.
As residents advanced through their training program, independence and responsibility increased in accordance with individual ability. At the end of their training, residents were required to demonstrate a sound fund of knowledge about behavioral sciences and clinical neurology and psychiatry, including neuropsychopharmacology and basic psychological treatment methods. The latter included formal training in CBT. In addition to medical knowledge, they were required to demonstrate the skills, competences, and attitudes needed to manage neurological and psychiatric problems. This curriculum afforded residents the ability to recognize, assess, and manage patients with neurologic and/or psychiatric illness independently in acute emergency, inpatient, and outpatient settings. By the end of their training and on multiple occasions, they were able to assume the confident role of educators to other medical personnel and the general or lay public on neuropsychiatric and brain health issues.
This dual residency adopted the same pattern of longitudinal learning that is implemented in American residency and fellowship programs in neurology (inpatient and outpatient), emergency neurology, neurophysiology, psychiatry (inpatient and outpatient), medical psychiatry, public and community neuropsychiatry, addiction medicine, outpatient psychotherapies, and research training. The program’s overarching goals and objectives were anchored to the six core competencies modeled after those of the Accreditation Council for Graduate Medical Education (ACGME), as well as the additional competencies articulated by the ACGME Residency Review Committee (RRC) for Psychiatry and the RRC for Neurology (
13,
14). The core competencies were reviewed by the University of Hargeisa for cultural appropriateness and sensitivity. The six competencies, followed on a yearly as well as rotation basis, were patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice.
The didactic elements of the curriculum addressed general clinical psychiatry and neurology, anatomy, neurophysiology, neuropsychopharmacology, pathophysiology, neuroradiology, and CBTs. Didactic sessions took place every 2 days and were prepared by the trainee and delivered to his or her fellow residents and supervising faculty. Every 2 weeks, the residents also participated in videoconferences with faculty at MGH and Boston University School of Medicine, during which time they received and were offered presentations and were provided with supervision. The local university hospitals in Addis Ababa and Hargeisa also offered the residents a range of grand rounds and specialty rounds, as well as group supervision that the residents had to attend weekly. Residents also engaged in weekly faculty-supervised tutorials addressing neuroanatomy, neurophysiology, neuropathology, neuroradiology, pathophysiology, psychiatric semiology, and interviewing skills. On-site didactic education also was complemented by departmental grand rounds at the Boston University School of Medicine, which were made available to the Somaliland residents for viewing via Zoom.
Additionally, the residents were engaged in scholarly activities. For example, they were involved in writing a poster on tetanus that was accepted for presentation at the 30th annual meeting of the American Neuropsychiatric Association (
15), which was later expanded to a full manuscript that was published (
16). Even past the completion of their program, the graduating residents continued to be involved in the write-up of three manuscripts related to the patients’ databases, as well as a white paper submitted to the government of Somaliland addressing challenges and opportunities for implementation and highlighting the need for brain health in the country and the region.
Evaluations were completed every 3 months by the residents and faculty in Addis Ababa and Hargeisa. Evaluations were anchored to the ACGME Milestones, and the New Innovations Platform was used to complete the evaluations. Residents also rated each other on their presentations and provided evaluations of the program as a whole. A plan for addressing deficiencies in resident performance was developed, completion of which permitted advancement to the next stage of training. Periodic review of resident and program performance was conducted by one of our team members (Z.C.) during on-site visits to the program. Clinical evaluations were mandatory, and residents had to complete written and oral examinations in psychiatry. The oral examination in psychiatry was administered by another team member (G.F.). Additionally, written examinations in neurology were administered by a team member (Z.C.) and Jama Hirsi, M.D.
Ongoing evaluations of clinical competency were conducted in addition to resident evaluations and a summary of test scores, which integrated written and oral psychiatry and neurology examinations with attending supervisor evaluations. These summary evaluations were presented to and reviewed in-person by two of our team members (Z.C. and G.F.) to Professor Ereg, the Dean of the University of Hargeisa Medical School, and to the Head of Somaliland’s Board of Medical Specialties in a review session that took place in Hargeisa. Successful completion of all written and oral examinations, along with satisfactory clinical evaluations and completed case logs, was required for graduation from the training program and certification as independent practitioners in the field of neurology-psychiatry.
Special Challenges Encountered During Program Operation
Clinical training.
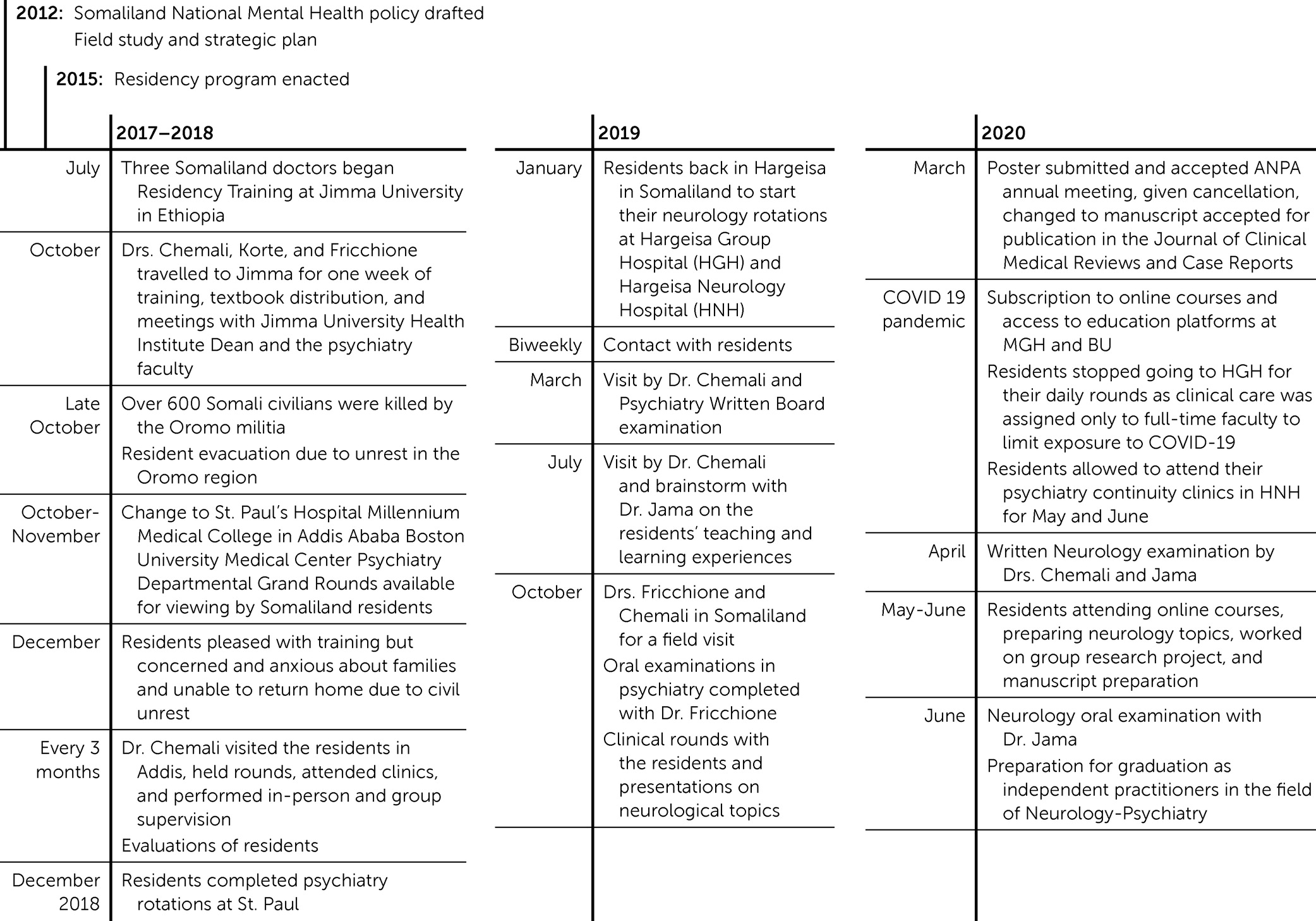
The residents started their psychiatry training at Jimma University, Southwest of Addis Ababa in Ethiopia (a timeline of the program is presented in
Figure 1). The Oromo insurrection (a long-standing conflict between the Oromo people and the Ethiopian government) necessitated moving their training to St. Paul Millennial Medical College Hospital and Amanuel Hospital in Addis Ababa, where there is a large Somali enclave. There, they completed their psychiatry rotations over an 18-month period, after which they returned to Hargeisa in Somaliland to pursue their neurology training. Their relocation presented unanticipated challenges in relation to obtaining the experiences and supervision incorporated into the original design of the clinical curriculum. In hindsight, however, they were provided with excellent educational opportunities at St. Paul Millennial Medical College Hospital and Amanuel Hospital in Addis Ababa. Indeed, the residents themselves reflected this in their correspondence about their experiences, offering their “appreciation of the support and care received and the tireless efforts to help and teach [them].” They described their clinical rotation sites as “big, busy and specialized psychiatry hospitals” where they were “attending case discussion classes and seminars, seeing patients in the outpatient offices, with intern students translating for [them]. They presented “one case in the morning report for every week.” While this change in training site was unanticipated, it ultimately proved to be a change that was not only accommodated fully by the residents and faculty but also one that appears to have afforded excellent training opportunities.
The neurology training was challenged by the scarcity of neurologists in the country (i.e., only two neurologists in Hargeisa) and by the priority given to private practice relative to teaching. A solution to this challenge was provided by Jama Hirsi, M.D., a Somalilander who had recently completed his neurology training at Addis Ababa University, who was hired to teach, supervise, and mentor the residents. When Dr. Jama became their primary mentor and educator, the residents were able to receive the supervision needed to perform and learn from their clinical work. Their experienced included overnight call for the neurology service three times per week. They maintained case logs related to clinical work they completed, which was signed by Dr. Jama monthly and sent to one of our team members (Z.C.) at MGH for review.
Our team member (Z.C.) also complemented the supervision provided by Dr. Jama by engaging in quarterly in-person visits to the training sites in Ethiopia and Somaliland. During these visits, our team member (Z.C.) participated in clinical rounds with the residents and supervised weekday presentations on a broad range of topics in neurology and psychiatry. She also provided in-person individual and group supervision to the residents.
Over the course of this period of program development and operation, it became clear that overcoming challenges to clinical training program operations required supervisory faculty needed to be on-site and for the team at MGH and Boston University School of Medicine to perform in-person visits. These visits afforded the opportunity to provide direct support to the on-site faculty in relation to both curricular implementation and resident supervision.
Didactic education.
As in any training program, organizing the didactic curriculum and securing faculty presenters of didactic content was necessary. Given the scarcity of in-country faculty, implementing the didactic curriculum proved to be a particular challenge. The U.S.-based faculty concluded that their contributing directly to the didactic curriculum was desirable and that doing so would diminish reliance on faculty-guided, but self-directed, learning (which is often the default mode of didactic instruction in low-to-middle income countries). Accordingly, our team members (Z.C. and G.F.) and Kristina Korte, Ph.D., provided on-site educational sessions during the residents’ participation in this program. Textbooks and reading materials that were secured for the residents’ use were distributed to them during these visits; additional teaching materials (e.g., articles, manuscripts) were provided by e-mail. During these visits, the U.S.-based faculty also met with the psychiatry faculty and with the Dean of Jimma University Health Institute to review progress toward achievement of the learning objectives for the residents.
The inconsistent availability of high-speed Internet service needed to support online/videoconference-based elements of the didactic program and other elements of supervision was a particularly difficult challenge to overcome. Internet access and related serves in Ethiopia are highly regulated, and governmental shutdown of services without prior notice occurs frequently and unpredictably. In that context, the speed and privacy of Internet-based communication and information transfer are also major concerns without clear solutions. Despite these challenges, however, effective Internet-based communication between residents and supervising faculty was maintained without incident or known adverse consequence to patient privacy. The more consistent availability of high-speed Internet service in Somaliland was particularly helpful toward those ends.
Evaluation.
Resident and faculty evaluations are challenging to complete in a timely manner under the best of circumstances, and this proved no less the case in this training program. During their in-person visits to the program, the U.S.-based faculty collected evaluations and reviewed them with the residents and their rotation-specific faculty members.
Political and environmental context.
Developing a residency training program in a country in the throes of postcivil-war regional conflict with no neurology and psychiatry faculty was a difficult task. Among the most difficult issues presented by this political and environmental context included securing agreement on and approval of the curriculum from all stakeholders. Additionally, negotiating a professional services agreement with Jimma University in Ethiopia, securing Ethiopian visas, and obtaining lodging for psychiatric trainees proved especially difficult, as the timing of those negotiations followed (rather than preceded) acceptance of three Somaliland physicians into the inaugural residency class.
While these challenges were successfully addressed, as noted above, the residents were subject to evacuation from Jimma University by the Ethiopian government shortly after beginning their training because of unrest in the Oromo region (which led to casualties among ethnic Somalis in the region). Throughout their training, and despite great involvement and commitment to their education, the residents remained concerned and anxious about their families in Hargeisa, to which returning was not an option for them given the civil unrest there. This challenge was addressed through support from faculty during the period of their displacement and, more definitively, by their return to Somaliland in 2019, where they began their neurology rotations at Hargeisa Group Hospital and Hargeisa Neurology Hospital.
A subsequent contextual challenge was introduced by the COVID-19 pandemic on the African continent in mid-April of 2020. While the didactic curriculum remained available to the residents through virtual learning (including subscription to online courses and the provision of access to educational platforms at MGH and Boston University School of Medicine), the clinical curriculum was interrupted (as it was elsewhere) by contact precautions aimed at reducing the risk of infection with the SARS-CoV-2 virus. By order of the president of the University of Hargeisa, the program’s residents were not permitted to work at Hargeisa Group Hospital. This loss of training opportunity was accommodated by relocating the residents to Hargeisa Neurology Hospital, where they participated in clinics and also provided psychiatric services. Their time was also reallocated to scholarly projects during this period of their training, during which they participated in a group research project focused on mapping psychiatry and neurology databases and preparing a policy paper.