The use of contingent skin shock to treat severe behavior problems was first described by Lovass and colleagues in 1965 (
3). Although exceptionally controversial then and now, the procedure has nevertheless been shown to be effective in decreasing the rates of severe problem behaviors in many cases (
4,
5), and the effects have been immediate and durable, lasting weeks, months, years, or permanently (
6–
8). In many cases, positive effects have outweighed adverse effects by a wide margin (
9,
10). Contingent skin shock has been used to treat a range of problem behaviors, such as inappropriate sexual behavior after brain injury (
11), aggression (
12), self-injury (
13), and trichotillomania (
14).
The controversy concerning skin shock has played out in the research literature (
15), legislative hearings (
16), courtrooms (
17), and news media (
18), as well as at a National Institutes of Health consensus development conference (
19,
20) and other professional conferences (
21). Most recently, the U.S. Food and Drug Administration (FDA) issued a ban on all electrical stimulation devices (
22). This ban potentially affected patients at the Judge Rotenberg Center (JRC), where a specialized electrical stimulation device called the graduated electronic decelerator (GED) has been used to manage extremely violent and self-injurious behavior among individuals with intellectual disabilities. However, the ban was never implemented because the JRC and JRC Parents Association petitioned and received a stay of action from the FDA pending an appeal of the ban with the U.S. Court of Appeals for the District of Columbia (
23). The ban was subsequently vacated by the court. A request by the FDA for a rehearing,
en banc, was denied.
Treatment-refractory behavior disorders are serious conditions that profoundly affect patients and their families. Banning a treatment implies that the risks outweigh the benefits in all cases. Here, we describe the effect of adding contingent skin shock to a comprehensive behavioral program to address treatment-refractory self-injurious, assaultive, and destructive behaviors by a woman with autism spectrum disorder and intellectual disability. The results are discussed in the context of ethics, individualized treatment, and the FDA ban on electrical stimulation devices. This report received research approval from the Massachusetts Department of Developmental Services Research Review Committee, and the patient’s guardians provided written informed consent.
Case Report
“Ms. A” is a 26-year-old woman with autism spectrum disorder (level 3) and moderate intellectual disability who was admitted to the JRC in 2010 with chronic and intractable self-injury (causing concussions, lacerations, and callousing) and aggression that resulted in 340 staff injuries and 5,354 restraint episodes over a period of 98 months. The patient followed verbal instructions, made requests through single words or brief phrases, and uttered scripted speech from Disney movies (especially prior to and during problem behaviors). Her speech was characterized by stereotyped phrases with irregular intonation. In addition, she wore noise-canceling headphones.
When she was 2 years old, she received early-intervention services to address delays in expressive language. Subsequently, she received treatment through special education settings until she entered a day-treatment program at age 8, and at the age of 11, she entered her first residential program. She required hospitalization on numerous occasions during this period before entering the JRC facility in 2010, at which time no other residential program was willing to admit her because of the severity of her problem behaviors.
Over the course of her treatment history, Ms. A received trials of many psychotropic drugs representing different medication classes. These pharmaceuticals were prescribed and managed by licensed practitioners with expertise in psychopharmacology and the ability to monitor dosages, durations, efficacy, adverse reactions, and drug-drug interactions. These medications included quetiapine, ziprasidone, olanzapine, risperidone, aripiprazole, valproic acid, oxcarbazepine, carbamazepine, amphetamine and dextroamphetamine, methylphenidate, clonidine, guanfacine, fluoxetine, citalopram, fluvoxamine, buspirone, naltrexone, alprazolam, and lorazepam (
Table 1). In 2011, the administration of psychopharmacological medications was discontinued, because it was concluded that they were ineffective and potentially contributing to her behavioral disorder. In 2014, her parents sought and received independent psychological and medical evaluations for her through a respected teaching hospital (the JRC team did not refer her or know the evaluators). The data from the medical evaluation did not result in recommendations for further pharmacological interventions. The psychological evaluation data (and other testing data) are presented in
Table 2. Overall, Ms. A completed academic tasks at the early elementary school level, with strengths in the areas of spelling and word identification.
To protect the patient from self-harm, a range of protective equipment was used, including protective gloves to prevent harm to the hands associated with biting; a helmet with face shield to prevent her from biting herself as well as others; and a mechanical restraint chair to facilitate restraint, because she would otherwise overpower those attempting to restrain her and because she banged her head while in supine restraint position. Staff members assigned to work with her wore helmets and arm guards to reduce their risk of injury from bites and head butts. Additionally, the areas surrounding her bed, work, and recreational locations were heavily padded to reduce the possibility of injury.
She was treated with a wide range of behavioral procedures on the basis of information from an ongoing functional assessment, including retrospective video monitoring of problem-behavior episodes and analog functional analysis with contrived conditions (this analysis suggested multiple controlling factors). Her self-injury had multiple maintaining variables, including automatic or unknown factors and escape. Any attempt of the staff to interfere with her self-injury evoked aggressive behaviors.
A range of differential reinforcement procedures were utilized, including differential reinforcement of other behavior, differential reinforcement of alternative behavior, and differential reinforcement of incompatible behavior. Ms. A was able to earn various rewards, such as access to movies, music, various food items, breaks, and Disney and Hello Kitty toys. She was able to refuse or postpone tasks through functional communication, access attention upon request, and earn or request various tangible items. To control striking behaviors, she was taught a behavior that was incompatible with striking; that is, she was required to rest her hands in a “hand holster.” When her hands entered the holsters, her fingers activated a microswitch, causing mounted green light-emitting diode (LED) lights to illuminate, and reinforcement ensued (e.g., access to Disney movies). If she removed her hands from the holster, the LED light color changed to red, a tone sounded, and reinforcement ceased. She practiced these sessions once a day and was asked to engage in a session contingent on certain identified antecedent behaviors. A total of 329 permutations of behavioral interventions (e.g., reinforcement, extinction, satiation, and response blocking) were implemented over the course of 9 years, resulting in modest reductions in problem behaviors. Such procedures continued after the GED intervention was introduced.
Contingent skin shock was administered via a GED that delivered an average direct current of 15 mA root mean square (RMS) at 60 V
RMS when applied to a 4-kΩ resistor. The stimulus was a 2-second train of square waves with a 25% duty cycle (meaning the current was on for 0.5 seconds during the 2-second application). The cycle consisted of 3-ms pulses (with the current on) at a rate of 80 pulses per second, followed by 9 ms of no current. A complete description of the battery, remote, and electrode was presented in a previous study by Israel et al. (
12). It is important to emphasize that GED output is direct current as opposed to alternating current. Direct current is much safer than an equivalent level of alternating current. The 0.45‐joule energy delivered by the GED per application is far less than that of other electrical stimulation devices, such as electroconvulsive therapy devices that deliver up to 100 joules, defibrillators that deliver up to 269 joules, and electronic control weapons that deliver up to 50 joules (
4). A physician specializing in electrical safety who evaluated and experienced the GED found “the brief exposure to be moderately painful and to only last as long as the exposure. There was no pain or abnormal sensation after the exposure ended” (J Miner, unpublished GED safety report, October 29, 2009). In the same report, one of two naive recipients (the second author, M.C.) described the experience to be “unpleasant but brief, surprising, distinctly different than pain experience from tissue damage, with no residual discomfort.” Clinical staff at the JRC facility administered hundreds of skin shock stimulations to themselves when demonstrating the GED to families, professionals, and regulators.
Prior to initiation of the GED intervention for Ms. A, her parents provided written informed consent that could be revoked at any time. The clinician who directed and composed her program that integrated use of the GED was a psychologist and Board Certified Behavior Analyst–Doctoral. The patient’s physician certified the absence of medical contraindications for the use of the GED. An internal peer review committee reviewed her treatment plan and deemed it appropriate, and a human rights committee approved the plan as well. In addition, a Massachusetts probate court judge authorized the treatment plan through a “substituted judgment” petition in an individual court hearing in which Ms. A was represented by her own court-appointed attorney. This attorney retained his own independent psychologist to provide advice concerning the proposed treatment plan. Reports on her treatment status were submitted to the probate court every 3 months, and the judge held a formal review at a minimum of once a year.
With the introduction of the GED, the patient’s aforementioned positive reinforcement procedures remained in place. Behavioral topographies were defined as follows: aggressive behavior (hitting, kicking, punching, slapping, grabbing, head butting, biting, scratching, and pinching), destructive behavior (throwing objects, tearing and ripping items, and breaking and kicking objects), health-dangerous behavior (head banging, biting herself, hitting herself, and striking her head with her feet), major disruptive behavior (screaming and yelling), and noncompliant behavior (attempting to remove the device and removing her hands from an activated holster). When she engaged in a behavior within a topography, she received one GED application and was required to complete a 5-minute hand-holster session. Remarkably, all restraint and protective equipment were rendered unnecessary within 24 hours of initiating treatment with the GED.
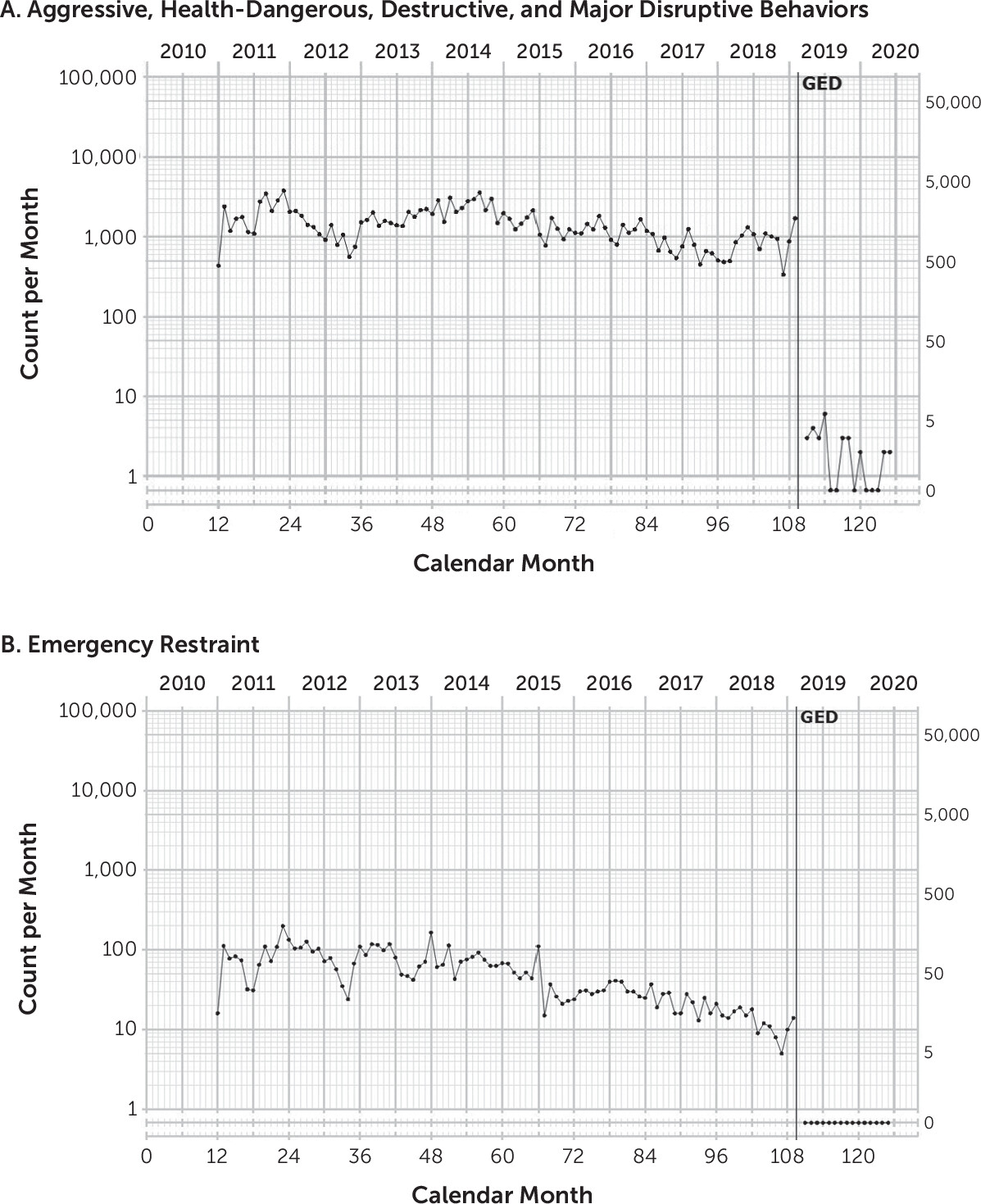
Figure 1A shows the effect of adding the GED intervention as a consequence for Ms. A’s aggressive, health-dangerous, destructive, and major disruptive behaviors. In the 98 months prior to the introduction of this intervention, she exhibited these behaviors at a mean monthly rate of 1,476.09. In the 16 months after the GED intervention was introduced, the mean monthly frequency decreased to 1.87 per month.
Figure 1B shows the monthly frequency of emergency physical restraints before and after the introduction of the GED intervention. Although some deceleration in restraint frequency was observed prior to introduction of the GED, this intervention immediately and completely eliminated the need for emergency restraint.
Discussion
For over a decade, well-meaning professionals and caregivers attempted a range of behavioral, pharmacological, and other interventions to address Ms. A’s severe problem behaviors without success. She injured herself and her caregivers, she needed to wear a protective helmet, and she was restrained more than 5,000 times. Her problem behaviors necessitated leaving her family home at 11 years of age, and the behaviors continued to interfere with every aspect of her life. The introduction of the GED intervention immediately and nearly completely eliminated her severe behavior problems that were refractory to all previous treatments.
The cessation of problem behaviors dramatically improved Ms. A’s quality of life. She began attending field trips on a weekly basis. She was able to go on frequent visits with her parents to parades and the family vacation home, as well as to visit relatives. Signs of self-injury, such as callouses on her hands from biting herself, disappeared, and there have been no self-injury events since initiating the GED intervention. All protective padding in her living and work areas was removed. Ms. A is now more engaging and responsive to others, and she can tolerate normal and inevitable delays to reinforcement, schedule changes, and other unpredictable variations in her environment and in social interactions.
The results for Ms. A are similar to those reported by various investigators who have implemented the use of electrical stimulation devices similar to the GED (
3–
15). The effect of significantly reducing or eliminating previously intractable self-injury, aggression, or other behaviors and improving quality of life has been replicated hundreds of times through various single-subject research designs. Despite such evidence, divisions remain among treatment providers on whether treatment with electrical stimulation devices should be available. Similar controversy exists within the public sphere. Although the divisions may never be completely bridged, community and provider education, conscientious decision making, transparency in administration, rigorous individual ethical safeguards, and continued scientific investigation may help to preserve an individual’s right to effective treatment.